The Outcomes of Peripherally Inserted Central Catheter (PICC) Insertion in Pediatric Patients at Siriraj Hospital
Outcomes of PICC in Pediatric Patients
DOI:
https://doi.org/10.33192/smj.v76i3.266562Keywords:
Peripherally inserted central catheter, pediatric PICC, complicationsAbstract
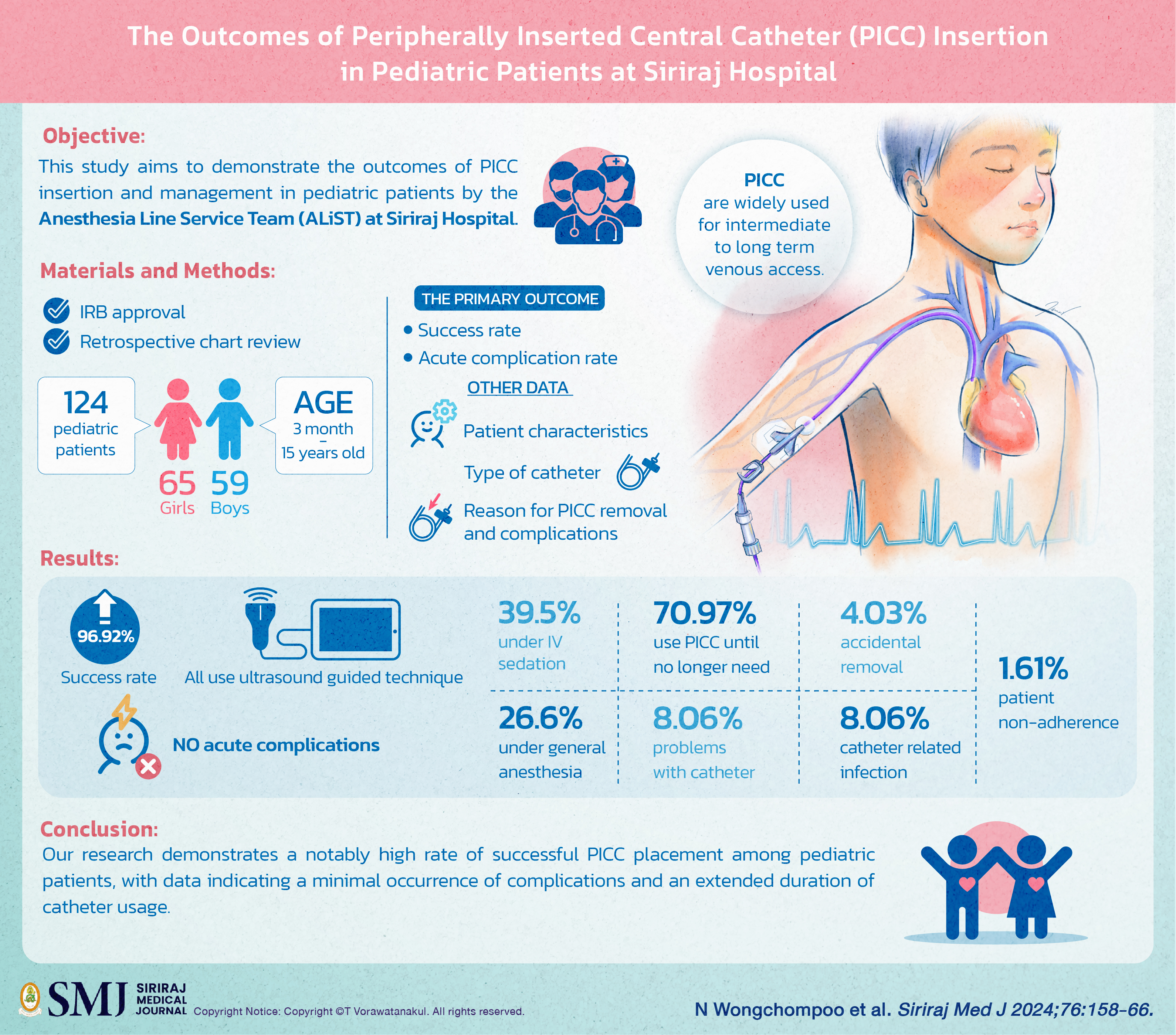
Objective: Peripherally Inserted Central Catheters (PICC) are widely used for intermediate to long term venous access. Venipunctures and catheterizations in pediatric patients can be challenging and traumatizing to children’s veins due to frequent and painful needle sticks. This study aims to demonstrate the outcomes of PICC insertion and management in pediatric patients by the Anesthesia Line Service Team (ALiST) at Siriraj Hospital.
Materials and Methods: This is a retrospective, descriptive study collecting data from January 2018 to December 2021. The inclusion criteria were pediatric patients aged 15 years and under, body weight equal to or exceeding 5 kg with no history of previous complicated central venous accesses. The primary outcome is the success rate of insertion.
Results: 124 PICCs were inserted in pediatric patients. The median age of patients was 5.0 years, with a median height of 107.8 cm, and a median weight of 10.0 kg. The successful insertion rate was 96.92%, and all insertions were inserted using ultrasound-guided technique, with or without fluoroscopy. No acute complications were noted during insertion. Most patients received either intravenous sedation (39.5%) or general anesthesia (26.6%) during the procedure. The mean duration of catheter indwelling was 66.48 days. Reasons for removal of PICC included completion of therapy and patient demise (70.97%), catheter malformation (8.06%), accidental removal (4.03%), infection (8.06%), and patient non-adherence (1.61%).
Conclusion: Our research demonstrates a notably high rate of successful PICC placement among pediatric patients, with data indicating a minimal occurrence of complications and an extended duration of catheter usage.
References
Thiagarajan RR, Ramamoorthy C, Gettmann T, Bratton SL. Survey of the use of peripherally inserted central venous catheters in children. Pediatrics. 1997;99(2):E4.
Grewal S, Towbin R, Schaefer C, Aria D. How We Do It: Peripherally Inserted Central Catheter Placement (PICC). Appl Radiol. 2020;1(1):1.
Anthony KK, Gil KM, Schanberg LE. Brief report: Parental perceptions of child vulnerability in children with chronic illness. J Pediatr Psychol. 2003;28(3):185-90.
Delarbre B, Dabadie A, Stremler-Lebel N, Jolibert M, Cassagneau P, Lebel S, et al. Introduction of the use of a pediatric PICC line in a French University Hospital: review of the first 91 procedures. Diagn Interv Imaging. 2014;95(3):277-81.
Badheka A, Bloxham J, Schmitz A, Freyenberger B, Wang T, Rampa S, et al. Outcomes associated with peripherally inserted central catheters in hospitalised children: a retrospective 7-year single-centre experience. BMJ Open. 2019;9(8):e026031.
Laochareonsuk W, Boonsanit K, Chotsompancharoen T. Sangkhathat S. An Appraisal of Totally Implantable Venous Access Devices in Pediatric Cancers. Siriraj Med J. 2020;72(2):95-102.
Jumani K, Advani S, Reich NG, Gosey L, Milstone AM. Risk factors for peripherally inserted central venous catheter complications in children. JAMA Pediatr. 2013;167(5):429-35.
Raina R, Mittal A, Sethi SK, Chakraborty R. Challenges of Vascular Access in the Pediatric Population. Adv Chronic Kidney Dis. 2020;27(3):268-75.
Naik VM, Mantha SSP, Rayani BK. Vascular access in children. Indian J Anaesth. 2019;63(9):737-45.
Wrightson DD. Peripherally inserted central catheter complications in neonates with upper versus lower extremity insertion sites. Adv Neonatal Care. 2013;13(3):198-204.
Kwon S, Son SM, Lee SH, Kim JH, Kim H, Kim JY, et al. Outcomes of bedside peripherally inserted central catheter placement: a retrospective study at a single institution. Acute Crit Care. 2020;35(1):31-7.
Westergaard B, Classen V, Walther-Larsen S. Peripherally inserted central catheters in infants and children - indications, techniques, complications and clinical recommendations. Acta Anaesthesiol Scand. 2013;57(3):278-87.
Tariq M, Huang DT. PICCing the best access for your patient. Crit Care. 2006;10(5):315.
Gunst M, Matsushima K, Vanek S, Gunst R, Shafi S, Frankel H. Peripherally inserted central catheters may lower the incidence of catheter-related blood stream infections in patients in surgical intensive care units. Surg Infect (Larchmt). 2011;12(4):279-82.
Limprayoon K, Borisut C, Vichainsarn S. The Quality Improvement of Central Venous Catheter Associated Blood Stream Infection (CABSI) by New Clinical Practice Guideline in Pediatric ICU Siriraj Hospital. Siriraj Med J. 2007;59(4):181-3.
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














