Prevalence and Factors Associated with Post-operative Strictures in Anorectal Malformations
DOI:
https://doi.org/10.33192/smj.v75i7.262816Keywords:
Stricture, stenosis, complication, anorectal malformation, ARMAbstract
Objective: Rectal strictures are a serious complication following operation for anorectal malformations (ARM). The purpose of this study was to determine the factors affecting rectal strictures following surgical treatments for ARM.
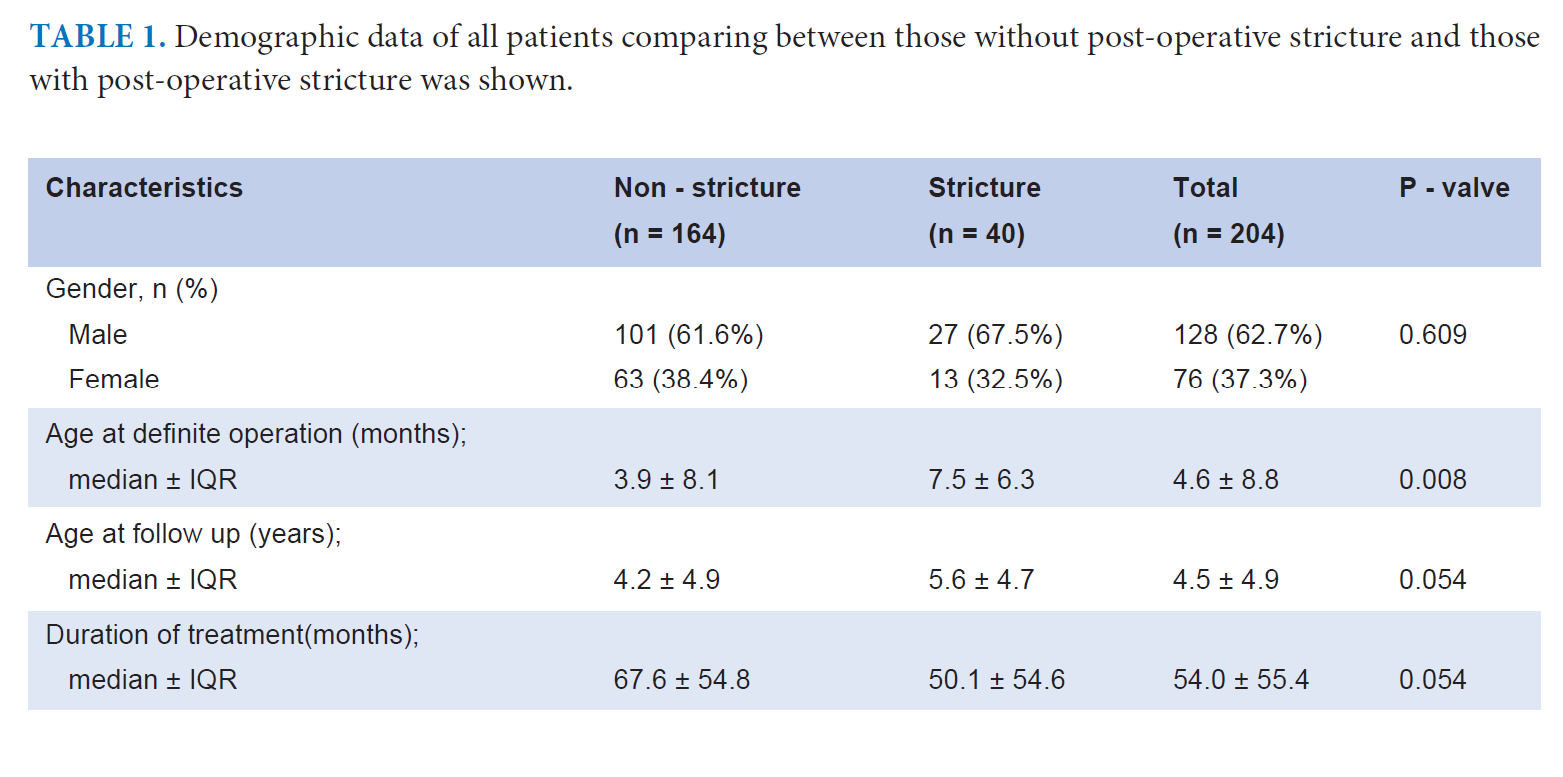
Materials and Methods: Retrospective chart reviews of 204 patients with ARM who underwent surgical treatment at Siriraj Hospital between January 2003 and December 2019 were carried out.
Results: Overall, the prevalence of post-operative rectal stricture was 19.6% (40/204). The higher types of ARM had higher rectal stricture rates. In low type ARM, the stricture rate following surgery for perineal fistula, vestibular fistula was 4.1% and 14.7%, respectively. Recto-bulbar urethral fistula and recto-prostatic urethral fistula had stricture rates of 19.2% and 26.7%, respectively, but in higher types, the stricture rates were above 70%. Complications such as wound infection, dehiscence, retraction, colonic necrosis and recurrent fistula all affected the post-operative stricture rate (p = 0.029, p = 0.01, p = 0.01, p = 0.042 and p = 0.002, respectively). The operation for low type ARM using local tissue flap, such as YV and cutback anoplasty, had low complications. More complicated operations were performed for higher type ARM. The higher the complication rate, the higher the post-operative rectal stricture. Routine rectal dilatation by parents seemed to prevent rectal strictures (p = 0.056). The surgical treatments for rectal strictures composed of 57.5% anoplasty, 17.5% PSARP, 15% abdo-assisted pull-through and 10% abdo-assisted PSARP.
Conclusion: Post-operative rectal stricture occurred because of complications following complicated operations for high type ARM. A meticulous operative technique is crucial.
References
Peña A, Hong AR, Midulla P, Levitt M. Reoperative surgery for anorectal anomalies. Semin Pediatr Surg 2003;12(2):118-23.
Jenetzky E, Reckin S, Schmiedeke E, Schmidt D, Schwarzer N, Grasshoff-Derr S, et al. Practice of dilatation after surgical correction in anorectal malformations. Pediatr Surg Int 2012:28:1095-9.
Peña A, Grasshoff S, Levitt A. Reoperations for anorectal malformations. J Pediatr Surg 2007;42:318-25.
Holbrook C, Misra D, Zaparackaite I, Cleeve S. Post-operative strictures in anorectal malformation: trends over 15 years. Pediatr Surg Int 2017;33:869-73.
Potts WJ, Riker WL, Deboer A. Imperforate anus with recto-vesical, -urethral-vaginal and -perineal fistula. Ann Surg 1954;140(3):381-95.
deVries P, Peña A. Posterior sagittal anorectoplasty. J Pediatr Surg 1982;17:638-43.
Peña A, deVries P. Posterior sagittal anorectoplasty: Important technical considerations and new applications. J Pediatr Surg 1982;17:796-881.
Levitt MA, Peña A. Imperforate anus and cloacal malformations. In: Holcomb III GW, Murphy JA. ed. Ashcraft’s Pediatric Surgery, 5th edition, Philadelphia: Saunders Elsevier; 2010:468-90.
Ruangtrakool R, Sirianant P. Surgical complications and functional outcomes in children with anorectal malformations with vestibular fistula. J Med Assoc Thai 2022,105(3):240-6.
Lohsiriwat V, Jaturanon P. Effect of intraoperative hypothermia on surgical outcomes after colorectal surgery within an Enhanced Recovery after Surgery Pathway. Siriraj Med J 2019;71(1):52-8.
Liem NT, Quynh TA. One stage operation through modified posterior sagittal approach preserving the sphincter intact for anal agenesis with rectovestibular fistula. J Pediatr Surg 2015;50:634-7.
Temple SJ, Shawyer A, Langer JC. Is daily dilatation by parents necessary after surgery for Hirschsprung’s disease and anorectal malformations? J Pediatr Surg 2012;47:209-12.
Katdare MV, Ricciardi R. Anal Stenosis. Surg Clin N Am 2010;90:137-45
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














