Comparison between Lidocaine Spray and Oral Paracetamol for Pain Reduction during Amniocentesis in Second Trimester Pregnancy; A Randomize Controlled Trial
DOI:
https://doi.org/10.33192/smj.v76i1.266128Keywords:
Lidocaine spray, Paracetamol, Pain, AmniocentesisAbstract
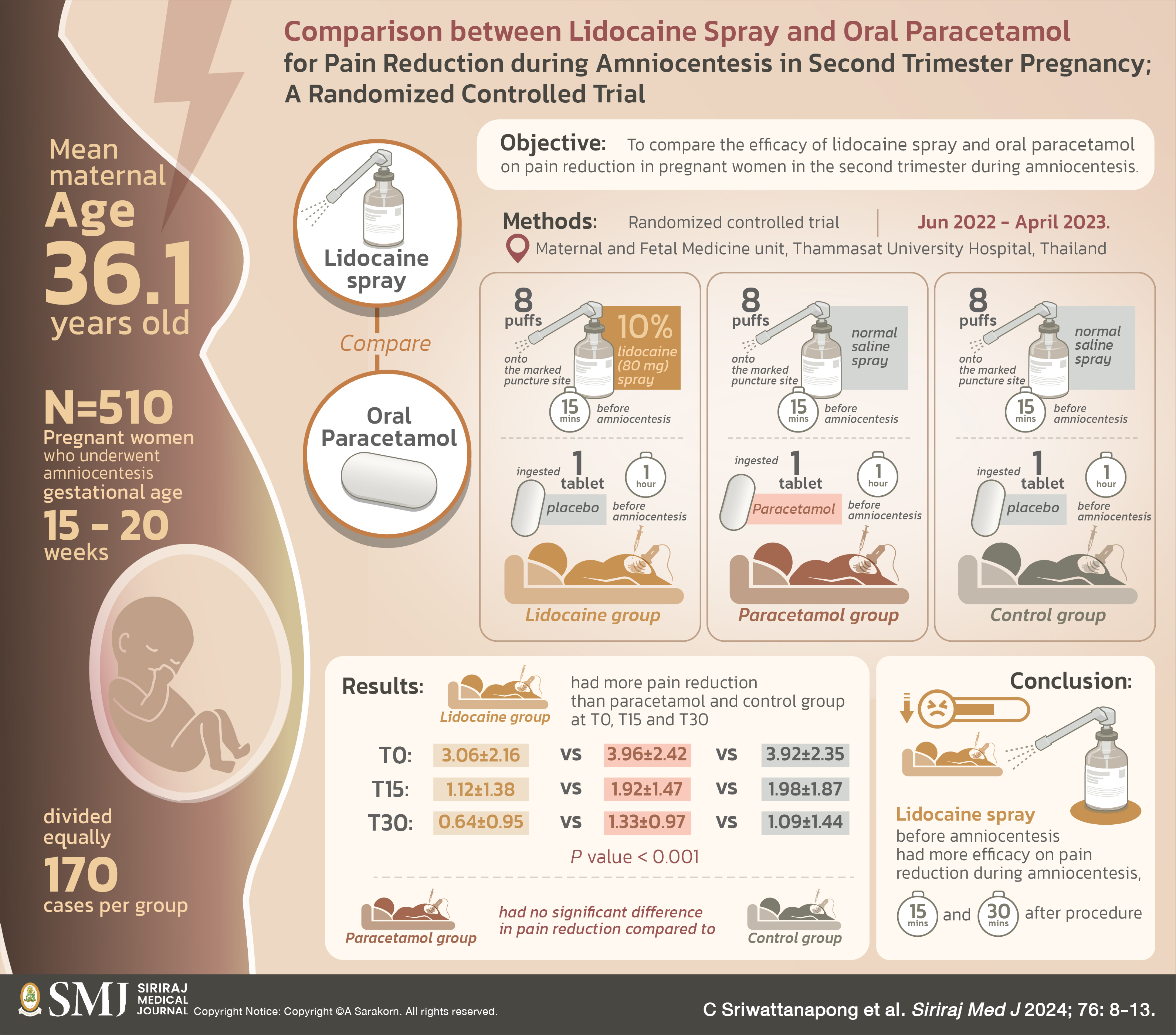
Objective: The aim of this study was to compare the efficacy of lidocaine spray and oral paracetamol on pain reduction in pregnant women in the second trimester during amniocentesis.
Materials and Methods: This was a prospective randomized-controlled trial study conducted at Maternal and Fetal Medicine unit, Thammasat University Hospital, Pathum Thani, Thailand between June 2022 and April 2023. Participants were pregnant women who underwent amniocentesis during gestational age between 15 and 20 weeks. They were allocated into three groups namely lidocaine, paracetamol and control groups. Subjects in lidocaine group received 8 puffs of 10% lidocaine (80 mg) spray onto the marked puncture site for five minutes before amniocentesis and ingested 1 placebo tablet 1 hour before procedure. Paracetamol group ingested 650 mg paracetamol orally 1 hour before amniocentesis and received 8 puffs of normal saline spray on the marked puncture site. Control group received 8 puffs of normal saline spray onto the marked puncture site for five minutes before amniocentesis and ingested 1 placebo tablet 1 hour before amniocentesis. Expected pain (Te), during procedure (T0), 15 and 30 minutes after procedure (T15 and T30) were evaluated based on 10-cm visual analog scale (VAS).
Results: A total of 510 pregnant women were recruited and divided equally (170 cases per group). Mean maternal age was 36.1 years old. Demographic characters of three groups were comparable. Lidocaine had more pain reduction than paracetamol and control group at T0, T15 and T30 (at T0: 3.06±2.16 vs 3.96±2.42 vs 3.92±2.35, P value < 0.001, T15: 1.12±1.38 vs 1.92±1.47 vs 1.98±1.87, P value < 0.001, T30: 0.64±0.95 vs 1.33±0.97 vs 1.09±1.44, P value < 0.001). However, paracetamol had no significant difference in pain reduction compared to control group.
Conclusion: Lidocaine spray before amniocentesis had more efficacy on pain reduction during amniocentesis, 15 and 30 minutes after procedure.
References
Cunningham FG, Leveno KJ. Prenatal diagnosis. In: Cunningham FG, Lenovo KJ, editors. Williams obstetrics. 26th ed. New York: McGraw-Hill Education; 2022. p.277-99.
Suntornlimsiri W, Naunkeaw K. Clinical correlates of pain with second-trimester genetic amniocentesis. J Med Assoc Thai. 2009;92:1567-72.
Thanitha T, Dennopporn S, Lunthaporn P. Oral paracetamol premedication effect on maternal pain in amniocentesis: a randomized double blind placebo-controlled trial. J Obstet Gynaecol. 2018;38:1078-82.
Gordon MC, Ventura-Braswell A, Higby K, Ward JA. Does local anesthesia decrease pain perception in women undergoing amniocentesis. Am J Obstet Gynecol. 2007;196:55.e1-4.
Elimian A, Goodman JR, Knudtson E, Wagner A, Wilson P, Williams M. Local anesthesia and pain perception during amniocentesis: a randomized double blind placebo-controlled trial. Prenat Diagn. 2013;33:1158-61.
Homkrun P, Tongsong T, Srisupundit K. Effect of xylocaine spray for analgesia during amniocentesis: a randomized controlled trial. Prenat Diagn. 2019;39:1179-83.
Pongrojpaw D, Somprasit C, Chanthasenanont A. The efficacy of lidocaine-prilocaine cream to reduce pain in genetic amniocentesis. J Med Assoc Thai. 2007;90:1992-6.
Derry S, Wiffen PJ, Moore RA, Quinlan J. Topical lidocaine for neuropathic pain in adults. Cochrane Database Syst Rev. 2014;2014:CD010958.
Benchahong S, Pongrojpaw D, Chanthasenanont A, Limpivest U, Nanthakomon T, Lertvutivivat S, et al. Cold therapy for pain relief during and after amniocentesis procedure: A randomized controlled trial. J Obstet Gynaecol Res. 2021;47:2623-31.
Hanprasertpong T, Kor-Anantakul O, Prasartwanakit V, Leetanaporn R, Suntharasaj T, Suwanrath C. Efficacy of cryoanalgesia in decreasing pain during second trimester genetic amniocentesis: a randomized trial. Arch Gynecol Obstet. 2012;286:563-6.
Wax JR, Pinette MG, Carpenter M, Chard R, Blackstone J, Cartin A. Reducing pain with genetic amniocentesis-A randomized trial of subfreezing versus room temperature needles. J Matern Fetal Neonatal Med. 2005;18:221-4.
Anderson BJ. Paracetamol (Acetaminophen): mechanisms of action. Paediatr Anaesth. 2008;18:915-21.
Hanprasertpong T, Kor-anantakul O, Leetanaporn R, Suwanrath C, Suntharasaj T, Pruksanusak N, et al. Music Listening to Decrease Pain during Second Trimester Genetic Amniocentesis: A Randomized Trial. J Med Assoc Thai. 2016;99:1272-6.
Hanprasertpong T, Koranantakul O, Leetanaporn R, Suwanrath C, Thitima S, Pruksanusak N, et al. Reducing pain and anxiety during second trimester genetic amniocentesis using aromatic therapy: a randomized trial. J Med Assoc Thai. 2015;98:734-8.
Yang X, Wei X, Mu Y, Li Q, Liu J. A review of the mechanism of the central analgesic effect of lidocaine. Medicine (Baltimore). 2020;99(17):e19898.
Anderson BJ. Paracetamol (Acetaminophen): mechanisms of action. Paediatr Anaesth. 2008;18(10):915-21.
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














