Incidence, Risk-factors, and Outcomes of Intraoperative Hypotension Following Spinal Anesthesia in Hip Fracture Surgery: A Retrospective Study from Thailand
DOI:
https://doi.org/10.33192/smj.v76i7.267837Keywords:
hip fracture, spinal anesthesia, intraoperative hypotension, complications, incidence, risk factorsAbstract
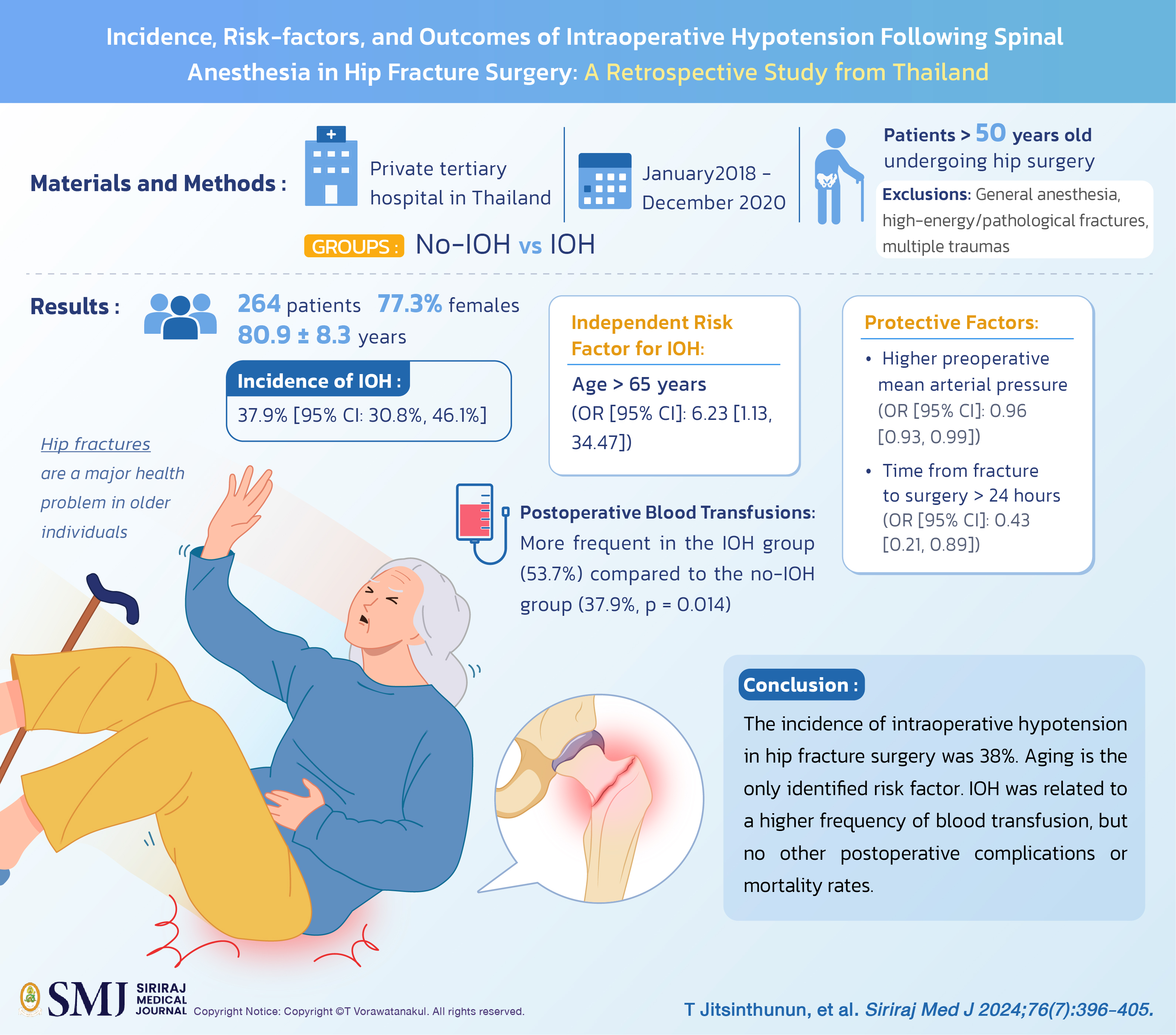
Objective: Hip fractures are a major health problem in older individuals. Surgical repair is the recommended treatment. Intraoperative hypotension (IOH) due to spinal anesthesia is common and may be associated with unfavorable outcomes. This study aimed to identify the incidence, risk factors, and outcomes of IOH in patients with hip fracture under spinal anesthesia.
Materials and Methods: Retrospective data from a Thai hospital (January 2018-December 2020) were reviewed. Patients over 50 who underwent hip surgery were included, excluding those receiving general anesthesia, with high-energy/pathological fractures, or multiple traumas. Patients were categorized into no-IOH and IOH groups, with outcome measures compared.
Results: In total, 264 patients were included for analysis. The mean age was 80.9 ± 8.3 years, with 77.3% females. The incidence of IOH was 37.9% [95% CI: 30.8%, 46.1%] and an independent risk factor was age > 65 years (OR [95% CI]: 6.23 [1.13, 34.47]. The two protective factors for IOH were higher preoperative mean arterial pressure (OR [95% CI]: 0.96 [0.93, 0.99]) and time from fracture to surgery > 24 hours (OR [95% CI]: 0.43 [0.21, 0.89]). Postoperative blood transfusions were administered more frequently (53.7%) in the IOH group than in the no-IOH group (37.9%, p = 0.014).
Conclusion: The incidence of intraoperative hypotension in hip fracture surgery was 38%. Aging is the only identified risk factor. IOH was related to a higher frequency of blood transfusion, but no other postoperative complications or mortality rates.
References
Wongtriratanachai P, Luevitoonvechkij S, Songpatanasilp T, Sribunditkul S, Leerapun T, Phadungkiat S, et al. Increasing incidence of hip fracture in Chiang Mai, Thailand. J Clin Densitom. 2013;16:347-52.
Sucharitpongpan W, Daraphongsataporn N, Saloa S, Philawuth N, Chonyuen P, Sriruanthong K, et al. Epidemiology of fragility hip fractures in Nan, Thailand. Osteoporos Sarcopenia. 2019;5:19-22.
Vaseenon T, Luevitoonvechkij S, Wongtriratanachai P, Rojanasthien S. Long-term mortality after osteoporotic hip fracture in Chiang Mai, Thailand. J Clin Densitom. 2010;13:63-7.
Daraphongsataporn N, Saloa S, Sriruanthong K, Philawuth N, Waiwattana K, Chonyuen P, et al. One-year mortality rate after fragility hip fractures and associated risk in Nan, Thailand. Osteoporos Sarcopenia. 2020;6:65-70.
Bhandari M, Swiontkowski M. Management of acute hip fracture. N Engl J Med. 2017;377:2053-62.
Griffiths R, Babu S, Dixon P, Freeman N, Hurford D, Kelleher E, et al. Guideline for the management of hip fractures 2020: Guideline by the Association of Anaesthetists. Anaesthesia. 2021;76:225-37.
Shelton C, White S. Anaesthesia for hip fracture repair. BJA Educ. 2020;20:142-9.
White SM, Moppett IK, Griffiths R, Johansen A, Wakeman R, Boulton C, et al. Secondary analysis of outcomes after 11,085 hip fracture operations from the prospective UK Anaesthesia Sprint Audit of Practice (ASAP-2). Anaesthesia. 2016;71:506-14.
Beecham G, Cusack R, Vencken S, Crilly G, Buggy DJ. Hypotension during hip fracture surgery and postoperative morbidity. Ir J Med Sci. 2020;189:1087-96.
Futier E, Lefrant J-Y, Guinot P-G, Godet T, Lorne E, Cuvillon P, et al. Effect of individualized vs standard blood pressure management strategies on postoperative organ dysfunction among high-risk patients undergoing major surgery: a randomized clinical trial. JAMA. 2017;318:1346-57.
Bijker JB, Van Klei WA, Kappen TH, Van Wolfswinkel L, Moons KG, Kalkman CJ. Incidence of intraoperative hypotension as a function of the chosen definition: literature definitions applied to a retrospective cohort using automated data collection. Anesthesiology. 2007;107:213-20.
Wesselink E, Kappen T, Torn H, Slooter A, Van Klei W. Intraoperative hypotension and the risk of postoperative adverse outcomes: a systematic review. Br J Anaesth. 2018;121:706-21.
Brady KM, Hudson A, Hood R, DeCaria B, Lewis C, Hogue CW. Personalizing the definition of hypotension to protect the brain. Anesthesiology. 2020;132:170-9.
Guay J, Parker MJ, Gajendragadkar PR, Kopp S. Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev. 2016;2:CD000521.
Kunutsor SK, Hamal PB, Tomassini S, Yeung J, Whitehouse MR, Matharu GS. Clinical effectiveness and safety of spinal anaesthesia compared with general anaesthesia in patients undergoing hip fracture surgery using a consensus-based core outcome set and patient-and public-informed outcomes: a systematic review and meta-analysis of randomised controlled trials. Br J Anaesth. 2022;129:788-800.
Memtsoudis SG, Cozowicz C, Bekeris J, Bekere D, Liu J, Soffin EM, et al. Anaesthetic care of patients undergoing primary hip and knee arthroplasty: consensus recommendations from the International Consensus on Anaesthesia-Related Outcomes after Surgery group (ICAROS) based on a systematic review and meta-analysis. Br J Anaesth. 2019;123:269-87.
Maxwell BG, Spitz W, Porter J. Association of Increasing Use of Spinal Anesthesia in Hip Fracture Repair with Treating an Aging Patient Population. JAMA Surg. 2020;155:167-8.
Cao MM, Zhang YW, Sheng RW, Gao W, Kang QR, Gao YC, et al. General anesthesia versus regional anesthesia in the elderly patients undergoing hip fracture surgeries: A systematic review and meta-analysis of randomized clinical trials. World J Surg. 2023;47:1444-56.
Carpenter RL, Caplan RA, Brown DL, Stephenson C, Wu R. Incidence and risk factors for side effects of spinal anesthesia. Anesthesiology. 1992;76:906-16.
Hartmann B, Junger A, Klasen J, Benson M, Jost A, Banzhaf A, et al. The incidence and risk factors for hypotension after spinal anesthesia induction: An analysis with automated data collection. Anesth Analg. 2002;94:1521-9.
Wijnberge M, Schenk J, Bulle E, Vlaar A, Maheshwari K, Hollmann M, et al. Association of intraoperative hypotension with postoperative morbidity and mortality: systematic review and meta-analysis. BJS open. 2021;5:zraa018.
Sheehan KJ, Guerrero EM, Tainter D, Dial B, Milton-Cole R, Blair JA, et al. Prognostic factors of in-hospital complications after hip fracture surgery: a scoping review. Osteoporos Int. 2019;30:1339-51.
Akarapatima R. The risk factors for spinal anesthesia-induced hypotension in patients undergoing hip Fracture surgery among the alderly: A retrospective cohort study. Thai J Anesthesiol. 2021;47:85-92.
Singla D, Kathuria S, Singh A, Kaul TK, Gupta S. Risk factors for development of early hypotension during spinal anaesthesia. J Anaesthesiol Clin Pharmacol. 2006;22:387-93.
Griffiths R, Beech F, Brown A, Dhesi J, Foo I, Goodall J, et al. Peri-operative care of the elderly 2014: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2014;69(Suppl 1):81-98.
Li T, Li J, Yuan L, Wu J, Jiang C, Daniels J, et al. Effect of Regional vs General Anesthesia on Incidence of Postoperative Delirium in Older Patients Undergoing Hip Fracture Surgery: The RAGA Randomized Trial. JAMA. 2022;327:50-8.
Chinachoti T, Saetia S, Chaisiri P, Tritrakarn T. Incidence and risk factors of hypotension and bradycardia during spinal anesthesia. Siriraj Med J. 2006;58:696-701.
Whiteside JB, Burke D, Wildsmith JA. Comparison of ropivacaine 0.5% (in glucose 5%) with bupivacaine 0.5% (in glucose 8%) for spinal anaesthesia for elective surgery. Br J Anaesth. 2003;90:304-8.
Mohta M. Ropivacaine: Is it a good choice for spinal anesthesia? J Anaesthesiol Clin Pharmacol. 2015;31:457-8.
Ferré F, Martin C, Bosch L, Kurrek M, Lairez O, Minville V. Control of Spinal Anesthesia-Induced Hypotension in Adults. Local Reg Anesth. 2020;13:39-46.
Staheli B, Rondeau B. Anesthetic Considerations in the Geriatric Population. Treasure Island (FL): StatPearls Publishing LLC.; 2023.
Barnett S. Anesthesia for the older adult. In: Joshi GP, Nussmeier NA, ed. UpToDate. Waltham: MA; 2022.
Messina A, La Via L, Milani A, Savi M, Calabrò L, Sanfilippo F, et al. Spinal anesthesia and hypotensive events in hip fracture surgical repair in elderly patients: a meta-analysis. J Anesth Analg Crit Care. 2022;2:19.
Ariyanuchitkul T. Preoperative risk factors of hypotension after spinal anesthesia for elective cesarean delivery in Maharat Nakhon Ratchasima Hospital. Thai J Anesthesiol. 2022;48:241-8.
Shitemaw T, Jemal B, Mamo T, Akalu L. Incidence and associated factors for hypotension after spinal anesthesia during cesarean section at Gandhi Memorial Hospital Addis Ababa, Ethiopia. PLoS One. 2020;15:e0236755.
Carpintero P, Caeiro JR, Carpintero R, Morales A, Silva S, Mesa M. Complications of hip fractures: A review. World J Orthop. 2014;5:402-11.
Fawcett WJ, Thomas M. Pre-operative fasting in adults and children: clinical practice and guidelines. Anaesthesia. 2019;74:83-8.
Yeniay O, Tekgul ZT, Okur O, Koroglu N. Unexpectedly prolonged fasting and its consequences on elderly patients undergoing spinal anesthetics. A prospective observational study1. Acta Cir Bras. 2019;34:e201900309.
Lindholm C, Sterner E, Romanelli M, Pina E, Torra y Bou J, Hietanen H, et al. Hip fracture and pressure ulcers - the Pan-European Pressure Ulcer Study - intrinsic and extrinsic risk factors. Int Wound J. 2008;5:315-28.
Sutipornpalangkul W, Harnroongroj T, Harnroongroj T. Intracapsular hip fractures have poorer nutritional status and more complications than trochanteric fractures: a retrospective study of 255 Thai patients. Siriraj Med J. 2010;62:1-3.
Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55:146-54.
Suenghataiphorn T, Songwisit S, Tornsatitkul S, Somnuke P. An overview on postoperative cognitive dysfunction; pathophysiology, risk factors, prevention and treatment. Siriraj Med J. 2022;74:705-13.
Xie R, Wang L, Bao H. Crystalloid and colloid preload for maintaining cardiac output in elderly patients undergoing total hip replacement under spinal anesthesia. J Biomed Res. 2011;25:185-90.
Bajwa SJ, Kulshrestha A, Jindal R. Co-loading or pre-loading for prevention of hypotension after spinal anaesthesia! a therapeutic dilemma. Anesth Essays Res. 2013;7:155-9.
Giannoulis D, Calori GM, Giannoudis PV. Thirty-day mortality after hip fractures: has anything changed? Eur J Orthop Surg Traumatol. 2016;26:365-70.
Royal College of Physicians. National Hip Fracture Database Annual Report Web site. Available from: https://www.nhfd.co.uk/2022report. [Accessed June 12, 2023].
Tan CMP, Park DH, Chen YD, Jagadish MU, Su S, Premchand AXR. Mortality rates for hip fracture patients managed surgically and conservatively in a dedicated unit in Singapore. Arch Orthop Trauma Surg. 2022;142:99-104.
Li D, Chang B, Yao P, Mao J. Application of the collaborative model for the treatment of elderly patients with hip fracture. Asian J Surg. 2023;46:2786-7.
The National Institute for Health and Care Excellence. Hip fracture Management Clinical Guideline 124 Web site. Available from: https://www.nice.org.uk/guidance/cg124/resources/hip-fracture-management-pdf-35109449902789. [Accessed June 12, 2023].
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














