Mobile Device Digital Photography for Teledermatology Consultation: Real-Life Situations
DOI:
https://doi.org/10.33192/smj.v75i12.264488Keywords:
Consult, Dermatology, Telemedicine, Teledermatology, SmartphoneAbstract
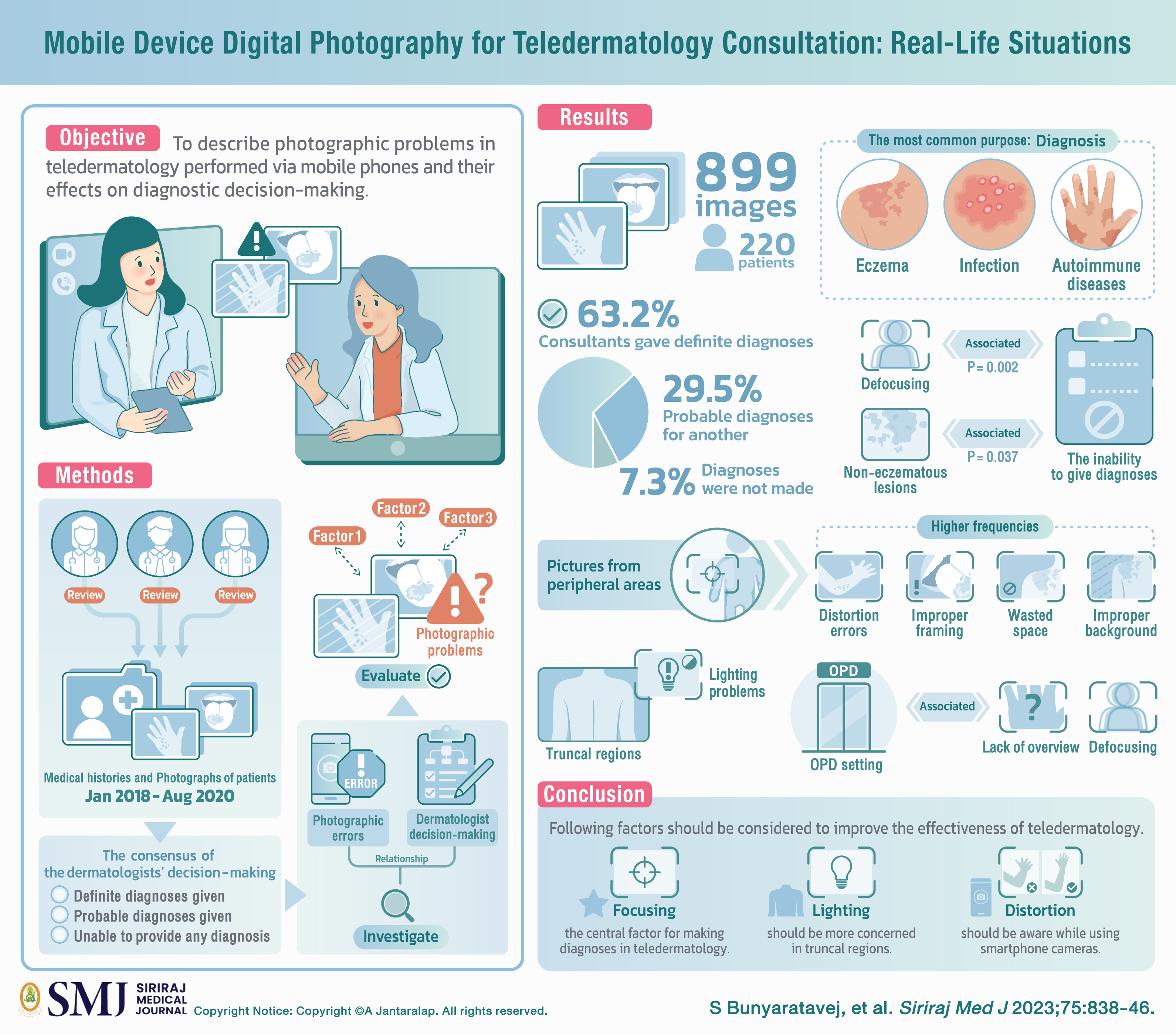
Objective: The use of mobile phones for teledermatology consultations is increasing. In this study, we aimed to describe photographic problems in teledermatology performed via mobile phones and their effects on diagnostic decision-making.
Materials and Methods: Three dermatologists independently reviewed the medical histories and photographs of patients taken by primary-care physicians for teledermatology between January 2018 and August 2020. The consensus of the dermatologists’ decision-making was categorized into “definite diagnoses given,” “probable diagnoses given,” and “unable to provide any diagnosis.” Relationships between photographic errors and dermatologist decision-making were investigated. Factors related to photographic problems were evaluated.
Results: In all, 899 images from 220 patients were reviewed. The most common purpose of teledermatology was to make a diagnosis. The most frequent diagnoses were eczema, infection, and autoimmune diseases. Consultants gave definite diagnoses for 63.2% of patients and probable diagnoses for another 29.5%. However, diagnoses were not made in 7.3% of cases. Defocusing and non-eczematous lesions were significantly associated with the inability to give diagnoses (P = 0.002 and 0.037, respectively). Pictures from peripheral areas showed higher frequencies of distortion errors, improper framing, wasted space, and improper background, while truncal regions tended to have lighting problems. The outpatient department setting was associated with a lack of overview and defocusing.
Conclusion: Focusing was the central factor for making diagnoses in teledermatology. Lighting should be more concerned in truncal regions. While using smartphone cameras, distortion should be aware. These factors should be considered to improve the effectiveness of teledermatology.
References
Sidoroff A. Chapter 2 - The Role of Clinical Photography in Dermatology. In: Hamblin MR, Avci P and Gupta GK (eds) Imaging in Dermatology. Boston: Academic Press, 2016.p.5-11.
Trettel A, Eissing L and Augustin M. Telemedicine in dermatology: findings and experiences worldwide - a systematic literature review. J Eur Acad Dermatol Venereol 2018;32:215-24.
Warshaw EM, Hillman YJ, Greer NL, Hagel EM, MacKonald R, Rutks IR, et al. Teledermatology for diagnosis and management of skin conditions: a systematic review. J Am Acad Dermatol 2011;64(4): 759-72.
Kunde L, McMeniman E and Parker M. Clinical photography in dermatology: ethical and medico-legal considerations in the age of digital and smartphone technology. Australas J Dermatol 2013;54:192-7.
Zakaria A, Maurer T, Su G, Amerson E. Impact of teledermatology on the accessibility and efficiency of dermatology care in an urban safety-net hospital: A pre-post analysis. J Am Acad Dermatol 2019;81(6):1446-52.
Paradela-De-La-Morena S, Fernandez-Torres R, Martínez-Gómez W, Fonseca-Capdevila E. Teledermatology: diagnostic reliability in 383 children. Eur J Dermatol 2015;25(6):563-9.
Weingast J, Scheibböck C, Wurm EM, Ranharter E, Porkert S, Dreiseitl S, et al. A prospective study of mobile phones for dermatology in a clinical setting. J Telemed Telecare 2013;19(4): 213-8.
Krupinski EA, LeSueur B, Ellsworth L, Levie N, Hansen R, Silvis N, et al. Diagnostic accuracy and image quality using a digital camera for teledermatology. Telemed J 1999;5(3):257-63.
Rubin CB, Kovarik CL. Teledermatologic care, the Affordable Care Act, and 20 million new patients: picturing the future. JAMA Dermatol 2014;150(3):243-4.
Marwaha SS, Fevrier H, Alexeeff S, Crowley E, Haiman M, Pham N, et al. Comparative effectiveness study of face-to-face and teledermatology workflows for diagnosing skin cancer. J Am Acad Dermatol 2019;81(5):1099-106.
Finnane A, Curiel-Lewandrowski C, Wimberley G, Caffery L, Katragadda C, Halpern A, et al. Proposed Technical Guidelines for the Acquisition of Clinical Images of Skin-Related Conditions. JAMA Dermatol 2017;153(5):453-7.
Muraco L. Improved Medical Photography: Key Tips for Creating Images of Lasting Value. JAMA Dermatol 2020;156(2):121-3.
Dermatologists BAo. UK guideance on the use of mobile photographic devices in dermatology. 2021.
Dusendang JR, Marwaha S, Alexeeff SE, Crowley E, Haiman M, Pham N, et al. Association of teledermatology workflows with standardising co-management of rashes by primary care physicians and dermatologists. J Telemed Telecare 2022;28(3):182-7.
Koh U, Betz-Stablein B, O’Hara M, Horsham C, Curiel-Lewandrowski C, Soyer HP, et al. Development of a Checklist Tool to Assess the Quality of Skin Lesion Images Acquired by Consumers Using Sequential Mobile Teledermoscopy. Dermatology 2022;238(1):27-34.
Association AT. Quick Guide to Store-Forward Teledermatology for Referring Providers. 2012.
Ashique KT, Kaliyadan F, Aurangabadkar SJ. Clinical photography in dermatology using smartphones: An overview. Indian Dermatol Online J 2015;6(3):158-63.
Kaliyadan F, Manoj J, Venkitakrishnan S, Dharmaratnam AD. Basic digital photography in dermatology. Indian J Dermatol Venereol Leprol 2008;74(5):532-6.
Quigley EA, Tokay BA, Jewell ST, Marchetti MA, Halpern AC. Technology and Technique Standards for Camera-Acquired Digital Dermatologic Images: A Systematic Review. JAMA Dermatol 2015;151(8):883-90.
Kaliyadan F, Ashique KT. Nail Photography: Tips and Tricks. J Cutan Aesthet Surg 2016;9(4): 254-7.
Kjærsgaard Andersen R, Jemec GBE. Teledermatology management of difficult-to-treat dermatoses in the Faroe Islands. Acta Dermatovenerol Alp Pannonica Adriat 2019;28(3):103-5.
Giavina-Bianchi M, Santos AP, Cordioli E. Teledermatology reduces dermatology referrals and improves access to specialists. EClinicalMedicine 2020;29-30:100641.
Cutler L, Ross K, Withers M, Chiu M, Cutler D. Teledermatology: Meeting the Need for Specialized Care in Rural Haiti. J Health Care Poor Underserved 2019;30(4):1394-406.
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














