The Impact of Retro-apical Urethral Dissection Approach Technique on Positive Surgical Margins in Robotic-assisted Laparoscopic Radical Prostatectomy: A Study in Thailand
DOI:
https://doi.org/10.33192/smj.v75i11.265055Keywords:
Positive surgical margins, retro-apical urethral dissection approach technique, prostate cancer, radical prostatectomyAbstract
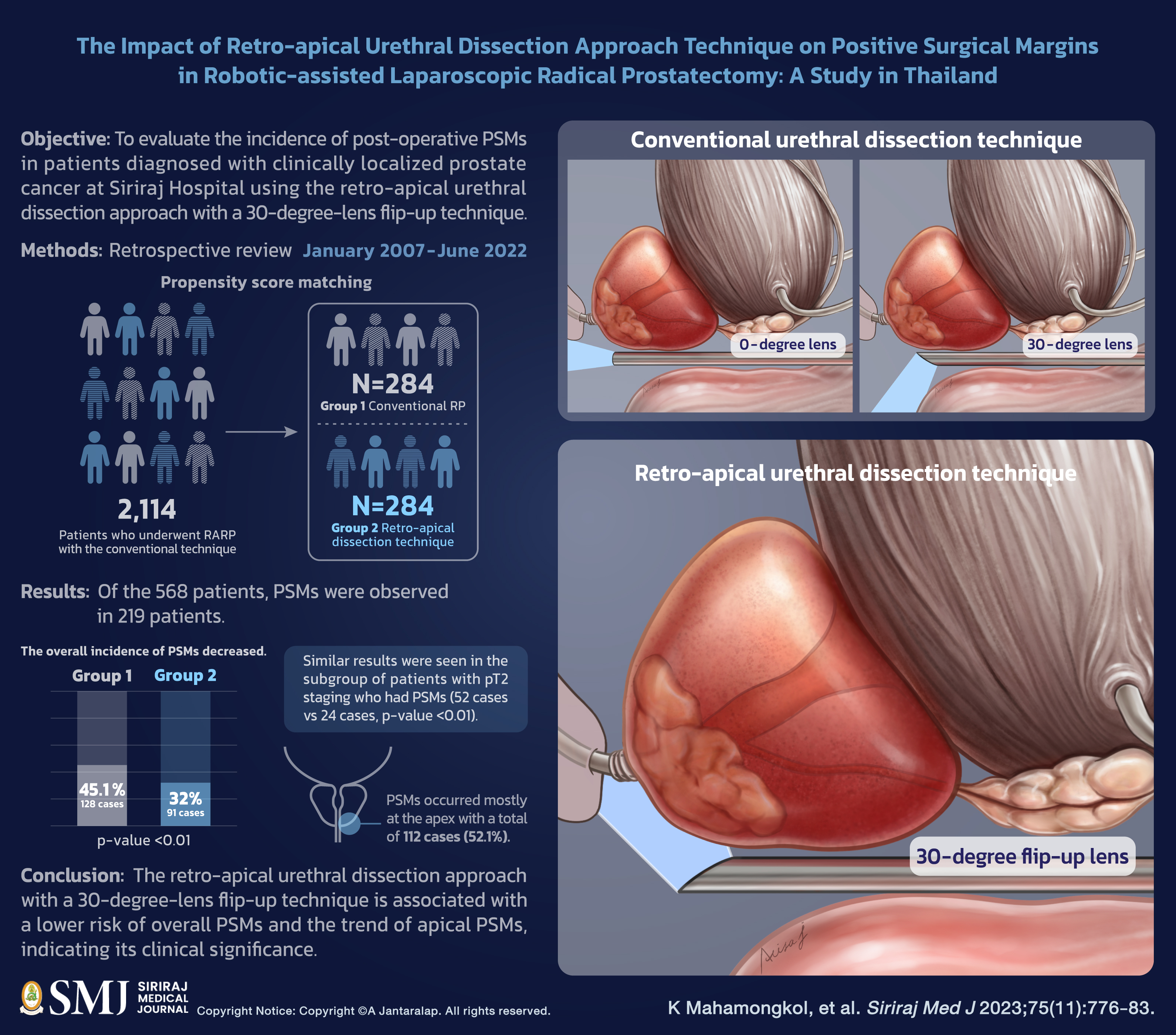
Objective: Among the various postoperative outcomes following robotic-assisted laparoscopic radical prostatectomy (RARP), positive surgical margins (PSMs) are a significant prognostic factor associated with biochemical recurrence (BCR). Many surgical techniques are available for RARP; however, the technique proposed in this study may improve surgical outcomes. This study aims to evaluate the incidence of post-operative PSMs in patients diagnosed with clinically localized prostate cancer at Siriraj Hospital using the retro-apical urethral dissection approach with a 30-degree-lens flip-up technique.
Materials and Methods: A retrospective review of 2,114 consecutive patients who underwent RARP with the conventional technique was conducted using Siriraj Hospital’s database, from January 2007 to June 2022. Propensity score matching was employed to select a group of 284 men from the total cohort of 2,114 patients who underwent conventional radical prostatectomy (Group 1) for comparison against another group of 284 patients who underwent the retro-apical dissection technique (Group 2). The incidence of PSMs was then evaluated in each group.
Results: Of the 568 patients, PSMs were observed in 219 patients. The overall incidence of PSMs decreased from 128 cases (45.1%) in Group 1 to 91 cases (32.0%) in Group 2 (p-value <0.01). Similar results were seen in the subgroup of patients with pT2 staging who had PSMs (52 cases vs 24 cases, p-value <0.01). PSMs occurred mostly at the apex with a total of 112 cases (52.1%).
Conclusion: The retro-apical urethral dissection approach with a 30-degree-lens flip-up technique is associated with a lower risk of overall PSMs and the trend of apical PSMs, indicating its clinical significance.
References
The Global Cancer Observatory. Prostate cancer fact sheet [Internet]. Lyon, France: International Agency for Research on Cancer, World Health Organization; 2020 [cited 2023 Sep 9]. Available from: https://gco.iarc.fr/today/data/factsheets/cancers/27-Prostate-fact-sheet.pdf.
National Cancer Institution of Thailand. Hospital-based cancer registry 2021 [Internet]. Bangkok, Thailand: Ministry of Public Health; 2022 [cited 2023 Sep 9]. Available from: https://www.nci.go.th/e_book/hosbased_2564/index.html.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209-49. DOI: https://doi.org/10.3322/caac.21660
Eastham JA, Auffenberg GB, Barocas DA, Chou R, Crispino T, Davis JW, et al. Clinically Localized Prostate Cancer: AUA/ASTRO Guideline, Part I: Introduction, Risk Assessment, Staging, and Risk-Based Management. J Urol. 2022;208(1):10-8. DOI: https://doi.org/10.1097/JU.0000000000002757
Eastham JA, Auffenberg GB, Barocas DA, Chou R, Crispino T, Davis JW, et al. Clinically Localized Prostate Cancer: AUA/ASTRO Guideline, Part II: Principles of Active Surveillance, Principles of Surgery, and Follow-Up. J Urol. 2022;208(1):19-25. DOI: https://doi.org/10.1097/JU.0000000000002758
Eastham JA, Auffenberg GB, Barocas DA, Chou R, Crispino T, Davis JW, et al. Clinically Localized Prostate Cancer: AUA/ASTRO Guideline. Part III: Principles of Radiation and Future Directions. J Urol. 2022;208(1):26-33. DOI: https://doi.org/10.1097/JU.0000000000002759
Tewari A, Sooriakumaran P, Bloch DA, Seshadri-Kreaden U, Hebert AE, Wiklund P. Positive surgical margin and perioperative complication rates of primary surgical treatments for prostate cancer: a systematic review and meta-analysis comparing retropubic, laparoscopic, and robotic prostatectomy. Eur Urol. 2012;62(1):1-15. DOI: https://doi.org/10.1016/j.eururo.2012.02.029
Ramirez D, Zargar H, Caputo P, Kaouk JH. Robotic-assisted laparoscopic prostatectomy: An update on functional and oncologic outcomes, techniques, and advancements in technology. J Surg Oncol. 2015;112(7):746-52. DOI: https://doi.org/10.1002/jso.24040
Pohle M, Magheli A, Fischer T, Kempkensteffen C, Busch J, Cash H, et al. The Effect of Evolving Strategies in the Surgical Management of Organ-Confined Prostate Cancer: Comparison of Data from 2005 to 2014 in a Multicenter Setting. Adv Ther. 2017;34(2):576-85. DOI: https://doi.org/10.1007/s12325-016-0469-4
Srinualnad S, Hansomwong T, Aussavavirojekul P, Saksirisampant P. Paradigm shift from open surgery to minimally invasive surgery in three approaches for radical prostatectomy: comparing outcomes and learning curves. Siriraj Med J. 2022;74(10):618-26. DOI: https://doi.org/10.33192/Smj.2022.73
Wagaskar VG, Mittal A, Sobotka S, Ratnani P, Lantz A, Falagario UG, et al. Hood Technique for Robotic Radical Prostatectomy-Preserving Periurethral Anatomical Structures in the Space of Retzius and Sparing the Pouch of Douglas, Enabling Early Return of Continence Without Compromising Surgical Margin Rates. Eur Urol. 2021;80(2):213-21. DOI: https://doi.org/10.1016/j.eururo.2020.09.044
Arroyo C, Martini A, Wang J, Tewari AK. Anatomical, surgical and technical factors influencing continence after radical prostatectomy. Ther Adv Urol. 2019;11:1756287218813787. DOI: https://doi.org/10.1177/1756287218813787
Ahlering TE, Eichel L, Edwards RA, Lee DI, Skarecky DW. Robotic radical prostatectomy: a technique to reduce pT2 positive margins. Urology. 2004;64(6):1224-8. DOI: https://doi.org/10.1016/j.urology.2004.08.021
Laven BA, Alsikafi NF, Yang XJ, Brendler CB. Minor modifications in apical dissection of radical retropubic prostatectomy in patients with clinical stage T2 prostate cancer reduce positive surgical margin incidence. Urology. 2004;63(1):95-8. DOI: https://doi.org/10.1016/j.urology.2003.08.037
Poulakis V, de Vries R, Dillenburg W, Altmansberger HM, Becht E. Laparoscopic radical prostatectomy: impact of modified apical and posterolateral dissection in reduction of positive surgical margins in patients with clinical stage T2 prostate cancer and high risk of extracapsular extension. J Endourol. 2006;20(5):332-9. DOI: https://doi.org/10.1089/end.2006.20.332
Guru KA, Perlmutter AE, Sheldon MJ, Butt ZM, Zhang S, Tan W, et al. Apical margins after robot-assisted radical prostatectomy: does technique matter? J Endourol. 2009;23(1):123-7. DOI: https://doi.org/10.1089/end.2008.0398
Namiki K, Kasraeian A, Yacoub S, Rosser CJ. Blunt apical dissection during anatomic radical retropubic prostatectomy. BMC Res Notes. 2009;2:20. DOI: https://doi.org/10.1186/1756-0500-2-20
Sasaki H, Miki J, Kimura T, Sanuki K, Miki K, Takahashi H, et al. Lateral view dissection of the prostato-urethral junction to reduce positive apical margin in laparoscopic radical prostatectomy. Int J Urol. 2009;16(8):664-9. DOI: https://doi.org/10.1111/j.1442-2042.2009.02328.x
Ou YC, Hung SW, Wang J, Yang CK, Cheng CL, Tewari AK. Retro-apical transection of the urethra during robot-assisted laparoscopic radical prostatectomy in an Asian population. BJU Int. 2012;110(2 Pt 2):E57-63. DOI: https://doi.org/10.1111/j.1464-410X.2011.10660.x
Zhang L, Wu B, Zha Z, Zhao H, Jiang Y, Yuan J. Positive surgical margin is associated with biochemical recurrence risk following radical prostatectomy: a meta-analysis from high-quality retrospective cohort studies. World J Surg Oncol. 2018;16(1):124. DOI: https://doi.org/10.1186/s12957-018-1433-3
Kim M, Yoo D, Pyo J, Cho W. Clinicopathological significances of positive surgical resection margin after radical prostatectomy for prostatic cancers: a meta-analysis. Medicina (Kaunas). 2022;58(9):1251. DOI: https://doi.org/10.3390/medicina58091251
Meeks JJ, Eastham JA. Radical prostatectomy: positive surgical margins matter. Urol Oncol. 2013;31(7):974-9. DOI: https://doi.org/10.1016/j.urolonc.2011.12.011
Eastham JA, Kuroiwa K, Ohori M, Serio AM, Gorbonos A, Maru N, et al. Prognostic significance of location of positive margins in radical prostatectomy specimens. Urology. 2007;70(5):965-9. DOI: https://doi.org/10.1016/j.urology.2007.08.040
Martini A, Gandaglia G, Fossati N, Scuderi S, Bravi CA, Mazzone E, et al. Defining Clinically Meaningful Positive Surgical Margins in Patients Undergoing Radical Prostatectomy for Localised Prostate Cancer. Eur Urol Oncol. 2021;4(1):42-8. DOI: https://doi.org/10.1016/j.euo.2019.03.006
Beckmann KR, O'Callaghan ME, Vincent AD, Moretti KL, Brook NR. Clinical outcomes for men with positive surgical margins after radical prostatectomy—results from the South Australian Prostate Cancer Clinical Outcomes Collaborative community-based registry. Asian Journal of Urology. 2022. DOI: https://doi.org/10.1016/j.ajur.2022.02.014
Kang SG, Schatloff O, Haidar AM, Samavedi S, Palmer KJ, Cheon J, et al. Overall rate, location, and predictive factors for positive surgical margins after robot-assisted laparoscopic radical prostatectomy for high-risk prostate cancer. Asian J Androl. 2016;18(1):123-8. DOI: https://doi.org/10.4103/1008-682X.148723
Matikainen MP, von Bodman CJ, Secin FP, Yunis LH, Vora K, Guillonneau B, et al. The depth of the prostatic apex is an independent predictor of positive apical margins at radical prostatectomy. BJU Int. 2010;106(5):622-6. DOI: https://doi.org/10.1111/j.1464-410X.2009.09184.x
Yao A, Iwamoto H, Masago T, Morizane S, Honda M, Sejima T, et al. The role of staging MRI in predicting apical margin positivity for robot-assisted laparoscopic radical prostatectomy. Urol Int. 2014;93(2):182-8. DOI: https://doi.org/10.1159/000358175
Coelho RF, Chauhan S, Orvieto MA, Palmer KJ, Rocco B, Patel VR. Predictive factors for positive surgical margins and their locations after robot-assisted laparoscopic radical prostatectomy. Eur Urol. 2010;57(6):1022-9. DOI: https://doi.org/10.1016/j.eururo.2010.01.040
Saksirisampant P, Nualyong C, Srinualnad S, Leewansangtong S, Taweemonkongsap T, Jitpraphai S, et al. Positive surgical margins after radical prostatectomy: Associated risk factors in Thai prostate cancer patients. J Med Assoc Thai.2020;103(5):68-74.
Hansomwong T, Saksirisampant P, Isharwal S, Aussavavirojekul P, Woranisarakul V, Jitpraphai S, et al. Role of preoperative magnetic resonance imaging on the surgical outcomes of radical prostatectomy: Does preoperative tumor recognition reduce the positive surgical margin in a specific location? Experience from a Thailand Prostate Cancer Specialized Center. Asian J Urol. [In press] 2022. doi:10.1016/j.ajur.2022.05.012 DOI: https://doi.org/10.1016/j.ajur.2022.05.012
Tewari AK, Srivastava A, Mudaliar K, Tan GY, Grover S, El Douaihy Y, et al. Anatomical retro-apical technique of synchronous (posterior and anterior) urethral transection: a novel approach for ameliorating apical margin positivity during robotic radical prostatectomy. BJU Int. 2010;106(9):1364-73. DOI: https://doi.org/10.1111/j.1464-410X.2010.09318.x
Kang SG, Shim JS, Onol F, Bhat KRS, Patel VR. Lessons learned from 12,000 robotic radical prostatectomies: Is the journey as important as the outcome? Investig Clin Urol. 2020;61(1):1-10. DOI: https://doi.org/10.4111/icu.2020.61.1.1
Koulikov D, Mohler MC, Mehedint DC, Attwood K, Wilding GE, Mohler JL. Low detectable prostate specific antigen after radical prostatectomy--treat or watch? J Urol. 2014;192(5):1390-6. DOI: https://doi.org/10.1016/j.juro.2014.05.088
Kang JJ, Reiter RE, Steinberg ML, King CR. Ultrasensitive prostate specific antigen after prostatectomy reliably identifies patients requiring postoperative radiotherapy. J Urol. 2015;193(5):1532-8. DOI: https://doi.org/10.1016/j.juro.2014.11.017
Milonas D, Venclovas Z, Sasnauskas G, Ruzgas T. The Significance of Prostate Specific Antigen Persistence in Prostate Cancer Risk Groups on Long-Term Oncological Outcomes. Cancers. 2021;13(10):2453. DOI: https://doi.org/10.3390/cancers13102453
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














