Outcomes of Per-Oral Endoscopic Myotomy in the Treatment of Esophageal Achalasia: Over One Hundred Cases in a Single Tertiary Center
DOI:
https://doi.org/10.33192/smj.v75i9.263612Keywords:
Per-oral esophageal myotomy, POEM, achalasia, outcomes, complicationAbstract
Objective: To study the outcomes and complications of per-oral endoscopic myotomy (POEM) in patients with esophageal achalasia.
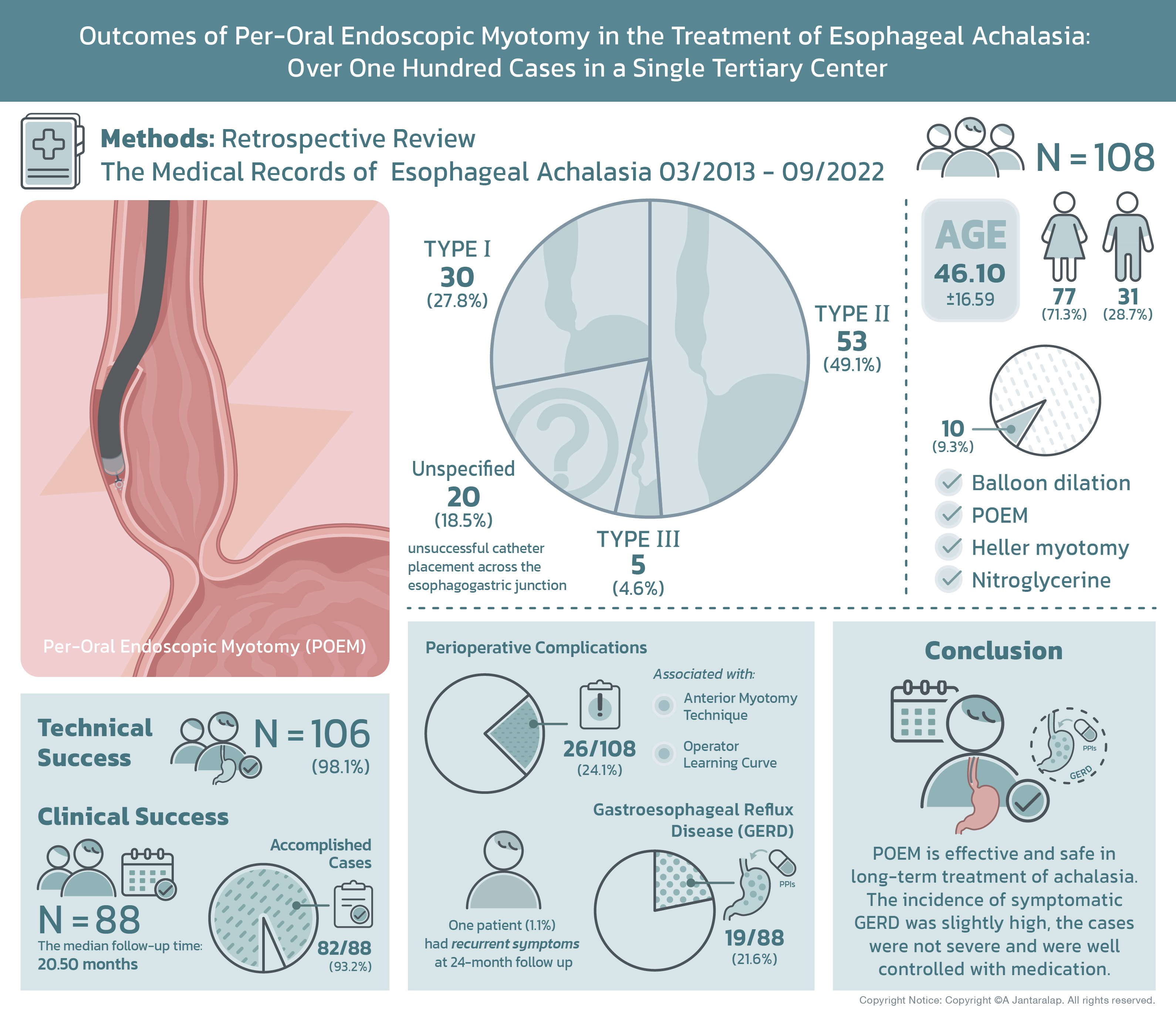
Materials and Methods: This retrospective observational study reviewed the medical records of esophageal achalasia patients who underwent POEM between March 2013 and September 2022. One hundred and eight cases were included.
Results: A total of 108 consecutive patients were included in this study and classified into 4 groups: 30 (27.8%) as type I; 53 (49.1%) as type II; 5 (4.6%) as type III; and 20 (18.5%) as unspecified due to unsuccessful catheter placement across the esophagogastric junction. The mean patient age was 46.10+16.59, 77 (71.3%) patients were female. Ten (9.3%) of the patients had undergone prior treatment, including balloon dilation, POEM, Heller myotomy, and nitroglycerine. Technical success was achieved in 106 (98.1%) cases, clinical success was evaluated only in 88 patients who follow up more than 6 month and the median follow-up time was 20.50 months (range 6-110 months). The clinical success was accomplished in 82 (93.2%), and 26 (24.1%) patients experienced perioperative complications which were significantly associated with anterior myotomy and probably operator learning curve. One patient (1.1%) had recurrent symptoms at 24-month follow up. Gastroesophageal reflux disease (GERD) was found in 19 (21.6%) patients, all of whom responded well to proton pump inhibitors (PPIs).
Conclusion: POEM is effective and safe in long-term treatment of achalasia. Although the incidence of symptomatic GERD was slightly high, the cases were not severe and were well controlled with medication.
References
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265-71.
Rai MR, Woo M, Bechara R. The Canadian POEM Experience: The first 50 patients. J Can Assoc Gastroenterol. 2020;4(3):110-4.
Campagna RAJ, Cirera A, Holmstrim AL, Triggs JR, Teitelbaum EN, Carlson DA, et al. Outcomes of 100 Patients More Than 4 Years After POEM for Achalasia. Ann Surg. 2021;273:1135-40.
Crosthwaite GL, Sejka M. Per-oral endoscopic myotomy (POEM): overview and experience of 100 cases by a single surgeon in Australia. Ann Esophagus. 2020;3:12.
Gutierrez OIB, Moran RA, Familliari P, Dbouk MH, Costamagna G, Ichkhanian Y, et al. Long-term outcomes of per-oral endoscopic myotomy in achalasia patients with a minimum follow-up of 4 years: a multicenter study. Endosc Int Open. 2020;8(5):E650-E655.
Vespa E, Pellegatta G, Chandrasekar VT, Spadaccini M, Patel H, Maselli R, et al. Long-term outcomes of peroral endoscopic myotomy for achalasia: a systematic review and meta-analysis. Endoscopy. 2023;55:167-75.
Nabi Z, Mandavdhare H, Akbar W, Talukdar R, Nageshwar R. Long-term Outcome of Peroral Endoscopic Myotomy in Esophageal Motility Disorders: A Systematic Review and Meta-analysis. J Clin Gastroenterol. 2023;57:227-38.
Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet. 2014;383:83-93.
Schima W, Stacher G, Pokieser P, Uramitsch K, Nekahm D, Schober E, et al. Esophageal motor disorders: video fluoroscopic and manometric evaluation: a prospective study in 88 symptomatic patients. Radiology. 1992;185:487-91.
Boonsomjint W, Maneerattanaporn M, Charoensak A. Correlation between Time Barium Esophagogram and the Eckardt Stage in Achalasia. Siriraj Med J. 2018;70(1):60-5.
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160-74.
Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24 Suppl 1:57-65.
Cho YK, Kim SH. Current Status of Peroral Endoscopic Myotomy. Clin Endosc. 2018;51:13-8.
Modayil R, Stavropoulos SN. POEM Contraindications and Pitfalls. In: Reavis KM. Per Oral Endoscopic Myotomy (POEM). eBook: Springer International Publishing AG; 2017. p.85-121. Doi 10.1007/978-3-319-50051-5_7.
Leung LJ, Ma GK, Lee JK, Fukami N, Chang H, Svahn J, et al. Successful Design and Implementation of a POEM Program for Achalasia in an Integrated Healthcare System. Dig Dis Sci. 2023;68(6):2276-84.
Xu MM, Kahaleh M. Recurrent symptoms after per-oral endoscopic myotomy in achalasia: Redo, dilate, or operate? A call for a tailored approach. Gastrointest Endosc. 2018;87(1): 102-3.
Callahan ZM, Su B, Ujiki M. Management of reflux after peroral endoscopic myotomy. J Xiangya Med. 2019;4(6):1-10.
Wayne WD. Biostatistics: A foundation of analysis in the health sciences. 6th ed. New York: John Wiley and Sons; 1995.
Nabi Z, Ramchandani M, Chavan R, Basha J, Reddy M, Darisetty S, et al. Double tunnel technique reduces technical failure during POEM in case with severe submucosal fibrosis. Endosc Int Open. 2021;9(9):E1335-E41.
Sanagapalli S, Roman S, Hastier A, Leong RW, Patel K, Raeburn A, et al. Achalasia diagnosed despite normal integrated relaxation pressure responds favorably to therapy. Neurogastroenterol Motil. 2019;31(6):e13586.
Hata Y, Sato H, Shimamura Y, Abe H, Shiwaku A, Shiota J, et al. Impact of peroral endoscopic myotomy on high-resolution manometry findings and their association with the procedure’s outcomes. Gastrointest Endosc. 2023;97(4):673-83.e2.
Liu ZQ, Li QL, Chen WF, Zhang XC, Wu QN, Cai MY, et al. The effect of prior treatment on clinical outcomes in patients with achalasia undergoing peroral endoscopic myotomy. Endoscopy. 2019;51(4):307-16.
Ramchandani M, Nabi Z, Reddy DN, Talele R, Darisetty S, Kotla R, et al. Outcomes of anterior myotomy versus posterior myotomy during POEM: a randomized pilot study. Endosc Int Open. 2018;6(2):E190-8.
Nabi Z, Reddy DN. Impacted of modified techniques on outcomes of peroral endoscopic myotomy: A narrative review. Frontiersin.org [Internet]. 2022, Aug, 18 [cited 2023, May,17]. Available from: doi:10.3389/fmed.2022.948299.
Khashab M, Sanaei O, Rivory J, Eleftheriadis N, Chu PWYW, Shiwaku H, et al. Peroral endoscopic myotomy: anterior versus posterior approach: a randomized single-blinded clinical trial. Gastrointest Endosc. 2020;91(2):288-97.e7.
Mohan BP, Ofosu A, Chandan S, Ramai D, Khan SR, Ponnada S, et al. Anterior versus posterior approach in peroral endoscopic myotomy (POEM): a systematic review and meta-analysis. Endoscopy. 2020;52(4):251-8.
Ichkhanian Y, Abimansour JP, Pioche M, Vosoughi K, Eleftheriadis N, Chiu PWY, et al. Outcomes of anterial versus posterior peroral endoscopic myotomy 2 years post-procedure: prospective follow-up results from a randomized clinical trial. Endoscopy. 2021;53:462-8.
Zein ME, Kumbhari V, Ngamruengphong S, Carson KA, Stein E, Tieu A, et al. Learning curve for peroral endoscopic myotomy. Endosc Int Open. 2016;4(5):E577-82.
Gonzalez JM, Meunier E, Debourdeau A, Basile P, Mouel JPL, Caillo L, et al. Training in esophageal peroral endoscopic myotomy (POEM) on an ex vivo porcine model: learning curve study and training strategy. Surg Endosc. 2023;37:2062-9.
Mota RCL, Moura EGH, Moura DTH, Bernardo WM, Moura ETH, Brunaldi VO, et al. Risk factors for gastroesophageal reflux after POEM for achalasia: a systematic review and meta-analysis. Surg Endosc. 2021;35(1):383-97.
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














