The Efficacy of Preoperative Tamsulosin on Ureteroscopy Access in Pediatrics: A Systematic Review and Meta-Analysis
DOI:
https://doi.org/10.33192/smj.v75i9.263934Keywords:
Alpha blockers, pediatric, systematic review, tamsulosin, ureteroscopyAbstract
Objective: The incidence of urolithiasis in pediatrics increases to 4-10% annually. One of the methods for treating urolithiasis is ureteroscopy (URS). The small anatomy in pediatrics often makes the initial URS unsuccessful. Alpha blockers, a drug that can relax the ureteral muscles, is a therapy that can be considered before URS is carried out. The objective of this study is to evaluate the efficacy of preoperative tamsulosin for URS access in pediatrics.
Materials and Methods: We conducted a search using four databases, including PubMed, EBSCO, Cochrane Library, and ProQuest. This study includes randomized controlled trials (RCTs), retrospective and prospective studies, which compared the efficacy of preoperative alpha blockers and placebo or non-placebo controls in pediatrics undergoing ureteroscopy. The outcome of interest was the success rate of URS access and the duration of surgery.
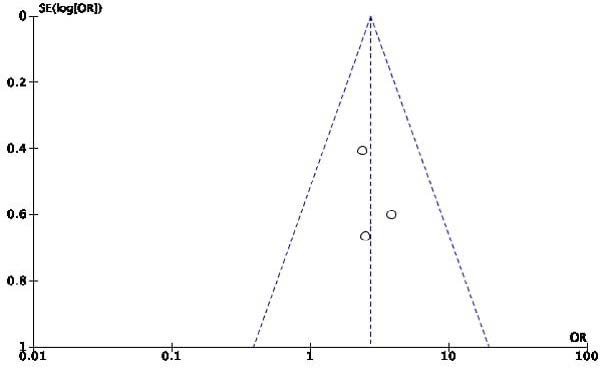
Results: A total of 120 studies were identified from a database search. There were 3 studies included in this review involving 235 patients. The meta-analysis was conducted using a random-effects model. The results of the meta-analysis showed that alpha blockers provided a successful rate of ureteroscopy access in pediatric patients (Odds ratio (OR) 2.73; 95% confidence interval (CI) 1.52 up to 4.91; p=0.0008). Duration of surgery did not show significant results (Mean difference (MD) 3.46; 95% CI -3.59 up to 10.50; p=0.34).
References
McGee LM, Sack BS, Wan J, Kraft KH. The effect of preoperative tamsulosin on ureteroscopic access in school-aged children. J Pediatr Urol. 2021;17(6):795.e1-795.e6.
Halinski A, Halinski A, Zaniew M, Kudlinski B, Soltysiak J, Sobolewski B, et al. Interest of URS-L in the treatment of ureterolithiasis in preschool children. Front Pediatr. 2019;7:324.
Khan A, Afridi AK, Khan RA, Khan, N, Nizamudin, Rashidullah M. The Effect of preoperative tamsulosin on ureteroscopic access in below 16 years children. J Saidu Med Coll Swat. 2022;12(4):150-4.
Aldaqadossi HA, Shaker H, Saifelnasr M, Gaber M. Efficacy and safety of tamsulosin as a medical expulsive therapy for stones in children. Arab J Urol. 2015;13(2):107-11.
Morley C, Hajiran A, Elbakry AA, Al-Qudah HS, Al-Omar O. Evaluation of preoperative tamsulosin role in facilitating ureteral orifice navigation for school-age pediatric ureteroscopy. Res Rep Urol. 2020;12:563-8.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89.
Lo CK-L, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14(1):45.
Paraboschi I, Gnech M, De Marco EA, Minoli DG, Bebi C, Zanetti SP, et al. Pediatric urolithiasis: current surgical strategies and future perspectives. Front Pediatr. 2022;10:886425.
Cao B, Daniel R, McGregor R, Tasian GE. Pediatric nephrolithiasis. Healthcare (Basel). 2023;11(4):552.
Straub M, Gschwend J, Zorn C. Pediatric urolithiasis: the current surgical management. Pediatr Nephrol. 2010;25(7):1239-44.
Whatley A, Jones P, Aboumarzouk O, Somani BK. Safety and efficacy of ureteroscopy and stone fragmentation for pediatric renal stones: a systematic review. Transl Androl Urol. 2019;8(Suppl 4):S442-S7.
Nerli RB, Sharma M, Gupta P, Adhikari P, Bidi S, Ghagane SC. Therapeutic ureteroscopy for urolithiasis in children younger than 60 months of age. Pediatr Surg Int. 2021;37(1):145-50.
Tan H, Li Y, Zhang X, Mao X. Pooled analysis of the efficacy and safety of adjunctive alpha-blocker therapy before ureteroscopy in the management of ureteral stones. J Int Med Res. 2020;48(6):300060520923878.
Rob S, Jones P, Pietropaolo A, Griffin S, Somani BK. Ureteroscopy for stone disease in paediatric population is safe and effective in medium-volume and high-volume centres: Evidence from a Systematic Review. Curr Urol Rep. 2017;18(12):92.
Ziaeefar P, Basiri A, Zangiabadian M, de la Rosette J, Zargar H, Taheri M, et al. Medical expulsive therapy for pediatric ureteral stones: a meta-Analysis of randomized clinical trials. J Clin Med. 2023;12(4):1410.
Yusuf M, Yogiswara N, Setiawan MR, Salsabila S, Soebadi MA, Wirjopranoto S. Preoperative alpha-blockers to facilitate ureteral access sheath (UAS) insertion: a systematic review and meta-analysis. Bali Med J. 2023;12(1):291–8.
Arrighi N, Bodei S, Zani D, Peroni A, Simeone C, Mirabella G, et al. Alpha1 Adrenoceptors in human urinary tract: expression, distribution and clinical implications. Urologia. 2007;74(2):53-60.
Soliman MG, El-Gamal O, El-Gamal S, Abdel Raheem A, Abou-Ramadan A, El-Abd A. Silodosin versus tamsulosin as medical expulsive therapy for children with lower-third ureteric stones: prospective randomized placebo-controlled study. Urol Int. 2021;105(7-8):568-73.
Michel MC, Vrydag W. Alpha1-, alpha2- and beta-adrenoceptors in the urinary bladder, urethra and prostate. Br J Pharmacol. 2006;147 Suppl 2:S88-S119.
Yu Z-W, Wang R-H, Zhang C-C, Gao J-G. The efficacy and safety of alpha-adrenergic blockers for medical expulsion therapy in patients with ureteral calculi: a meta-analysis of placebo-controlled trials. Medicine (Baltimore). 2021;100(37):e27272.
Alsaikhan B, Koziarz A, Lee JY, Pace KT. Preoperative alpha-blockers for ureteroscopy for ureteral stones: a systematic review and meta-analysis of randomized controlled trials. J Endourol. 2020;34(1):33-41.
Ahmed AF, Maarouf A, Shalaby E, Alshahrani S, El-Feky , Khaled S, et al. Semi-rigid ureteroscopy for proximal ureteral stones: does adjunctive tamsulosin therapy increase the chance of success? Urol Int. 2017;98(4):411-7.
Sesari SS, Atmoko W, Birowo P, Rasyid N. The efficacy of adjunctive alpha-blockers on ureteroscopy procedure for ureteral stones: a systematic review and meta-analysis. F1000Res. 2021;10:427.
Abdelaziz AS, Kidder AM. Tamsulosin therapy improved the outcome of ureterorenoscopy for lower ureteral stones: a prospective, randomised, controlled, clinical trial. African Journal of Urology. 2017;23:148-53.
Sun K, Zhang P, Sun Y, Wang Q, Xia Q. Meta-analysis of the efficacy and adverse drug reactions of adrenergic alpha-antagonists in treating children with ureteral calculi. Front. Pediatr. 2023;11:1098002.
Demir M, Ertas K, Aslan R, Eryilmaz R, Sevim M, Taken K. Does tamsulosin use before ureteroscopy increase the success of the operation? J Coll Physicians Surg Pak. 2022;32(2):197-201.
Whitehurst L, Pietropaolo A, Geraghty R, Kyriakides R, Somani BK. Factors affecting operative time during ureteroscopy and stone treatment and its effect on outcomes: retrospective results over 6.5 years. Ther Adv Urol. 2020;12:1756287220934403.
Katafigiotis I, Sabler IM, Heifetz EM, Isid A, Sfoungaristos S, Lorber A, et al. Factors predicting operating room time in ureteroscopy and ureterorenoscopy. Curr Urol. 2019;12(4):195-200.
Srinualnad S, Sawangchareon A, Jongjitaree K, Phinthusophon K, Taweemonkongsap T, Leewansangtong S, et al. Predictive factors of intravesical recurrence after ureteroscopy in upper urinary tract urothelial carcinoma followed by radical nephroureterectomy. Siriraj Med J. 2023;75(3):234-40.
Ito H, Kuroda S, Kawahara T, Makiyama K, Yao M, Matsuzaki J. Clinical factors prolonging the operative time of flexible ureteroscopy for renal stones: a single-center analysis. Urolithiasis. 2015;43(5):467-75.
Oofuvong M, Pattaravit N, Kanjanawanichkul O, Siripruekpong S, Nuanjun K, Suwannarat B. Are technical skills assessed using medical knowledge associated with non-technical skill knowledge in anaesthesia resident training? Siriraj Med J. 2022;74(12):844-56.
Legemate JD, Kamphuis GM, Freund JE, Baard J, Zanetti SP, Catellani M, et al. Durability of flexible ureteroscopes: A prospective evaluation of longevity, the factors that affect it, and damage mechanisms. Eur Urol Focus. 2019;5(6):1105-11.
Berardinelli F, Cindolo L, De Francesco P, Proietti S, Hennessey D, Dalpiaz O, et al. The surgical experience influences the safety of retrograde intrarenal surgery for kidney stones: a propensity score analysis. Urolithiasis. 2017;45(4):387-92.
Wolff I, Lebentrau S, Miernik A, Ecke T, Gilfrich C, Hoschke B, et al. Impact of surgeon’s experience on outcome parameters following ureterorenoscopic stone removal. Urolithiasis. 2019;47(5):473-9.
Chotikawanich E, Leewansangtong S, Liangkobkit K, Nualyong C, Srinualnad S, Chaiyaprasithi B, et al. The feasibility and outcomes of retrograde intrarenal surgery to treat staghorn renal calculi. Siriraj Med J. 2023;75(5):362-8.
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














