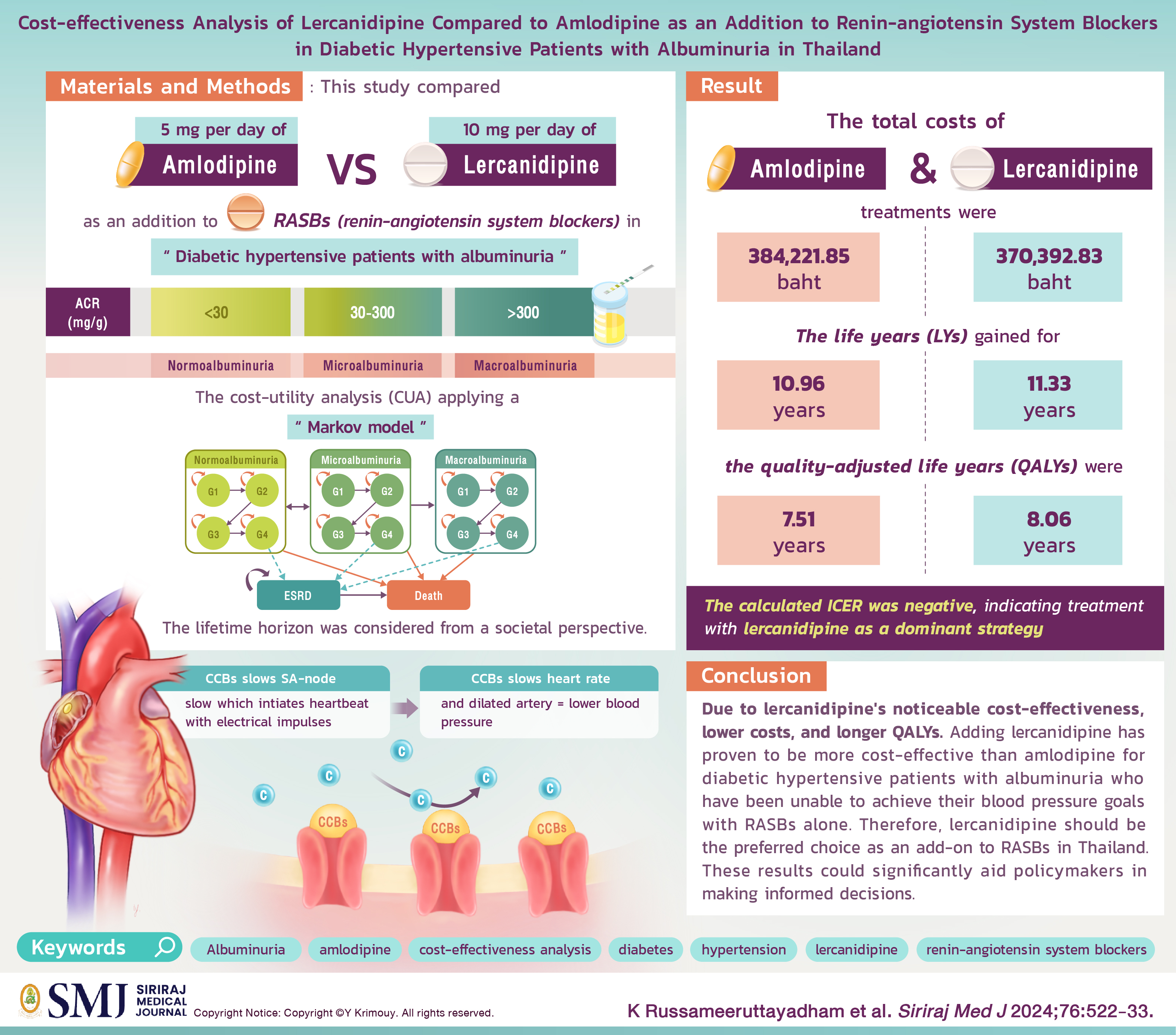
Cost-effectiveness Analysis of Lercanidipine Compared to Amlodipine as an Addition to Renin-angiotensin System Blockers in Diabetic Hypertensive Patients with Albuminuria in Thailand
DOI:
https://doi.org/10.33192/smj.v76i10.267782Keywords:
Albuminuria, amlodipine, cost-effectiveness analysis, Type 2 diabetes mellitus, hypertension, lercanidipine, renin-angiotensin system blockersAbstract
Objective: Dihydropyridine calcium channel blocker (DHP-CCBs) is an appropriate add-on antihypertensive option for uncontrolled blood pressure diabetic hypertensive patients with albuminuria who are already taking renin-angiotensin system blockers (RASBs). Among DHP-CCBs, amlodipine is the first-line medication in combination with RASBs. However, new-generation DHP-CCBs like lercanidipine has demonstrated superior effectiveness and fewer side effects, although at a higher cost than amlodipine. This study aims to assess the cost-effectiveness of lercanidipine versus amlodipine when added to RASBs in diabetic hypertensive patients with albuminuria. The objective is to provide robust evidence guiding the selection of the most suitable and worthwhile treatment option in Thailand.
Materials and Methods: This study analyses the cost-effectiveness of lercanidipine versus amlodipine as an addition to RASBs in diabetic hypertensive patients with albuminuria. The analysis was conducted from a societal perspective using a Markov model.
Results: The total costs of lercanidipine and amlodipine treatments were 370,392.83 baht and 384,221.85 baht, respectively. The life years gained for lercanidipine and amlodipine treatments were 11.33 years and 10.96 years respectively. Additionally, the quality-adjusted life years (QALYs) of lercanidipine and amlodipine treatments were 8.06 years and 7.51 years respectively.
Conclusion: Due to lercanidipine's noticeable cost-effectiveness, lower costs, and longer QALYs. Adding lercanidipine has proven to be more cost-effective than amlodipine for diabetic hypertensive patients with albuminuria who have been unable to achieve their blood pressure goals with RASBs alone. Therefore, lercanidipine should be the preferred choice as an add-on to RASBs in Thailand. These results could significantly aid policymakers in making informed decisions.
References
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. 2018;39(33):3021-104.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57.
Müller-Nurasyid M. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398(10304):957-80.
Cheung AK, Chang TI, Cushman WC, Furth SL, Hou FF, Ix JH, et al. KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int. 2021;99(3):S1-S87.
Tomson CR, Cheung AK, Mann JF, Chang TI, Cushman WC, Furth SL, et al. Management of blood pressure in patients with chronic kidney disease not receiving dialysis: synopsis of the 2021 KDIGO clinical practice guideline. Ann Intern Med. 2021;174(9):1270-81.
Bilous RW, Gonzalez-Campoy JM, Fradkin JE, Mauer M, Molitch ME, Narva AS, et al. KDOQI clinical practice guideline for diabetes and CKD: 2012 update. Am J Kidney Dis. 2012.
Turner R, Holman R, Matthews D, Bassett P, Coster R, Stratton I, et al. Hypertension in diabetes study (HDS). I. Prevalence of hypertension in newly presenting Type-2 diabetic-patients and the association with risk-factors for cardiovascular and diabetic complications. J Hypertens. 1993;11(3):309-17.
Cowie CC, Harris MI. Physical and metabolic characteristics of persons with diabetes. In: Harris MI, editor. Diabetes in America. 2nd ed. 1 Information Way, Bethesda: National Diabetes Information Clearinghouse; 1995.p.117-64.
Adler AI, Stratton IM, Neil HA, Yudkin JS, Matthews DR, Cull CA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000;321(7258):412-9.
Gerber LM, Shmukler C, Alderman MH. Differences in urinary albumin excretion rate between normotensive and hypertensive, white and nonwhite subjects. Arch Intern Med. 1992;152(2):373-7.
Giaconi S, Levanti C, Fommei E, Innocenti F, Seghieri G, Palla L, et al. Microalbuminuria and casual and ambulatory blood pressure monitoring in normotensives and in patients with borderline and mild essential hypertension. Am J Hypertens. 1989;2(4):259-61.
Romundstad S, Holmen J, Hallan H, Kvenild K, Ellekjær H. Microalbuminuria and all-cause mortality in treated hypertensive individuals: Does sex matter?: The Nord-Trøndelag Health Study (HUNT), Norway. Circulation. 2003;108(22):2783-9.
Parving H-H, Mogensen C, Evrin P-E. Increased urinary albumin-excretion rate in benign essential hypertension. The Lancet. 1974;303(7868):1190-2.
Bianchi S, Bigazzi R, Campese VM. Microalbuminuria in essential hypertension: Significance, pathophysiology, and therapeutic implications. Am J Kidney Dis. 1999;34(6):973-95.
Bigazzi R, Bianchi S, Campese VM, Baldari G. Prevalence of microalbuminuria in a large population of patients with mild to moderate essential hypertension. Nephron. 1992;61(1):94-7.
Mani A. Albuminuria in Hypertensive Patients: Where the Choice of Antihypertensive Medications Matters:: Commentary on "Several Conventional Risk Markers Suggesting Presence of Albuminuria Are Weak Among Rural Africans With Hypertension". J Clin Hypertens. 2016;18(1):31-2.
Kunanon S, Chattranukulchai P, Chotruangnapa C, Kositanurit W, Methavigul K, Boonyasirinant T, et al. 2019 Thai Guidelines on the Treatment of Hypertension: Executive Summary. J Med Assoc Thai. 2021;104(10):1729-38.
Mourad J-J, Le Jeune S, Pirollo A, Mourad C, Gaudouen Y, Lopez-Sublet M. Combinations of inhibitors of the renin–angiotensin system with calcium channel blockers for the treatment of hypertension: focus on perindopril/amlodipine. Curr Med Res. 2010;26(9):2263-76.
Cheng Y, Huang R, Kim S, Zhao Y, Li Y, Fu P. Renoprotective effects of renin–angiotensin system inhibitor combined with calcium channel blocker or diuretic in hypertensive patients: A PRISMA-compliant meta-analysis. Medicine (Baltimore). 2016;95(28):e4167.
Bakris GL, Sarafidis PA, Weir MR, Dahlöf B, Pitt B, Jamerson K, et al. Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomised controlled trial. Lancet. 2010;375(9721):1173-81.
Tabur S, Oğuz E, Sabuncu T, Korkmaz H, Çelik H. The effects of calcium channel blockers on nephropathy and pigment epithelium-derived factor in the treatment of hypertensive patients with type 2 diabetes mellitus. Clin Exp Hypertens. 2015;37(3):177-83.
Makani H, Bangalore S, Romero J, Htyte N, Berrios RS, Makwana H, et al. Peripheral edema associated with calcium channel blockers: incidence and withdrawal rate–a meta-analysis of randomized trials. J Hypertens. 2011;29(7):1270-80.
Sangam K, Devireddy P, Konuru V. Calcium channel blockers induced peripheral edema. Int J Pharm Sci Res. 2016;53:10.88.
Liang L, Kung JY, Mitchelmore B, Cave A, Banh HL. Comparative peripheral edema for dihydropyridines calcium channel blockers treatment: A systematic review and network meta-analysis. J Clin Hypertens (Greenwich). 2022;24(5):536-54.
Robles NR, Calvo C, Sobrino J, Espinel E, Esteban R, Mateos L, et al. Lercanidipine valuable effect on urine protein losses: the RED LEVEL study. Curr Med Res. 2016;32(Suppl 2):29-34.
Robles NR, Ocon J, Gomez CF, Manjon M, Pastor L, Herrera J, et al. Lercanidipine in patients with chronic renal failure: the ZAFRA study. Ren Fail. 2005;27(1):73-80.
Robles N, Romero B, de Vinuesa EG, Sánchez-Casado E, Cubero J. Treatment of proteinuria with lercanidipine associated with renin-angiotensin axis-blocking drugs. Ren Fail. 2010;32(2):192-7.
Raparti GT, Choure BK, Patil PT, Patne SS. A randomized comparison between lercanidipine and amlodipine for efficacy and tolerability in patients with essential hypertension. Int J Basic Clin Pharmacol. 2016;5(4):1181.
Goda A, Tase M, Banushi A, Goda T, Pavli E, Dado E, et al. Comparative effect of lercanidipine and amlodipine in the treatment of mild to moderate hypertension: PP.16.93. Journal of Hypertension. 2010;28:e277-e78.
Leonetti G, Magnani B, Pessina AC, Rappelli A, Trimarco B, Zanchetti A, et al. Tolerability of long-term treatment with lercanidipine versus amlodipine and lacidipine in elderly hypertensives. Am J Hypertens. 2002;15(11):932-40.
Makarounas-Kirchmann K, Glover-Koudounas S, Ferrari P. Results of a meta-analysis comparing the tolerability of lercanidipine and other dihydropyridine calcium channel blockers. Clin Ther. 2009;31(8):1652-63.
Sakulsupsiri A, Chattranukulchai P, Siwamogsatham S, Boonchayaanant P, Naeowong W, Ariyachaipanich A, et al. Home Blood Pressure Control and Drug Prescription Patterns among Thai Hypertensives: A 1-Year Analysis of Telehealth Assisted Instrument in Home Blood Pressure Monitoring Nationwide Pilot Project. Int J Hypertens. 2021;2021:8844727.
World Health Organization. World Health Statistics 2016 [OP]: Monitoring Health for the Sustainable Development Goals (SDGs): World Health Organization; 2016.
Ueapanjasin P, Thavornwattanayong W, Lertsirimunkong J, Chaiyakittisopon K. Cost-Effectiveness Analysis of Long-acting Injectable Once-monthly of Aripiprazole Compared with Long-acting Injectable Once-monthly Paliperidone Palmitate for the Treatment of Stable Schizophrenia Patients in Thailand. Siriraj Med J. 2023;75(10):725-35.
Trade Policy and Strategy Office. Economic and Trade Indices Database: ETID [cited 2023 March]. Available from: http://www.price.moc.go.th.
Drug and Medical Supply Information Center. Reference of Drugs Costs In: Ministry of Public Health Thailand. [cited 2023 March]. Available from: http://dmsic.moph.go.th/index/drugsearch/1.
Health Intervention and Technology Assessment: HITAP Ministry of Public Health. Standard Cost Lists for Health Technology Assessment [cited 2023 March]. Available from: http://costingmenu.hitap.net/.
Teerawattananon Y, Mugford M, Tangcharoensathien V. Economic evaluation of palliative management versus peritoneal dialysis and hemodialysis for end-stage renal disease: evidence for coverage decisions in Thailand. Value Health. 2007;10(1):61-72.
Korsah NN. Prevalence of renal impairment in diabetics with hypertension in Ghana. Western Reserve University; 2010.
Polonia J, Azevedo A, Monte M, Silva JA, Bertoquini S. Annual deterioration of renal function in hypertensive patients with and without diabetes. Vasc Health Risk. 2017:231-7.
Vesga JI, Cepeda E, Pardo CE, Paez S, Sanchez R, Sanabria RM. Chronic kidney disease progression and transition probabilities in a large preventive cohort in Colombia. Int J Nephrol. 2021;2021:8866446.
Berhane AM, Weil EJ, Knowler WC, Nelson RG, Hanson RL. Albuminuria and estimated glomerular filtration rate as predictors of diabetic end-stage renal disease and death. Clin J Am Soc Nephrol. 2011;6(10):2444-51.
Adler AI, Stevens RJ, Manley SE, Bilous RW, Cull CA, Holman RR, et al. Development and progression of nephropathy in type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS 64). Kidney Int. 2003;63(1):225-32.
Fici F, Ari Bakir E, Ilkay Yüce E, Kanuncu S, Makel W, Tarim BA, et al. PAIT-Survey Follow-Up: Changes in Albuminuria in Hypertensive Diabetic Patients with Mild-Moderate Chronic Kidney Disease. High Blood Press Cardiovasc Prev. 2020;27:43-9.
Scholze J, Bramlage P, Trenkwalder P, Kreutz R. Efficacy and safety of a fixed-dose combination of lercanidipine and enalapril in daily practice. A comparison of office, self-measured and ambulatory blood pressure. Expert Opin Pharmaco. 2011;12(18):2771-9.
Maldonado J, Pereira T, Tavares A. Efficacy and safety of a lercanidipine/enalapril fixed-dose combination in hypertensive patients in Portugal. Drug Dev Res. 2014;14:147-54.
Puig J, Calvo C, Luurila O, Luurila H, Sulosaari S, Strandberg A, et al. Lercanidipine, enalapril and their combination in the treatment of elderly hypertensive patients: placebo-controlled, randomized, crossover study with four ABPM. J Hum Hypertens. 2007;21(12):917-24.
Martinez-Martin FJ, Saiz-Satjes M. Add-on manidipine versus amlodipine in diabetic patients with hypertension and microalbuminuria: the AMANDHA study. Expert Rev Cardiovasc. 2008;6(10):1347-55.
Chrysant SG, Melino M, Karki S, Lee J, Heyrman R. The combination of olmesartan medoxomil and amlodipine besylate in controlling high blood pressure: COACH, a randomized, double-blind, placebo-controlled, 8-week factorial efficacy and safety study. Clin Ther. 2008;30(4):587-604.
Wang K-L, Yu W-C, Lu T-M, Chen L-C, Leu H-B, Chiang C-E. Amlodipine/valsartan fixed-dose combination treatment in the management of hypertension: A double-blind, randomized trial. J Chin Med Assoc. 2020;83(10):900.
Pérez-Maraver M, Carrera MJ, Micaló T, Sahun M, Vinzia C, Soler J, et al. Renoprotective effect of diltiazem in hypertensive type 2 diabetic patients with persistent microalbuminuria despite ACE inhibitor treatment. Diabetes Res Clin Pract. 2005;70(1):13-9.
Srisubat A, Sriratanaban J, Ngamkiatphaisan S, Tungsanga K. Cost-effectiveness of annual microalbuminuria screening in Thai diabetics. Asian Biomed. 2014;8(3):371-9.
Srisubat A, Jiamjariyaporn T, Chanpitakkul M, Leesmidt V, Wisansak W, Promnim S. Cost-effectiveness of integrated care in patients with chronic kidney disease stage 3 and 4 compared with standard care in rural communities. J Depart Med Serv. 2017;42(6):54-63.
Sullivan PW, Ghushchyan VH. EQ-5D scores for diabetes-related comorbidities. Value Health. 2016;19(8):1002-8.
Sullivan PW, Valuck R, Saseen J, MacFall HM. A comparison of the direct costs and cost effectiveness of serotonin reuptake inhibitors and associated adverse drug reactions. CNS drugs. 2004;18:911-32.
Ghamami N, Chiang SH, Dormuth C, Wright JM. Time course for blood pressure lowering of dihydropyridine calcium channel blockers. Cochrane Database Syst Rev. 2014(8):Cd010052.
Grassi G, Robles NR, Seravalle G, Fici F. Lercanidipine in the management of hypertension: an update. J Pharmacol Pharmacother. 2017;8(4):155-65.
Dalla Vestra M, Pozza G, Mosca A, Grazioli V, Lapolla A, Fioretto P, et al. Effect of lercanidipine compared with ramipril on albumin excretion rate in hypertensive Type 2 diabetic patients with microalbuminuria: DIAL Study (Diabete, Ipertensione, Albuminuria, Lercanidipina). Cardiovasc Ther Prev. 2022;9(7):41-8.
Robles N, Pastor L, Manjon M, Ocón J, Herrera J, Villatoro J, et al. Lercanidipine in diabetic patients with renal failure. Nefrología (Madr.). 2004;24(4):338-43.
Opie L. Pharmacological differences between calcium antagonists. Eur Heart J. 1997;18(Suppl_A):71-9.
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














