Validation Study of the Postoperative Cognitive Dysfunction Database in Siriraj Hospital, Thailand
DOI:
https://doi.org/10.33192/smj.v76i7.268007Keywords:
Postoperative Cognitive Dysfunction, Validation study, Validate, Database, Risk factorsAbstract
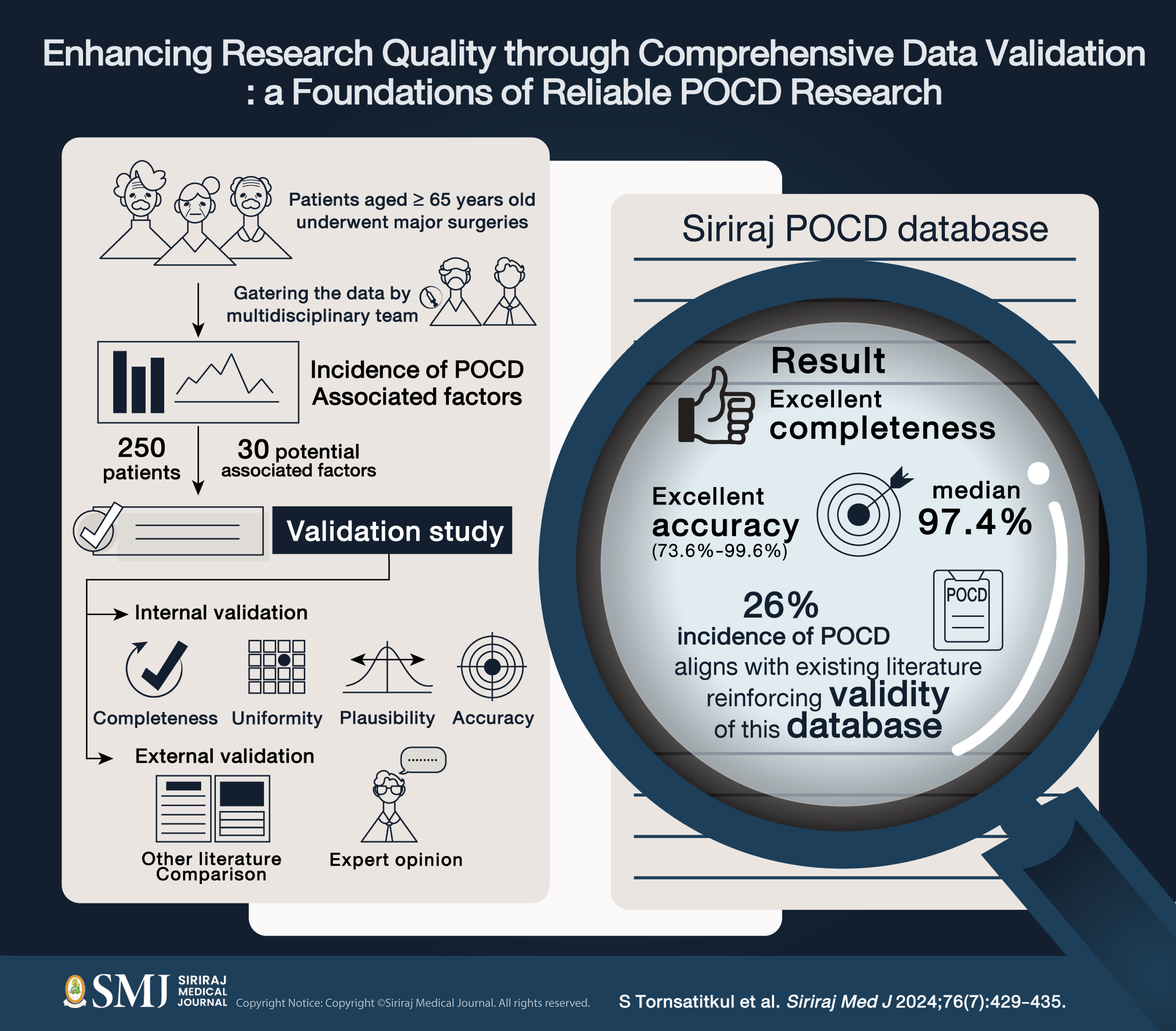
Objective: Postoperative Cognitive Dysfunction (POCD) is a complication that arises in the elderly. Because of the limited knowledge of POCD, researchers must handle a substantial amount of data to ensure the comprehensive collection of all relevant factors. To deal with this data, a validation study is a valuable method that aids in qualifying the data.
Materials and Methods: A validation exercise was performed for 40% of the data in the Siriraj POCD database (n=250) in 2020-2023. The validation covered 30 items, including demographic data, surgical and anesthetic factors. The validation study had two components: internal validation, which aimed to assess the completeness, uniformity, plausibility, and accuracy of the data in the database, and external validation, where the results were compared to external literature to confirm their correspondence.
Results: The completeness was 99.2% for creatinine and 94.0% for hemoglobin, while others showed 100% completeness. The accuracy ranged from 73.6% to 99.6%, with a median of 97.4%. Most errors found were related to “body weight”, followed by “hemoglobin levels” and “Propofol targeted controlled infusion”, with accuracy rates of 73.6%, 84.0%, and 85.2%, respectively. In the external validation, the POCD incidence at 1 week from surgery in the literature review ranged from 8.9%–46.1% compared to 26.0% in our study.
Conclusion: The Siriraj POCD cohort study database was found to be reasonably valid. Therefore, this data can support high-quality research. Our recommendations for developing a good database include implementing a dedicated plan, employing trained staff, and using reliable data sources.
References
Norkiene I, Samalavičius R, Misiuriene I, Paulauskiene K, Budrys V, Ivaškevičius J. Incidence and risk factors for early postoperative cognitive decline after coronary artery bypass grafting. Medicina. 2010;46(7):460-4. DOI: https://doi.org/10.3390/medicina46070066
Canet J, Raeder J, Rasmussen LS, Enlund M, Kuipers HM, Hanning CD, et al. Cognitive dysfunction after minor surgery in the elderly. Acta Anaesthesiol Scand. 2003;47(10):1204-10. DOI: https://doi.org/10.1046/j.1399-6576.2003.00238.x
Suenghataiphorn T, Songwisit S, Tornsatitkul S, Somnuke P. An Overview on Postoperative Cognitive Dysfunction; Pathophysiology, Risk Factors, Prevention and Treatment. Siriraj Med J. 2022;74(10):705-13. DOI: https://doi.org/10.33192/Smj.2022.82
Wang W, Feng N, Zhao W, Luo F, Zhu X, Zhao W, et al. Dexmedetomidine reduces brain neuronal injuries but not clinical neurocognitive function in the elderly, compared to midazolam. Int J Clin Exp Med. 2019;12(4):4210-7.
Steinmetz J, Rasmussen LS. Peri-operative cognitive dysfunction and protection. Anaesthesia. 2016;71 Suppl 1:58-63. DOI: https://doi.org/10.1111/anae.13308
Brodier EA, Cibelli M. Postoperative cognitive dysfunction in clinical practice. BJA Educ. 2021;21(2):75-82. DOI: https://doi.org/10.1016/j.bjae.2020.10.004
Hoeven LRV, Bruijne MC, Kemper PF, Koopman MMW, Rondeel JMM, Leyte A, et al. Validation of multisource electronic health record data: an application to blood transfusion data. BMC Med Inform Decis Mak. 2017;17(1):107. DOI: https://doi.org/10.1186/s12911-017-0504-7
Herrett E, Thomas SL, Schoonen WM, Smeeth L, Hall AJ. Validation and validity of diagnoses in the General Practice Research Database: a systematic review. Br J Clin Pharmacol. 2010;69(1):4-14. DOI: https://doi.org/10.1111/j.1365-2125.2009.03537.x
Silbert B, Evered L, Scott DA, McMahon S, Choong P, Ames D, et al. Preexisting Cognitive Impairment Is Associated with Postoperative Cognitive Dysfunction after Hip Joint Replacement Surgery. Anesthesiology. 2015;122(6):1224-34. DOI: https://doi.org/10.1097/ALN.0000000000000671
Feinkohl I, Winterer G, Pischon T. Diabetes is associated with risk of postoperative cognitive dysfunction: A meta-analysis. Diabetes Metab Res Rev. 2017;33(5). DOI: https://doi.org/10.1002/dmrr.2884
Feinkohl I, Winterer G, Pischon T. Hypertension and Risk of Post-Operative Cognitive Dysfunction (POCD): A Systematic Review and Meta-Analysis. Clin Pract Epidemiol Ment Health. 2017;13:27-42. DOI: https://doi.org/10.2174/1745017901713010027
Goldberg TE, Chen C, Wang Y, Jung E, Swanson A, Ing C, et al. Association of delirium with long-term cognitive decline: A meta-analysis. JAMA Neurology. 2020;77(11):1373-81. DOI: https://doi.org/10.1001/jamaneurol.2020.2273
Yang W, Kong LS, Zhu XX, Wang RX, Liu Y, Chen LR. Effect of dexmedetomidine on postoperative cognitive dysfunction and inflammation in patients after general anaesthesia: A PRISMA-compliant systematic review and meta-analysis. Medicine (United States)d. 2019;98(18). DOI: https://doi.org/10.1097/MD.0000000000015383
Mansouri N, Nasrollahi K, Shetabi H. Prevention of Cognitive Dysfunction after Cataract Surgery with Intravenous Administration of Midazolam and Dexmedetomidine in Elderly Patients Undergoing Cataract Surgery. Adv Biomed Res. 2019;8(1):6. DOI: https://doi.org/10.4103/abr.abr_190_18
Punjasawadwong Y, Chau-In W, Laopaiboon M, Punjasawadwong S, Pin-On. Processed electroencephalogram and evoked potential techniques for amelioration of postoperative delirium and cognitive dysfunction following non-cardiac and non-neurosurgical procedures in adults. Cochrane Database Syst Rev. 2018;5(5):CD011283. DOI: https://doi.org/10.1002/14651858.CD011283.pub2
Ortega-Loubon C, Herrera-Gómez F, Bernuy-Guevara C, Jorge-Monjas P, Ochoa-Sangrador C, Bustamante-Munguira J, et al. Near-infrared spectroscopy monitoring in cardiac and noncardiac surgery: Pairwise and network meta-analyses. J Clin Med. 2019;8(12):2208. DOI: https://doi.org/10.3390/jcm8122208
Zhu SH, Ji MH, Gao DP, Li WY, Yang JJ. Association between perioperative blood transfusion and early postoperative cognitive dysfunction in aged patients following total hip replacement surgery. Ups J Med Sci. 2014;119(3):262-7. DOI: https://doi.org/10.3109/03009734.2013.873502
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














