Comparative Study of PDA Ligation in the OR versus in the NICU: A 10-Year Retrospective Cohort Study
DOI:
https://doi.org/10.33192/smj.v76i1.266118Keywords:
Patent ductus arteriosus, Patent ductus arteriosus ligation, NICU surgery, Bedside surgeryAbstract
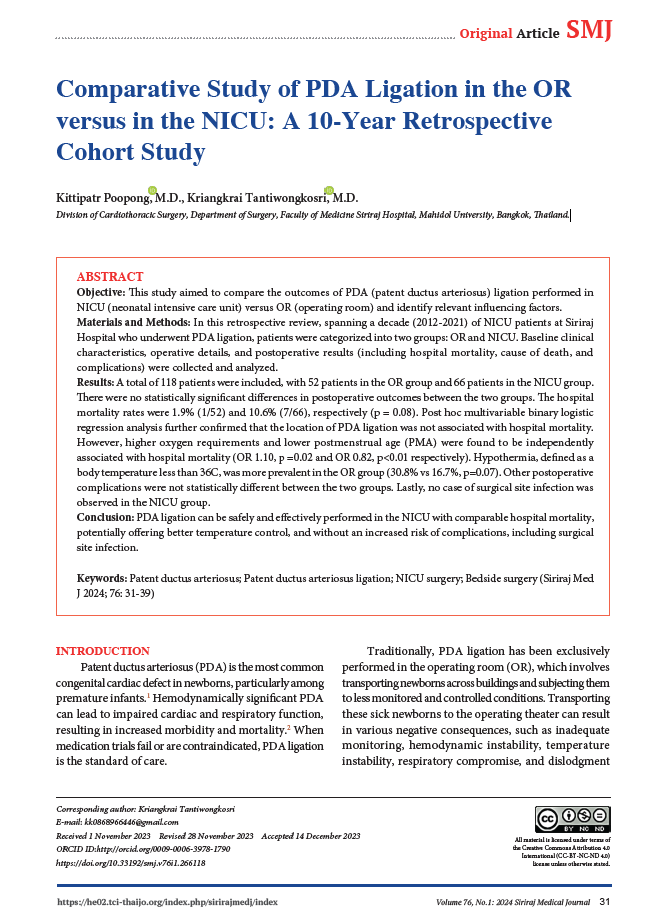
Objective: This study aimed to compare the outcomes of PDA (patent ductus arteriosus) ligation performed in NICU (neonatal intensive care unit) versus OR (operating room) and identify relevant influencing factors.
Materials and Methods: In this retrospective review, spanning a decade (2012-2021) of NICU patients at Siriraj Hospital who underwent PDA ligation, patients were categorized into two groups: OR and NICU. Baseline clinical characteristics, operative details, and postoperative results (including hospital mortality, cause of death, and complications) were collected and analyzed.
Results: A total of 118 patients were included, with 52 patients in the OR group and 66 patients in the NICU group. There were no statistically significant differences in postoperative outcomes between the two groups. The hospital mortality rates were 1.9% (1/52) and 10.6% (7/66), respectively (p = 0.08). Post hoc multivariable binary logistic regression analysis further confirmed that the location of PDA ligation was not associated with hospital mortality. However, higher oxygen requirements and lower postmenstrual age (PMA) were found to be independently associated with hospital mortality (OR 1.10, p =0.02 and OR 0.82, p<0.01 respectively). Hypothermia, defined as a body temperature less than 36C, was more prevalent in the OR group (30.8% vs 16.7%, p=0.07). Other postoperative complications were not statistically different between the two groups. Lastly, no case of surgical site infection was observed in the NICU group.
Conclusion: PDA ligation can be safely and effectively performed in the NICU with comparable hospital mortality, potentially offering better temperature control, and without an increased risk of complications, including surgical site infection.
References
Mitchell SC, Korones SB, Berendes HW. Congenital heart disease in 56,109 births: incidence and natural history. Circulation. (1971) 43:323–32.
Noori S, McCoy M, Friedlich P, Bright B, Gottipati V, Seri I, et al. Failure of ductus arteriosus closure is associated with increased mortality in preterm infants. Pediatrics. (2009) 123:e138– 44
Oxnard SC, McGough C, Jung AL, Ruttenberg HD. Ligation of the patent ductus arteriosus in the newborn intensive care unit. Ann Thorac Surg. 1977 Jun;23(6):564-7. doi: 10.1016/s0003-4975(10)63703-4. PMID: 869628.
Mohammad Saquib Mallick, Abdul Monem Jado, and Abdul Rahman Al-Bassam. Surgical procedures performed in the neonatal intensive care unit on critically ill neonates: feasibility and safety. Ann Saudi Med. 2008 Mar-Apr; 28(2): 105–108.
Lee GY, Sohn YB, Kim MJ, Jeon GW, Shim JW, Chang YS, Huh J, Kang IS, Yang JH, Jun TG, Park PW, Park WS, Lee HJ. Outcome following surgical closure of patent ductus arteriosus in very low birth weight infants in neonatal intensive care unit. Yonsei Med J. 2008 Apr 30;49(2):265-71. doi: 10.3349/ymj.2008.49.2.265. PMID: 18452264; PMCID: PMC2615315.
Ko YC, Chang CI, Chiu IS, Chen YS, Huang SC, Hsieh WS. Surgical ligation of patent ductus arteriosus in very-low-birth-weight premature infants in the neonatal intensive care unit. J Formos Med Assoc. 2009 Jan;108(1):69-71. doi: 10.1016/S0929-6646(09)60034-6. PMID: 19181610.
Avsar MK, Demir T, Celiksular C, Zeybek C. Bedside PDA ligation in premature infants less than 28 weeks and 1000 grams. J Cardiothorac Surg. 2016 Oct 4;11(1):146. doi: 10.1186/s13019-016-0539-3. PMID: 27716331; PMCID: PMC5050727.
Turkcan BS, Atalay A, Bozkaya D, Kulahcioglu E, Tasoglu I. Bedside Patent Ductus Arteriosus Ligation in Premature Infants. J Coll Physicians Surg Pak. 2022 Feb;32(2):208-212. doi: 10.29271/jcpsp.2022.02.208. PMID: 35108793.
Lee LK, Woodfin MY, Vadi MG, Grogan TR, Ross PJ, Applegate RL 2nd, Iravani M. A comparison of postoperative outcomes with PDA ligation in the OR versus the NICU: a retrospective cohort study on the risks of transport. BMC Anesthesiol. 2018 Dec 22;18(1):199. doi: 10.1186/s12871-018-0658-6. PMID: 30579349; PMCID: PMC6303951.
Gould DS, Montenegro LM, Gaynor JW, Lacy SP, Ittenbach R, Stephens P, et al. A comparison of on-site and off-site patent ductus arteriosus ligation in premature infants. Pediatrics 2003;112:1298-301.
Coster DD, Gorton ME, Grooters RK, Thieman KC, Schneider RF, Soltanzadeh H. Surgical closure of the patent ductus arteriosus in the neonatal intensive care unit. Ann Thorac Surg 1989;48:386-9.
Tsang FHF, Cheng LC, Yung TC, Chau AKT, Chiu CSW. Ligation of patent ductus arteriosus for premature infants in intensive care unit. HK J Paediatr (new series) 2005;10:282-5.
Finer NN, Woo BC, Hayashi A, Hayes B. Neonatal surgery: intensive care unit versus operating room. J Pediatr Surg 1993;28:645-9.
Gavilanes AWD, Heineman E, Herpers MJHM, Blanco CE. Use of neonatal intensive care unit as a safe place for neonatal surgery. Arch Dis Child Fetal Neonatal Ed. 1997;76(1):F51–3.
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














