Validity and Reliability of a Thai Behavioral and Emotional Screening Tool for Children with Enuresis (TBEST-E)
DOI:
https://doi.org/10.33192/smj.v75i9.264058Keywords:
enuresis, neuropsychiatric, psychological, SSIPPE, ADHDAbstract
Objective: Psychological comorbidity in children with enuresis is common and its screening is recommended. A brief validated screening instrument is needed for a busy medical practice. This study focused on the development of the Thai Behavioral and Emotional Screening Tool for children with Enuresis (TBEST-E) and aimed to examine its psychometric properties.
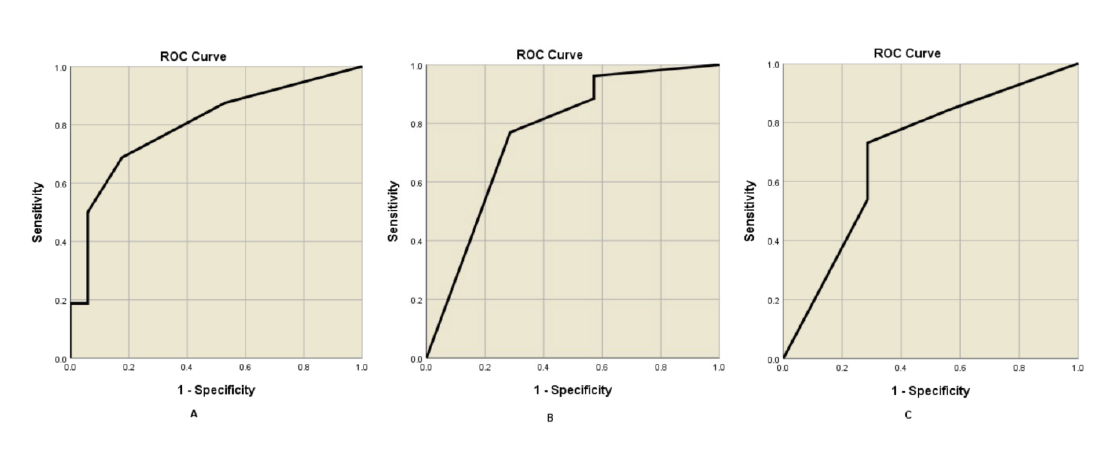
Materials and Methods: Using the Short Screening Instrument for Psychological Problems in Enuresis (SSIPPE) as a template, the 15-item with a yes/no answer format of the TBEST-E was developed for the screening of emotional problems (7 items), attention and hyperactivity/impulsivity problems (3 items each), and oppositional defiant symptoms (2 items). The parents of the children with enuresis completed the TBEST-E and the behavioral rating scale “Thai Youth Checklist” (TYC). The optimal cut-off for further assessment, the sensitivity, and the specificity the TBEST-E were identified using receiver operating characteristic (ROC) curves.
Results: After an adaptation following comments from three child psychiatrists, the TBEST-E showed a content validity of 0.9, an internal consistency of 0.71. A total of 33 children with enuresis (median age = 9, interquartile range = 6.5-11 years) were recruited. Further assessment was indicated when one of the following occurred; at least 3 emotional problems; 3 attention problems; or 2 hyperactivity/impulsivity together with 2 oppositional defiant symptoms. The overall sensitivity and specificity were 0.88 and 0.71 respectively with the accuracy of 0.84 (95% CI = 0.68-0.95).
Conclusion: The TBEST-E is time-efficient and has acceptable psychometric properties in early detection of common psychological problems in children with enuresis.
References
Bayoumi RA, Eapen V, Al-Yahyaee S, Al Barwani HS, Hill RS, Al Gazali L. The genetic basis of inherited primary nocturnal enuresis: a UAE study. J Psychosom Res. 2006;61(3):317-20.
Nevéus T, Fonseca E, Franco I, Kawauchi A, Kovacevic L, Nieuwhof-Leppink A, et al. Management and treatment of nocturnal enuresis-an updated standardization document from the International Children's Continence Society. J Pediatr Urol. 2020;16(1):10-9.
Hansakunachai T, Ruangdaraganon N, Udomsubpayakul U, Sombuntham T, Kotchabhakdi N. Epidemiology of enuresis among school-age children in Thailand. J Dev Behav Pediatr. 2005;26(5):356-60.
Tsai HL, Chang JW, Chen MH, Jeng MJ, Yang LY, Wu KG. Associations Between Psychiatric Disorders and Enuresis in Taiwanese Children: A National Population-Based Study. Clin Epidemiol. 2020;12:163-71.
von Gontard A, Baeyens D, Van Hoecke E, Warzak WJ, Bachmann C. Psychological and psychiatric issues in urinary and fecal incontinence. J Urol. 2011;185(4):1432-6.
Park S, Kim BN, Kim JW, Hong SB, Shin MS, Yoo HJ, et al. Nocturnal enuresis is associated with attention deficit hyperactivity disorder and conduct problems. Psychiatry Investig. 2013;10(3):253-8.
von Gontard A, Hussong J, Yang SS, Chase J, Franco I, Wright A. Neurodevelopmental disorders and incontinence in children and adolescents: Attention-deficit/hyperactivity disorder, autism spectrum disorder, and intellectual disability-A consensus document of the International Children's Continence Society. Neurourol Urodyn. 2022;41(1):102-14.
Lefeber TP, Nield OE, Nield LS. Psychological Aspects of Enuresis in Childhood. Annal Urol & Nephrol. 2018;1(1).
Wannapaschaiyong P, Bunman S. Nocturnal Enuresis: A Review and Focus on The Treatment Modalities of Monosymptomatic Nocturnal Enuresis. BKK Med J. 2022;18(1):56-60.
Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench. 2013;6(1):14-7.
Van Hoecke E, Baeyens D, Vanden Bossche H, Hoebeke P, Vande Walle J. Early detection of psychological problems in a population of children with enuresis: construction and validation of the Short Screening Instrument for Psychological Problems in Enuresis. J Urol. 2007;178(6):2611-5.
Vande Walle J, Rittig S, Bauer S, Eggert P, Marschall-Kehrel D, Tekgul S. Practical consensus guidelines for the management of enuresis. Eur J Pediatr. 2012;171(6):971-83.
Caldwell P, Deshpande A. Nocturnal Enuresis Resource Kit - A tool for healthcare professionals. 2 ed2017.
Vande Walle J, Rittig S, Tekgül S, Austin P, Yang SS-D, Lopez P-J, et al. Enuresis: practical guidelines for primary care. Br J Gen Pract. 2017;67(660):328-9.
Weisz JR, Suwanlert S, Chaiyasit W, Weiss B, Achenbach TM, Walter BR. Epidemiology of behavioral and emotional problems among Thai and American children: parent reports for ages 6 to 11. J Am Acad Child Adolesc Psychiatry. 1987;26(6):890-7.
Suwanlert S, Chaiyasit W. Manual for Thai Youth Checklist (TYC). 4th ed. Bangkok: Chulalongkorn University Printing House; 1999.
Amiri S, Shafiee-Kandjani AR, Naghinezhad R, Farhang S, Abdi S. Comorbid Psychiatric Disorders in Children and Adolescents with Nocturnal Enuresis. Urol J. 2017;14(1):2968-72.
Hosiri T, Sittanomai N, Bumrungtrakul T, Boonyasidhi V. Emotion Regulation and Behavioral Problems in Children with Autism Spectrum Disorder: A University Hospital Based Cross-Sectional Study. Siriraj Med J. 2023;75(3):218-23.
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














