Determining Perioperative Mortality in Patients with Ruptured Abdominal Aortic Aneurysm: Insights from a Retrospective Cohort Study
DOI:
https://doi.org/10.33192/smj.v76i8.266315Keywords:
Ruptured abdominal aortic aneurysm, perioperative mortality factorsAbstract
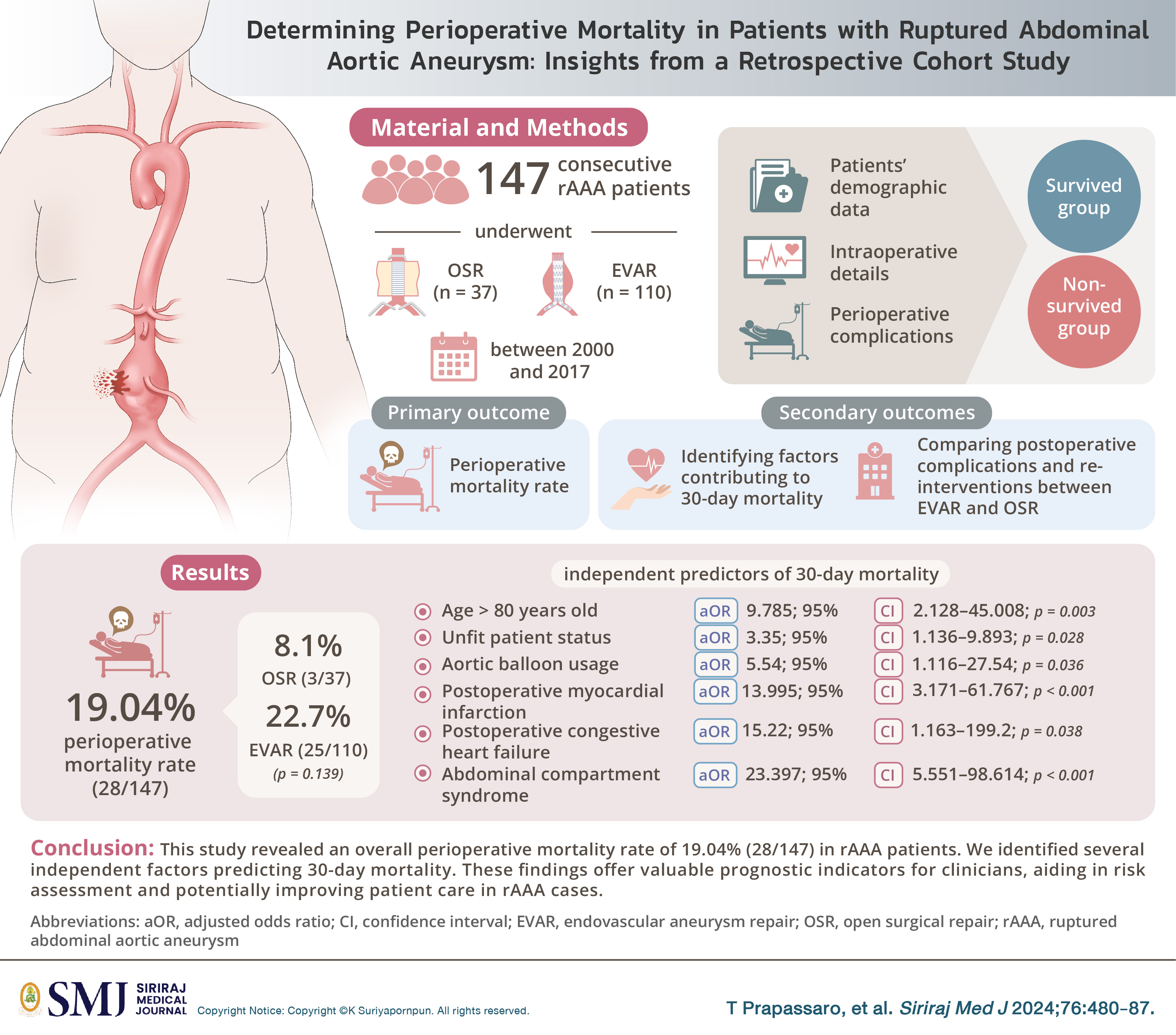
Objective: Analyzing factors determining perioperative mortality in patients with ruptured abdominal aortic aneurysm (rAAA) undergoing open surgical repair (OSR) and endovascular aneurysm repair (EVAR).
Materials and Methods: Inclusion of 147 consecutive rAAA patients who underwent OSR (n=37) or EVAR (n=110) between 2000 and 2017. Assessment of patients' demographic data, intraoperative details, and perioperative complications. Investigation of comparative outcomes between OSR and EVAR. Employing logistic regression analysis to identify factors associated with perioperative mortality.
Results: Perioperative mortality rate of 19.04% (28/147), with 8.1% (3/37) for OSR and 22.7% (25/110) for EVAR (p=0.139). Higher prevalence of unfit patients in the non-survived group (82.1% vs. 47.9%, p=0.002). Non-survived group had significantly higher preoperative serum creatinine levels (1.8 ± 1.74 vs. 1.4 ± 5.89, p=0.011). Intraoperatively, non-survived group had higher rates of aortic balloon usage and cardiac arrest (64.3% vs. 22.7% and 28.6% vs. 3.4%, p < 0.001). Multivariable analysis identified age > 80 years old, unfit patient status, aortic balloon usage, postoperative myocardial infarction, postoperative congestive heart failure, and abdominal compartment syndrome as independent predictors of 30-day mortality.
Conclusions: No significant difference in perioperative mortality between OSR and EVAR in rAAA patients. Independent predictors of 30-day mortality include age > 80 years old, unfit patient status, aortic balloon usage, postoperative myocardial infarction, congestive heart failure, and abdominal compartment syndrome. Valuable insights for clinicians in predicting outcomes and improving patient care in rAAA cases.
References
Stather PW, Sidloff D, Dattani N, Choke E, Bown MJ, Sayers RD. Systematic review and meta-analysis of the early and late outcomes of open and endovascular repair of abdominal aortic aneurysm. Br J Surg. 2013;100(7):863-72.
Wongwanit C, Mutirangura P, Chierakul N, Chaiyasoot W, Phongraweewan O. Rapidly Enlarging and Asymptomatic Abdominal Aortic Aneurysm in a Male Patient with Chronic Obstructive Pulmonary Disease: A Case Report of Endovascular Aortic Aneurysm Repair (EVAR). Siriraj Med J. 2006;58(5):812-18.
Badger S, Forster R, Blair PH, Ellis P, Kee F, Harkin DW. Endovascular treatment for ruptured abdominal aortic aneurysm. Cochrane Database Syst Rev. 2017;5(5):CD005261.
Antoniou GA, Georgiadis GS, Antoniou SA, Pavlidis P, Maras D, Sfyroeras GS, et al. Endovascular repair for ruptured abdominal aortic aneurysm confers an early survival benefit over open repair. J Vasc Surg. 2013;58(4):1091-105.
Aziz F. Ruptured abdominal aortic aneurysm: Is endovascular aneurysm repair the answer for everybody? Semin Vasc Surg. 2016;29(1-2):35-40.
de Boer M, Shiraev T, Waller J, Qasabian R. Has EVAR changed the outcomes of ruptured abdominal aortic aneurysms? A decades worth of experience in an Australian Teaching Hospital. ANZ J Surg. 2022;92(4):730-35.
Brown LC, Epstein D, Manca A, Beard JD, Powell JT, Greenhalgh RM. The UK Endovascular Aneurysm Repair (EVAR) trials: design, methodology and progress. Eur J Vasc Endovasc Surg. 2004;27(4):372-81.
Kirkpatrick AW, Roberts DJ, De Waele J, Jaeschke R, Malbrain M, Keulenaer B, et al. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013;39:1190-206.
Menges AL, M DO, Zimmermann A, Dueppers P. Ruptured abdominal aorto-iliac aneurysms: Diagnosis, treatment, abdominal compartment syndrome, and role of simulation-based training. Semin Vasc Surg. 2023;36(2):163-73.
Reimerink JJ, Hoornweg LL, Vahl AC, Wisselink W, Broek T, Legemate DA, et al. Endovascular repair versus open repair of ruptured abdominal aortic aneurysms: a multicenter randomized controlled trial. Ann Surg. 2013;258(2):248-56.
Desgranges P, Kobeiter H, Katsahian S, Bouffi M, Gouny P, Favre JP, et al. Editor's Choice - ECAR (Endovasculaire ou Chirurgie dans les Anévrysmes aorto-iliaques Rompus): A French Randomized Controlled Trial of Endovascular Versus Open Surgical Repair of Ruptured Aorto-iliac Aneurysms. Eur J Vasc Endovasc Surg. 2015;50(3):303-10.
Powell JT, Sweeting MJ, Thompson MM, Ashleigh R, Bell R, Gomes M, et al. Endovascular or open repair strategy for ruptured abdominal aortic aneurysm: 30 day outcomes from IMPROVE randomised trial. BMJ 2014;348:f7661.
Greenhalgh RM, Brown LC, Powell JT, Thompson SG, Epstein D. Endovascular repair of aortic aneurysm in patients physically ineligible for open repair. N Engl J Med. 2010;362(20):1872-80.
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














