Systematic Review and Meta-Analysis on Role of Adiponectin to Leptin Ratio in Women with Polycystic Ovarian Syndrome
DOI:
https://doi.org/10.33192/smj.v75i12.265452Keywords:
Polycystic ovarian syndrome, adiponectin to leptin ratio, biomarker, adiponectin, leptinAbstract
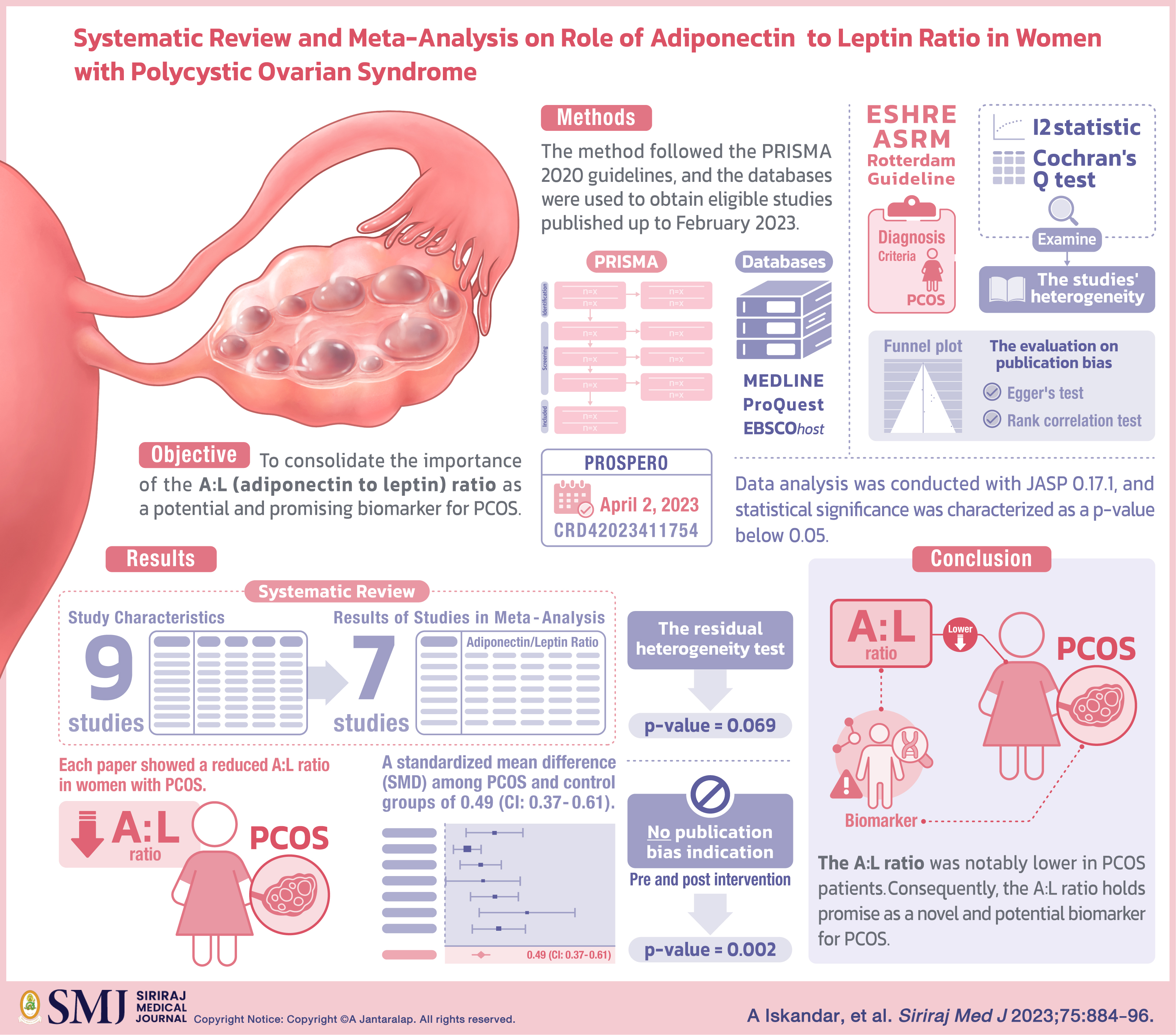
Objective: PCOS or Polycystic Ovarian Syndrome, a multifaceted disorder marked by disruptions in endocrine and metabolic processes, influences reproductive age women. The most commonly used criteria for diagnosing this condition are the Rotterdam 2003 and the National Institutes of Health Consensus 1990 guidelines. Recent studies are currently focusing on novel biomarkers, such as adiponectin and leptin to gain deeper insights on the intricate pathophysiology of PCOS. Therefore, this review aimed to consolidate the importance of the A:L (adiponectin to leptin) ratio as a potential and promising biomarker for PCOS.
Materials and Methods: The method followed the PRISMA 2020 guidelines. Furthermore, MEDLINE, Proquest, and EBSCOhost databases were used to obtain eligible studies published up to February 2023. This study was registered in PROSPERO on April 2, 2023 with registration number CRD42023411754. ESHRE/ASRM or Rotterdam Guideline was used as the diagnosis criteria for women with PCOS. To examine the studies' heterogeneity, the I2 statistic and Cochran's Q test were utilized. Meanwhile, the evaluation on publication bias visually employed a funnel plot and was confirmed through Egger's test and rank correlation test. Data analysis was conducted with JASP 0.17.1, and statistical significance was characterized as a p-value below 0.05.
Results: In the systematic review, a total of nine studies were incorporated, and seven studies were used in the subsequent meta-analysis. Each paper showcased a reduced A:L ratio in women with PCOS, with a standardized mean difference (SMD) among PCOS and control groups of 0.49 (CI: 0.37 - 0.61). The residual heterogeneity test yielded a p-value of 0.069, and no publication bias indication both pre and post intervention (p=0.002).
Conclusion: Referring to the findings, the A:L ratio was notably lower in PCOS patients. Consequently, the A:L ratio holds promise as a novel and potential biomarker for PCOS.
References
Louwers YV, Laven JSE. Characteristics of polycystic ovary syndrome throughout life. Ther Adv Reprod Health. 2020;14:2633494120911038.
Chang S, Dunaif A. Diagnosis of Polycystic Ovary Syndrome: Which Criteria to Use When? Endocrinol Metab Clin North Am. 2021;50(1):11-23.
Shi N, Ma H bo. Global trends in polycystic ovary syndrome research: A 10-year bibliometric analysis. Front Endocrinol. 2023;13:1027945.
Chen W, Pang Y. Metabolic Syndrome and PCOS: Pathogenesis and the Role of Metabolites. Metabolites. 2021;11(12):869.
Gupta V, Mishra S, Mishra S, Gupta V. L:A ratio, Insulin resistance and metabolic risk in women with polycystic ovarian syndrome. Diabetes Metab Syndr. 2017;11 Suppl 2:S697-701.
Zorena K, Jachimowicz-Duda O, Ślęzak D, Robakowska M, Mrugacz M. Adipokines and Obesity. Potential Link to Metabolic Disorders and Chronic Complications. Int J Mol Sci. 2020;21(10):3570.
Picó C, Palou M, Pomar CA, Rodríguez AM, Palou A. Leptin as a key regulator of the adipose organ. Rev Endocr Metab Disord. 2022;23(1):13-30.
Choi HM, Doss HM, Kim KS. Multifaceted Physiological Roles of Adiponectin in Inflammation and Diseases. Int J Mol Sci. 2020;21(4):1219.
Frühbeck G, Catalán V, Rodríguez A, Ramírez B, Becerril S, Salvador J, et al. Adiponectin-leptin Ratio is a Functional Biomarker of Adipose Tissue Inflammation. Nutrients. 2019;11(2):454.
Agostinis-Sobrinho C, Vicente SE de CF, Norkiene S, Rauckienė-Michaelsson A, Kievisienė J, Dubey VP, et al. Is the Leptin/Adiponectin Ratio a Better Diagnostic Biomarker for Insulin Resistance than Leptin or Adiponectin Alone in Adolescents? Child Basel Switz. 2022;9(8):1193.
Mishra P, Mittal P, Rani A, Bharti R, Agarwal V, Suri J. Adiponectin to Leptin Ratio and its Association with Insulin Resistance in Women with Polycystic Ovarian Syndrome. Indian J Endocrinol Metab. 2022;26(3):239-44.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10:89.
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19-25.
Wang F fang, Pan J xue, Wu Y, Zhu Y hang, Hardiman PJ, Qu F. American, European, and Chinese practice guidelines or consensuses of polycystic ovary syndrome: a comparative analysis. J Zhejiang Univ Sci B. 2018;19(5):354-63.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603-5.
Mamikutty R, Aly AS, Marhazlinda J. Selecting Risk of Bias Tools for Observational Studies for a Systematic Review of Anthropometric Measurements and Dental Caries among Children. Int J Environ Res Public Health. 2021;18(16):8623.
Effect Size Calculator [Internet]. [cited 2023 May 18]. Available from: https://www.campbellcollaboration.org/escalc/html/EffectSizeCalculator-Home.php
Mikolajewicz N, Komarova SV. Meta-Analytic Methodology for Basic Research: A Practical Guide. Front Physiol. 2019;10:203.
Chapter 10: Analysing data and undertaking meta-analyses [Internet]. [cited 2021 Jan 26]. Available from: /handbook/current/chapter-10
Lecke SB, Mattei F, Morsch DM, Spritzer PM. Abdominal subcutaneous fat gene expression and circulating levels of leptin and adiponectin in polycystic ovary syndrome. Fertil Steril. 2011;95(6):2044-9.
Obirikorang C, Owiredu WKBA, Adu-Afram S, Acheampong E, Asamoah EA, Antwi-Boasiakoh EK, et al. Assessing the variability and predictability of adipokines (adiponectin, leptin, resistin and their ratios) in non-obese and obese women with anovulatory polycystic ovary syndrome. BMC Res Notes. 2019;12(1):513.
Sarray S, Madan S, Saleh LR, Mahmoud N, Almawi WY. Validity of adiponectin-to-leptin and adiponectin-to-resistin ratios as predictors of polycystic ovary syndrome. Fertil Steril. 2015;104(2):460-6.
Golbahar J, Das NM, Al-Ayadhi MA, Gumaa K. Leptin-to-adiponectin, adiponectin-to-leptin ratios, and insulin are specific and sensitive markers associated with polycystic ovary syndrome: a case-control study from Bahrain. Metab Syndr Relat Disord. 2012;10(2):98-102.
Mohana CA, Hasanat MA, Rashid EU, Jahan IA, Morshed MS, Banu H, et al. Leptin and Leptin adiponectin ratio may be promising markers for polycystic ovary syndrome and cardiovascular risks: Leptin and LAR in PCOS. Bangladesh Med Res Counc Bull. 2021;47(3):266-72.
Shorakae S, Abell SK, Hiam DS, Lambert EA, Eikelis N, Jona E, et al. High-molecular-weight adiponectin is inversely associated with sympathetic activity in polycystic ovary syndrome. Fertil Steril. 2018;109(3):532-9.
Savastano S, Valentino R, Di Somma C, Orio F, Pivonello C, Passaretti F, et al. Serum 25-Hydroxyvitamin D Levels, phosphoprotein enriched in diabetes gene product (PED/PEA-15) and leptin-to-adiponectin ratio in women with PCOS. Nutr Metab. 2011;8:84.
Lin K, Sun X, Wang X, Wang H, Chen X. Circulating Adipokine Levels in Nonobese Women With Polycystic Ovary Syndrome and in Nonobese Control Women: A Systematic Review and Meta-Analysis. Front Endocrinol [Internet]. 2021 [cited 2023 May 19];11. Available from: https://www.frontiersin.org/articles/10.3389/fendo.2020.537809
Sitticharoon C, Klinjampa R, Souvannavong-Vilivong X, Chatree S, Boonpuan P, Sripong C, et al. Serum Neuropeptide Y and Leptin Levels compared between Non-pregnant and Pregnant Women in Overall, Non-obese, and Obese Subjects. Siriraj Med J. 2018;70(3):204-12.
Obradovic M, Sudar-Milovanovic E, Soskic S, Essack M, Arya S, Stewart AJ, et al. Leptin and Obesity: Role and Clinical Implication. Front Endocrinol. 2021;12:585887.
Wołodko K, Castillo-Fernandez J, Kelsey G, Galvão A. Revisiting the Impact of Local Leptin Signaling in Folliculogenesis and Oocyte Maturation in Obese Mothers. Int J Mol Sci. 2021;22(8):4270.
Seth MK, Gulati S, Gulati S, Kumar A, Rawat D, Kumari A, et al. Association of Leptin with Polycystic Ovary Syndrome: a Systematic Review and Meta-Analysis. J Obstet Gynaecol India. 2021;71(6):567.
Zheng SH, Du DF, Li XL. Leptin Levels in Women With Polycystic Ovary Syndrome: A Systematic Review and a Meta-Analysis. Reprod Sci Thousand Oaks Calif. 2017;24(5):656-70.
Childs GV, Odle AK, MacNicol MC, MacNicol AM. The Importance of Leptin to Reproduction. Endocrinology. 2020;162(2):bqaa204.
Houjeghani S, Pourghassem Gargari B, Farzadi L. Serum Leptin and Ghrelin Levels in Women with Polycystic Ovary Syndrome: Correlation with Anthropometric, Metabolic, and Endocrine Parameters. Int J Fertil Steril. 2012;6(2):117-26.
Michalakis KG, Segars JH. The role of adiponectin in reproduction: from polycystic ovary syndrome to assisted reproduction. Fertil Steril. 2010;94(6):1949-57.
Sitticharoon C, Souvannavong-Vilivong X, Klinjampa R, Churintaraphan M, Nway NC, Keadkraichaiwat I, et al. Serum Adiponectin, Visfatin, and Omentin Compared between Non-pregnant and Pregnant Women in Overall, Non-obese, and Obese subjects. Siriraj Med J. 2018;70(3):219-26.
Svendsen PF, Nilas L, Nørgaard K, Jensen JEB, Madsbad S. Obesity, body composition and metabolic disturbances in polycystic ovary syndrome. Hum Reprod Oxf Engl. 2008;23(9):2113-21.
Toulis KA, Goulis DG, Farmakiotis D, Georgopoulos NA, Katsikis I, Tarlatzis BC, et al. Adiponectin levels in women with polycystic ovary syndrome: a systematic review and a meta-analysis. Hum Reprod Update. 2009;15(3):297-307.
Frühbeck G, Catalán V, Rodríguez A, Gómez-Ambrosi J. Adiponectin-leptin ratio: A promising index to estimate adipose tissue dysfunction. Relation with obesity-associated cardiometabolic risk. Adipocyte. 2018;7(1):57-62.
Yun JE, Won S, Mok Y, Cui W, Kimm H, Jee SH. Association of the leptin to high-molecular-weight adiponectin ratio with metabolic syndrome. Endocr J. 2011;58(9):807-15.
Nahm FS. Receiver operating characteristic curve: overview and practical use for clinicians. Korean J Anesthesiol. 2022;75(1):25-36.
Hajian-Tilaki K. Receiver Operating Characteristic (ROC) Curve Analysis for Medical Diagnostic Test Evaluation. Casp J Intern Med. 2013;4(2):627-35.
Sangaraju SL, Yepez D, Grandes XA, Talanki Manjunatha R, Habib S. Cardio-Metabolic Disease and Polycystic Ovarian Syndrome (PCOS): A Narrative Review. Cureus. 2022;14(5):e25076.
Spritzer PM. Primary and secondary prevention of metabolic and cardiovascular comorbidities in women with polycystic ovary syndrome. Rev Bras Ginecol E Obstet Rev Fed Bras Soc Ginecol E Obstet. 2015;37(1):1-4.
van Doorn J, van den Bergh D, Böhm U, Dablander F, Derks K, Draws T, et al. The JASP guidelines for conducting and reporting a Bayesian analysis. Psychon Bull Rev. 2021;28(3):813-26.
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














