Prevalence of Abnormal Cerebroplacental Ratio in Uncomplicated Full-term Pregnancy and Correlation with Adverse Perinatal Outcomes
DOI:
https://doi.org/10.33192/smj.v76i8.267732Keywords:
Umbilical artery, Middle cerebral artery, Cerebroplacental ratioAbstract
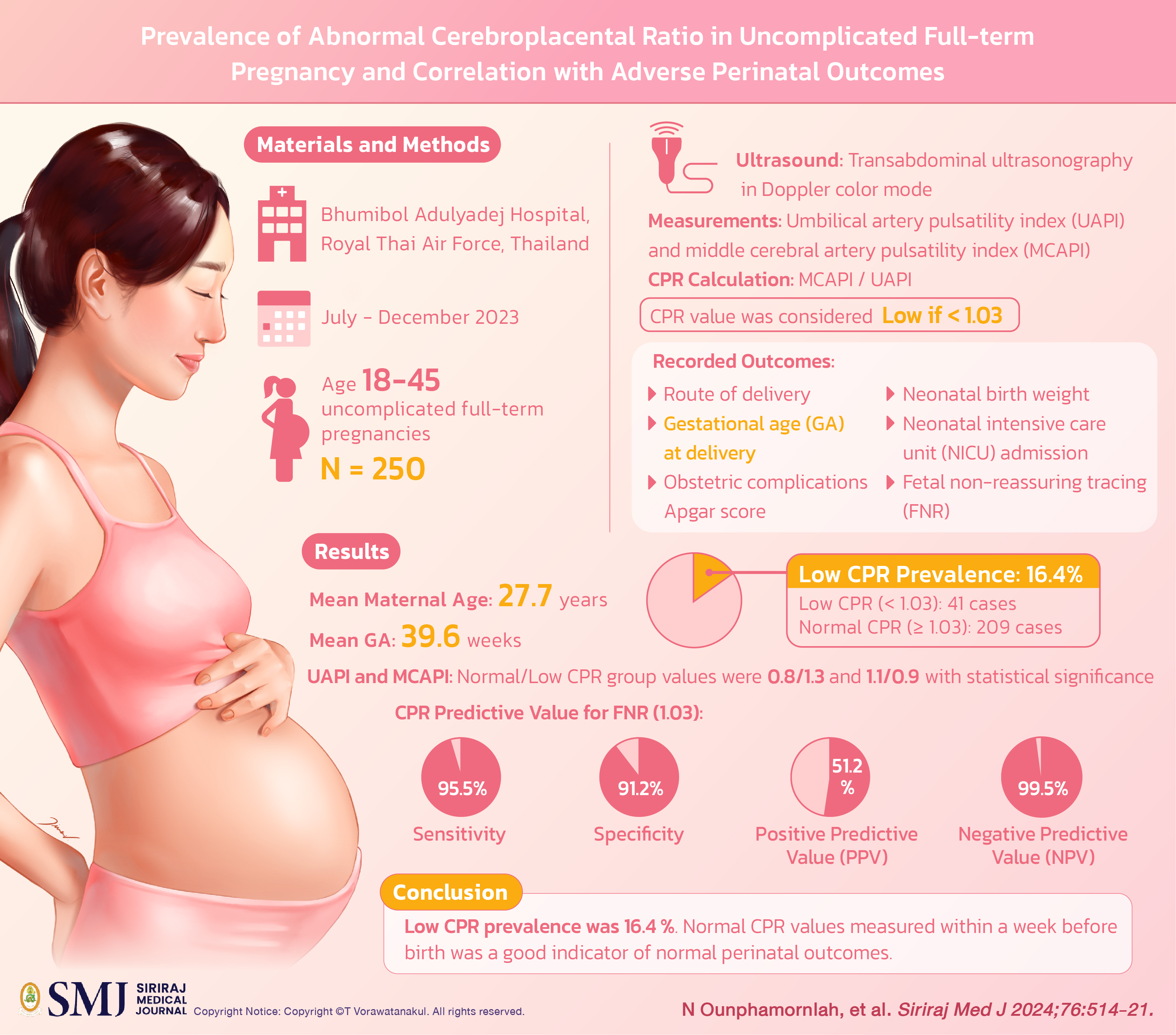
Objective: To investigate the prevalence of abnormal cerebroplacental ratio (CPR) and predicting values for adverse perinatal outcomes in uncomplicated full-term pregnancies.
Materials and Methods: This prospective cross-sectional study was conducted at Bhumibol Adulyadej Hospital, Royal Thai Air Force, Thailand between July and December 2023. The study population comprised pregnant women between the ages 18 and 45 presenting uncomplicated full-term pregnancies. Transabdominal ultrasonography in Doppler color mode was performed on all participants. Umbilical artery pulsatility index (UAPI) and middle cerebral artery pulsatility index (MCAPI) were both measured. CPR was calculated by MCAPI divided by UAPI. A CPR value was considered low if it was less than 1.03. Obstetric and perinatal outcomes were recorded including route of delivery, gestational age (GA) at delivery, obstetric complications, Apgar score, neonatal birth weight, neonatal intensive care unit (NICU) admission, and fetal non-reassuring tracing (FNR).
Results: A total of 250 pregnant women were recruited. The mean maternal age and GA was 27.7 years, 39.6 weeks, respectively. Low CPR prevalence was recorded at 16.4 percent. There were 41 and 209 cases in low (<1.03) and normal (≥1.03) CPR groups, respectively. UAPI and MCAPI of the normal/low CPR group were 0.8/1.3 and 1.1/0.9 with statistical significance. CPR for predicted value of FNR (1.03) gave sensitivity, specificity, PPV, and NPV at 95.5, 91.2, 51.2 and 99.5 percent, respectively. This study presented no adverse perinatal outcomes.
Conclusion: Low CPR prevalence was 16.4 percent. Normal CPR values measured within a week before birth was a good indicator of normal perinatal outcomes.
References
Rocha AS, Andrade ARA, Moleiro ML, Guedes-Martins L. Doppler Ultrasound of the Umbilical Artery: Clinical Application. Rev Bras Ginecol Obstet. 2022;44(5):519-31.
Buca D, Liberati M, Rizzo G, Gazzolo D, Chiarelli F, Giannini C, et al. Pre- and postnatal brain hemodynamics in pregnancies at term: correlation with Doppler ultrasound, birthweight, and adverse perinatal outcome. J Matern Fetal Neonatal Med. 2022;35(4):713-9.
Fiolna M, Kostiv V, Anthoulakis C, Akolekar R, Nicolaides KH. Prediction of adverse perinatal outcome by cerebroplacental ratio in women undergoing induction of labor. Ultrasound Obstet Gynecol. 2019;53(4):473-80.
Vollgraff Heidweiller-Schreurs CA, De Boer MA, Heymans MW, Schoonmade LJ, Bossuyt PMM, Mol BWJ, et al. Prognostic accuracy of cerebroplacental ratio and middle cerebral artery Doppler for adverse perinatal outcome: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2018;51(3):313-22.
Bhide A, Acharya G, Baschat A, Bilardo CM, Brezinka C, Cafici D, et al. ISUOG Practice Guidelines (updated): use of Doppler velocimetry in obstetrics. Ultrasound Obstet Gynecol. 2021;58(2):331-9.
Yin Q, Zhang Y, Ma Q, Gao L, Li P, Chen X. The clinical value of blood flow parameters of the umbilical artery and middle cerebral artery for assessing fetal distress. Am J Transl Res. 2021;13(5):5280-6.
Di Mascio D, Rizzo G, Buca D, D'Amico A, Leombroni M, Tinari S, et al. Comparison between cerebroplacental ratio and umbilicocerebral ratio in predicting adverse perinatal outcome at term. Eur J Obstet Gynecol Reprod Biol. 2020;252:439-43.
Antepartum Fetal Surveillance: ACOG Practice Bulletin, Number 229. Obstet Gynecol. 2021;137(6):e116-e27.
Gilroy LC, Al-Kouatly HB, Minkoff HL, McLaren RA, Jr. Changes in obstetrical practices and pregnancy outcomes following the ARRIVE trial. Am J Obstet Gynecol. 2022;226(5): 716.e1- e12.
Besimoglu B, Uyan Hendem D, Atalay A, Goncu Ayhan S, Sinaci S, Tanacan A, et al. Combination of Doppler measurements with amniotic fluid volume for the prediction of perinatal outcomes in fetal growth restriction. Int J Gynaecol Obstet. 2023;161(1):190-7.
Mascherpa M, Pegoire C, Meroni A, Minopoli M, Thilaganathan B, Frick A, et al. Prenatal prediction of adverse outcome using different charts and definitions of fetal growth restriction. Ultrasound Obstet Gynecol. 2023.
Shmueli A, Mor L, Blickstein O, Sela R, Weiner E, Gonen N, et al. Placental pathology in pregnancies with late fetal growth restriction and abnormal cerebroplacental ratio. Placenta. 2023;138:83-7.
Sapoval J, Singh V, Carter RE. Ultrasound Biophysical Profile. StatPearls. Treasure Island (FL)2023.
Umana OD, Siccardi MA. Prenatal Nonstress Test. StatPearls. Treasure Island (FL)2023.
Arnold JJ, Gawrys BL. Intrapartum Fetal Monitoring. Am Fam Physician. 2020;102(3):158-67.
Lin XS, Peng XY, Yang MM, Ning LL, Shao YW, Jiang Y, et al. The single pregnancy predicting model of 1 minute Apgar score less than 7 after preterm birth: A retrospective study. PLoS One. 2022;17(12):e027938
Sirivunnabood T, Wanitpongpan P, Yapan P. Incidence and risk factors of neonatal sepsis in preterm premature rupture of membranes before 34 weeks of gestation. Siriraj Med J. 2022;74:169-77.
Qureshey EJ, Mendez-Figueroa H, Wiley RL, Bhalwal AB, Chauhan SP. Cesarean delivery at term for non-reassuring fetal heart rate tracing: risk factors and predictability. J Matern Fetal Neonatal Med. 2022;35(25):6714-20.
Dall'Asta A, Ghi T, Rizzo G, Cancemi A, Aloisio F, Arduini D, et al. Cerebroplacental ratio assessment in early labor in uncomplicated term pregnancy and prediction of adverse perinatal outcome: prospective multicenter study. Ultrasound Obstet Gynecol. 2019;53(4):481-7
Gunay T, Bilir RA, Hocaoglu M, Bor ED, Ozdamar O, Turgut A. The role of abnormal cerebroplacental ratio in predicting adverse fetal outcome in pregnancies with scheduled induction of labor. Int J Gynaecol Obstet. 2021;153(2):287-93.
Mecke L, Ignatov A, Redlich A. The importance of the cerebroplacental ratio for the prognosis of neonatal outcome in AGA fetuses. Arch Gynecol Obstet. 2023;307(1):311-7.
Chainarong N, Petpichetchian C. The relationship between intrapartum cerebroplacental ratio and adverse perinatal outcomes in term fetuses. Eur J Obstet Gynecol Reprod Biol. 2018;228:82-6.
Bendall A, Schreiber V, Crawford K, Kumar S. Predictive utility of the fetal cerebroplacental ratio for hypoxic ischaemic encephalopathy, severe neonatal morbidity and perinatal mortality in late-preterm and term infants. Aust N Z J Obstet Gynaecol. 2023;63(4):491-8.
Mathewlynn S, Beriwal S, Ioannou C, Cavallaro A, Impey L. Abnormal umbilical artery pulsatility index in appropriately grown fetuses in the early third trimester: an observational cohort study. J Matern Fetal Neonatal Med. 2023;36(1):2152670.
Winchester ML, McCarther N, Cancino D, Fitzgerald S, Parrish M. Second trimester cerebroplacental ratio versus umbilicocerebral ratio for the prediction of adverse perinatal outcomes. J Matern Fetal Neonatal Med. 2022;35(25):7929-35.
Irvine KM, Bligh LN, Kumar S. Association between the fetal cerebroplacental ratio and biomarkers of hypoxia and angiogenesis in the maternal circulation at term. Eur J Obstet Gynecol Reprod Biol. 2020;245:198-204.
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














