Hepatocellular Carcinoma's Characteristics in an Endemic Country: A Closer Examination of Tumor Grade and Microvascular Invasion
DOI:
https://doi.org/10.33192/smj.v75i11.264786Keywords:
Hepatocellular carcinoma, tumor grade, microvascular invasion, IndonesiaAbstract
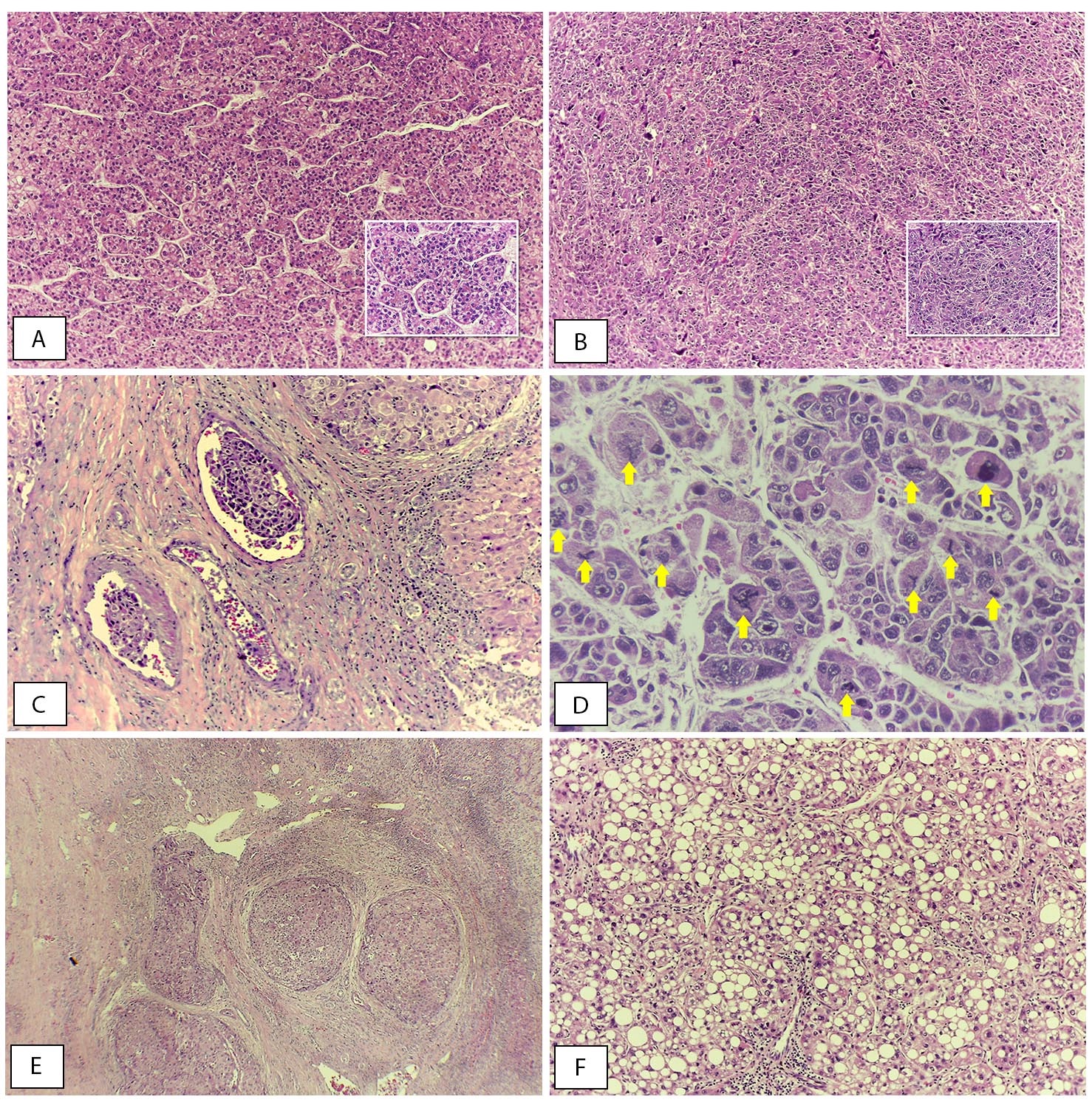
Objective: Although histological grade and microvascular invasion are known predictors for patient survival and recurrence in hepatocellular carcinoma (HCC), their relationship with various clinical and histomorphological features of HCC remains unclear.
Materials and Methods: Medical records were retrieved from 61 patients who were diagnosed with HCC from 2008-2018. Clinical and histomorphological variables that were hypothesized to be associated with histological grade and microvascular invasion were analyzed statistically using the Chi-square test or the Fisher’s exact test as alternatives. Multivariate analysis was performed with logistic regression model.
Results: The majority of the patients had well to moderately-differentiated HCC (67.2%) with some of them presenting microvascular invasion (57.4%). Alpha-fetoprotein level (AFP) ≥100 ng/ml (p=0.036), tumor size >7cm (p=0.031) and mitotic index ≥5 per 10 high power field (p=0.009) were significantly correlated with poorly-differentiated HCC. Mitotic Index ≥5 per 10 high power field was an independent factor for poorly differentiated HCC. Meanwhile BCLC stage B and mitotic index were also an independent factor for the presence of microvascular invasion.
Conclusion: Larger tumor size and higher mitotic index was significantly correlated and independent factors for poorly differentiated HCC and microvascular invasion. In biopsy specimens for which the microvascular invasion is difficult to assess, histological grade, tumor size and mitotic index may be beneficial to depict the prognosis of patients with HCC.
References
Theise ND, Curado MP, Franceschi S, et al. Hepatocellular carcinoma. In: Bosman FT, Carneiro F, Hruban RH, et al., editors. WHO Classification of Tumours of the Digestive System. 4th ed. Lyon: International Agency for Research on Cancer; 2010.p.205-16.
Zhu RX, Seto WK, Lai CL, Yuen MF. Epidemiology of Hepatocellular Carcinoma in the Asia-Pacific Region. Gut Liver. 2016;10(3):332-9. DOI: https://doi.org/10.5009/gnl15257
Rastogi A. Changing role of histopathology in the diagnosis and management of hepatocellular carcinoma. World J Gastroenterol. 2018;24(35):4000-13. DOI: https://doi.org/10.3748/wjg.v24.i35.4000
Perhimpunan Peneliti Hati Indonesia, Perhimpunan Dokter Spesialis Patologi Indonesia, Perhimpunan Dokter Spesialis Onkologi Radiasi Indonesia, et al. Konsensus Nasional Penatalaksanaan Karsinoma Sel Hati. Hasan I, Loho IM, editors. Jakarta: Perhimpunan Peneliti Hati Indonesia; 2017.p.1-77.
Loho IM, Hasan I, Rinaldi C, Dewiasty E, Gani RA. Hepatocellular carcinoma in a tertiary referral hospital in Indonesia: Lack of improvement of one-year survival rates between 1998-1999 and 2013-2014. Asian Pac J Cancer Prev. 2016;17(4):2165-70. DOI: https://doi.org/10.7314/APJCP.2016.17.4.2165
Pons F, Varela M, Llovet JM. Staging systems in hepatocellular carcinoma. HPB. 2005;7(1):35-41. DOI: https://doi.org/10.1080/13651820410024058
Mehta N, Yao FY. What Are the Optimal Liver Transplantation Criteria for Hepatocellular Carcinoma? Clin Liver Dis. 2019;13(1):20-5. DOI: https://doi.org/10.1002/cld.793
Ha SY, Choi M, Lee T, Park CK. The Prognostic Role of Mitotic Index in Hepatocellular Carcinoma Patients after Curative Hepatectomy. Cancer Res Treat. 2016;48(1):180-9. DOI: https://doi.org/10.4143/crt.2014.321
Sasaki K, Matsuda M, Ohkura Y, Kawamura Y, Inoue M, Hashimoto M, et al. In Hepatocellular Carcinomas, any Proportion of Poorly Differentiated Components is Associated with Poor Prognosis After Hepatectomy. World J Surg. 2014;38(5):1147-53. DOI: https://doi.org/10.1007/s00268-013-2374-1
El-Serag HB. Hepatocellular Carcinoma. J Clin Gastroenterol. 2002;35(5):S72-8. DOI: https://doi.org/10.1097/00004836-200211002-00002
Xiao J, Li G, Lin S, He K, Lai H, Mo X, et al. Prognostic factors of hepatocellular carcinoma patients treated by transarterial chemoembolization. Int J Clin Exp Pathol. 2014;7(3):1114-23.
Wang M, Wang Y, Feng X, Wang R, Wang Y, Zeng H, et al. Contribution of hepatitis B virus and hepatitis C virus to liver cancer in China north areas: Experience of the Chinese National Cancer Center. Int J Infect Dis. 2017;65:15-21. DOI: https://doi.org/10.1016/j.ijid.2017.09.003
Atisook K, Dechsukum C, Sthapanachai C, et al. Hepatocellular Carcinoma : Correlation of Histological Graalins with Immunohistochemical Identiffcation of Proliferative Hepatocytes with PC 10. Siriraj Hospital Gaz. 1999;51(2):71-76
Keng VW, Largaespada DA, Villanueva A. Why men are at higher risk for hepatocellular carcinoma? J Hepatol. 2012;57(2):453-4. DOI: https://doi.org/10.1016/j.jhep.2012.03.004
Qin LX, Tang ZY. The prognostic significance of clinical and pathological features in hepatocellular carcinoma. World J Gastroenterol. 2002;8(2):193-9. DOI: https://doi.org/10.3748/wjg.v8.i2.193
Han DH, Choi GH, Kim KS, Choi JS, Park YN, Kim SU, et al. Prognostic significance of the worst grade in hepatocellular carcinoma with heterogeneous histologic grades of differentiation. J Gastroenterol Hepatol. 2013;28(8):1384-90. DOI: https://doi.org/10.1111/jgh.12200
Lim KC, Chow PKH, Allen JC, Chia GS, Lim M, Cheow PC, et al. Microvascular Invasion Is a Better Predictor of Tumor Recurrence and Overall Survival Following Surgical Resection for Hepatocellular Carcinoma Compared to the Milan Criteria. Ann Surg. 2011;254(1):108-13. DOI: https://doi.org/10.1097/SLA.0b013e31821ad884
Dai CY, Lin CY, Tsai PC, Lin PY, Yeh ML, Huang CF, et al. Impact of tumor size on the prognosis of hepatocellular carcinoma in patients who underwent liver resection. J Chin Med Assoc. 2018;81(2):155-63. DOI: https://doi.org/10.1016/j.jcma.2017.06.018
Nagano Y, Shimada H, Takeda K, Ueda M, Matsuo K, Tanaka K, et al. Predictive Factors of Microvascular Invasion in Patients with Hepatocellular Carcinoma Larger Than 5 cm. World J Surg. 2008;32(10):2218-22. DOI: https://doi.org/10.1007/s00268-008-9585-x
Wang D, Luo L, Chen W, Chen LZ, Zeng WT, Li W, et al. Significance of the vascular endothelial growth factor and the macrophage migration inhibitory factor in the progression of hepatocellular carcinoma. Oncol Rep. 2014;31(3):1199-204. DOI: https://doi.org/10.3892/or.2013.2946
Pawlik TM, Delman KA, Vauthey JN, Nagorney DM, Lin Ng I, Ikai I, et al. Tumor size predicts vascular invasion and histologic grade: Implications for selection of surgical treatment for hepatocellular carcinoma. Liver Transpl. 2005;11(9):1086-92. DOI: https://doi.org/10.1002/lt.20472
Lu XY, Xi T, Lau WY, Dong H, Xian ZH, Yu H, et al. Pathobiological features of small hepatocellular carcinoma: correlation between tumor size and biological behavior. J Cancer Res Clin Oncol. 2011;137(4):567-75. DOI: https://doi.org/10.1007/s00432-010-0909-5
Osório FMF, Vidigal PVT, Ferrari TCA, Lima AS, Lauar GM, Couto CA. Histologic Grade and Mitotic Index as Predictors of Microvascular Invasion in Hepatocellular Carcinoma. Exp Clin Transplant. 2015;13(5):421-5.
Ren YJ, Huang T, Yu HL, Zhang L, He QJ, Xiong ZF, et al. Expression of β-catenin protein in hepatocellular carcinoma and its relationship with alpha-fetoprotein. J Huazhong Univ Sci Technolog Med Sci. 2016;36(6):846-51. DOI: https://doi.org/10.1007/s11596-016-1673-9
Chan MY, She WH, Dai WC, Tsang SHY, Chok KSH, Chan ACY, et al. Prognostic value of preoperative alpha-fetoprotein (AFP) level in patients receiving curative hepatectomy- an analysis of 1,182 patients in Hong Kong. Transl Gastroenterol Hepatol. 2019;4:52-64. DOI: https://doi.org/10.21037/tgh.2019.06.07
Tateishi R, Shiina S, Yoshida H, Teratni T, Obi S, Yamashiki N, et al. Prediction of recurrence of hepatocellular carcinoma after curative ablation using three tumor markers. Hepatology. 2006;44(6):1518-27. DOI: https://doi.org/10.1002/hep.21408
Huitzil-Melendez FD, Capanu M, O’Reilly EM, Duffy A, Gansukh B, Saltz LL, et al. Advanced Hepatocellular Carcinoma: Which Staging Systems Best Predict Prognosis? J Clin Oncol. 2010;28(17):2889-95. DOI: https://doi.org/10.1200/JCO.2009.25.9895
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














