Increased Serum Neutrophil Lymphocyte Ratio Raises the Risk for Peripheral Diabetic Neuropathy in Type 2 Diabetes Mellitus Patients
DOI:
https://doi.org/10.33192/smj.v75i9.263372Keywords:
diabetes mellitus, neutrophil-lymphocyte ratio, peripheral diabetic neuropathy, risk factorsAbstract
Objective: Peripheral diabetic neuropathy (PDN) is among the most prevalent diabetes mellitus (DM) sequelae. PDN is a severe health issue that represents a huge social and economic burden worldwide, is associated with long-term morbidity, and diminishes the quality of life of those affected. The neutrophil-lymphocyte ratio (NLR) is a mixture of the two primary components of chronic inflammatory diseases (high neutrophils and low lymphocytes) that contribute to the production of PDN. This study aimed to demonstrate high serum NRL levels enhance the risk of PDN in type 2 DM patients.
Materials and Methods: This study employed a case-control design, collecting data from the registers and outpatient medical records of Prof. Dr. IGNG Ngoerah General Hospital type 2 DM patients who satisfied the inclusion and exclusion criteria between January 2018 and December 2019. Based on clinical neuropathy and abnormal electrodiagnostic testing, the PDN diagnosis was established. Serum NLR was collected from laboratory tests recorded by a computer.
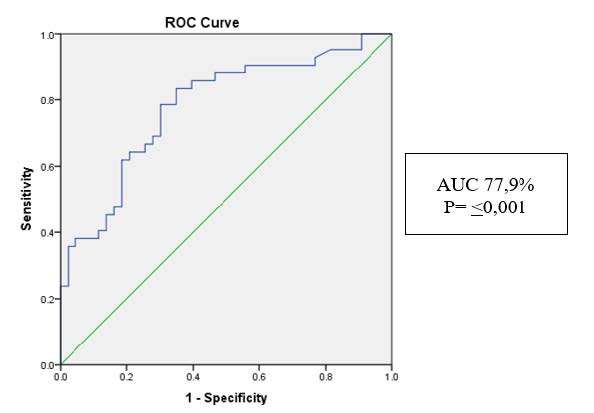
Results: The Receiver Operating Characteristic (ROC) curve approach determined the NLR cut-off value of 2.18. High NLR substantially increased the incidence of PDN (OR 10.36; 95% CI 3.69-29.07; p<0.001). Other characteristics evaluated, including duration of diabetes, usage of anti-diabetic medications, uncontrolled diabetes, obesity, hypertension, and dyslipidemia, were not significantly associated with the incidence of PDN. High serum NLR was an independent risk factor for PDN in type 2 DM patients (adjusted OR=10.36; 95% CI: 3.57-29.07; p<0.001).
Conclusion: Based on the findings of this investigation, it was determined that elevated serum NLR increases the risk of PDN events in patients with type 2 DM.
References
Karuranga, Joao da Rocha Fernandes, Yadi Huang. Eighth edition 2017. IDF Diabetes Atlas, 8th edition. 2017.1-150 p.
Rajchgot T, Thomas SC, Wang J-C, Ahmadi M, Balood M, Crosson T, et al. Neurons and Microglia; A Sickly-Sweet Duo in Diabetic Pain Neuropathy. Front Neurosci. 2019;13:25.
Hicks CW, Selvin E. Epidemiology of Peripheral Neuropathy and Lower Extremity Disease in Diabetes. Curr Diab Rep. 2019;19(10):86.
Gow D, Moore P. Assessing diabetic peripheral neuropathy in primary care. Best Pract J. 2014;(61):36-47.
Vongsirinavarat M. Falls among Older Adults with Type 2 Diabetes Mellitus with Peripheral Neuropathy. Siriraj Med J. 2021;72(2):92-8.
Xu T, Weng Z, Pei C, Yu S, Chen Y, Guo W, et al. The relationship between neutrophil-to-lymphocyte ratio and diabetic peripheral neuropathy in Type 2 diabetes mellitus. Medicine (Baltimore). 2017;96(45):e8289.
Tracey KJ. The inflammatory reflex. Nature. 2002;420(6917):853-9.
Mohammad WH, Ahmad AB, Al-Maghraby MH, Abdelrhman MZ, Ezzate S. Is neutrophil-lymphocyte ratio a novel biomarker for macrovascular and microvascular complications of type 2 diabetes? Egypt J Intern Med. 2019;31(1):1-7.
Karki D, Nagila A, Dhakal N, Chhetri S. Prevalence of peripheral neuropathy in diabetes mellitus and its association with therapy, ethnicity and duration of diabetes mellitus. Asian J Med Sci. 2018;10(1):72-6.
Suwannaphant K, Laohasiriwong W, Puttanapong N, Saengsuwan J, Phajan T. Association between Socioeconomic Status and Diabetes Mellitus: The National Socioeconomics Survey, 2010 and 2012. J Clin Diagn Res. 2017;11(7):LC18-LC22.
Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, et al. Prevalence of Diabetes among Men and Women in China. N Engl J Med. 2010;362(12):1090-101.
Bansal D, Gudala K, Muthyala H, Esam HP, Nayakallu R, Bhansali A. Prevalence and risk factors of development of peripheral diabetic neuropathy in type 2 diabetes mellitus in a tertiary care setting. J Diabetes Investig. 2014;5(6):714-21.
Yagihashi S, Mizukami H, Sugimoto K. Mechanism of diabetic neuropathy: Where are we now and where to go? J Diabetes Investig. 2011;2(1):18-32.
Aaberg ML, Burch DM, Hud ZR, Zacharias MP. Gender differences in the onset of diabetic neuropathy. J Diabetes Complications. 2008;22(2):83-7.
Azmiardi A, Tamtomo D, Murti B. Factors Associated with Diabetic Peripheral Neuropathy among Patients with Type 2 Diabetes Mellitus in Surakarta, Central Java. Indones J Med. 2019;4(4):300-12.
Amour AA, Chamba N, Kayandabila J, Lyaruu IA, Marieke D, Shao ER, et al. Prevalence, Patterns, and Factors Associated with Peripheral Neuropathies among Diabetic Patients at Tertiary Hospital in the Kilimanjaro Region: Descriptive Cross-Sectional Study from North-Eastern Tanzania. Int J Endocrinol. 2019;2019:1-7.
Rahimdel A, Afkhami-ardekani M, Souzani A, Modaresi M. Prevalence of Sensory Neuropathy in Type 2 Diabetic Patients in Iranian Population ( Yazd Province ). Iran J Diabetes Obes. 2009;1(1):30-5.
Liu S, Zheng H, Zhu X, Mao F, Zhang S, Shi H, et al. Neutrophil-to-lymphocyte ratio is associated with diabetic peripheral neuropathy in type 2 diabetes patients. Diabetes Res Clin Pract. 2017;130:90-7.
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














