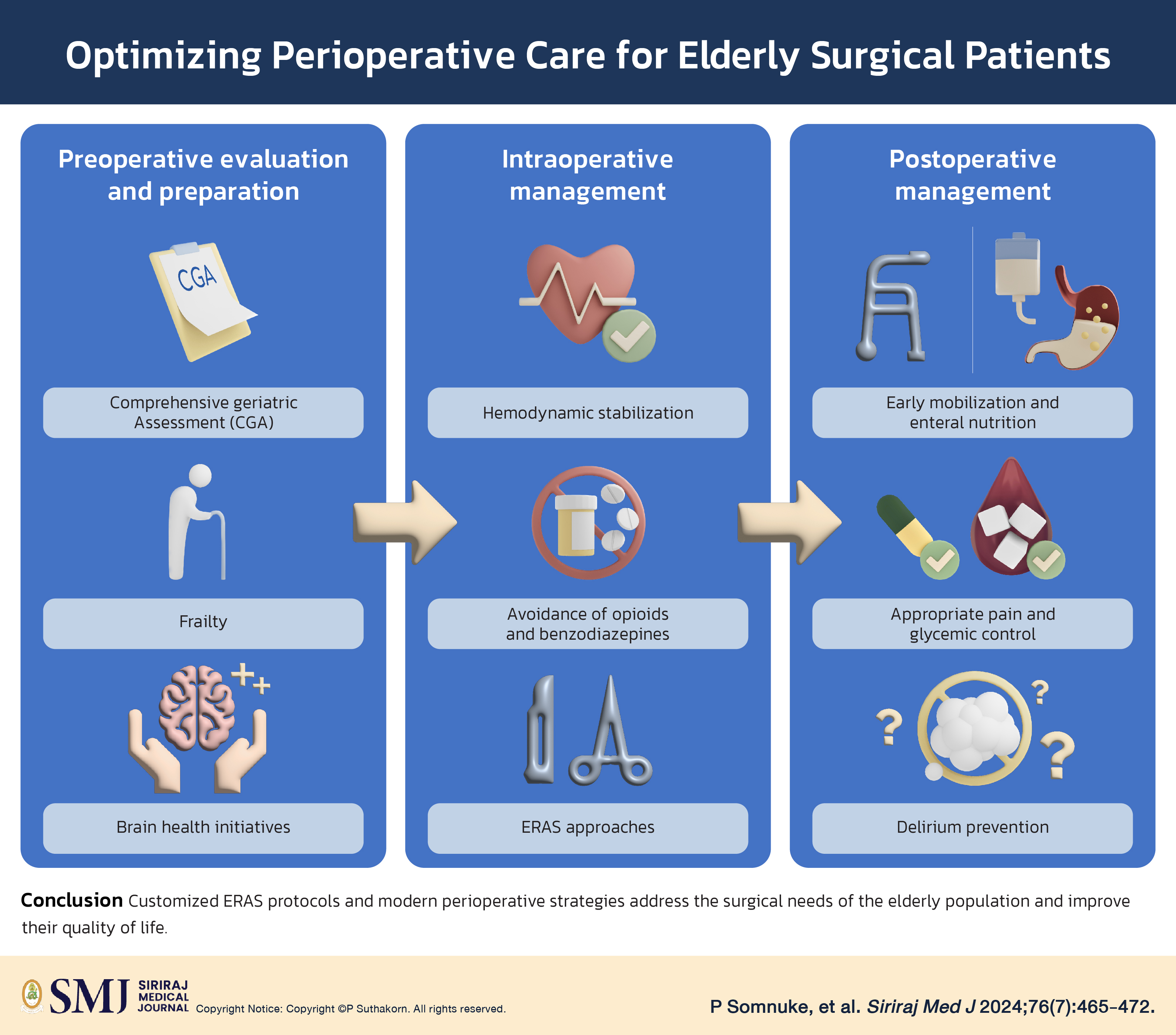
Optimizing Perioperative Care for Elderly Surgical Patients: A Review of Strategies and Evidence-Based Practices
DOI:
https://doi.org/10.33192/smj.v76i7.268063Keywords:
Elderly, Perioperative, Assessment, Cognitive function, Enhanced recovery after surgery (ERAS)Abstract
Thailand has transitioned into an aging society characterized by a notable demographic shift toward senior citizens. This demographic trend underscores the imperative of addressing age-related challenges. The aging process accounts for the progressive deterioration of physical and cognitive functions, often necessitating medical interventions such as medications or surgical procedures. As the elderly population continues to grow, prioritizing strategies to enhance quality of life and mitigate the onset of physical and cognitive impairments becomes increasingly crucial. Prudent patient care is paramount due to the heightened vulnerability of elderly patients and the elevated risk of adverse health outcomes. This review aimed to examine perioperative evaluation and optimization strategies tailored specifically for elderly individuals scheduled for surgery. Special emphasis was placed on preserving postoperative functional capacity and cognitive acuity among this group of patients.
References
World Health Organization. Thailand’s leadership and innovations towards healthy ageing. WHO. 2023. [cited 2024 Feb 26]. Available from:https://www.who.int/southeastasia/news/feature-stories/detail/thailands-leadership-and-innovation-towards-healthy-ageing.
Economic and Social Commission for Asia and the Pacific Social Development. Ageing Societies. ESCAP. 2023. [cited 2024 Feb 26]. Available from: https://www.unescap.org/our-work/social-development/ageing-societies.
Statista. Resident population in Thailand as of July 2023, by age group (in millions). Statista. 2023. [cited 2024 Feb 26]. Available from: https://www.statista.com/statistics/1283627/thailand-resident-population-by-age-group/.
Yang R, Wolfson M, Lewis MC. Unique Aspects of the Elderly Surgical Population: An Anesthesiologist’s Perspective. Geriatr Orthop Surg Rehabil. 2011;2(2):56-64.
Fabbri E, Zoli M, Gonzalez-Freire M, Salive ME, Studenski SA, Ferrucci L. Aging and Multimorbidity: New Tasks, Priorities, and Frontiers for Integrated Gerontological and Clinical Research. J Am Med Dir Assoc. 2015;16(8):640-7.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752-62.
Wang X, Hu J, Wu D. Risk factors for frailty in older adults. Medicine (Baltimore). 2022;101(34):e30169.
Welsh TJ, Gordon AL, Gladman JR. Comprehensive geriatric assessment--a guide for the non-specialist. Int J Clin Pract. 2014;68(3):290-3.
Charlson ME, Carrozzino D, Guidi J, Patierno C. Charlson Comorbidity Index: A Critical Review of Clinimetric Properties. Psychother Psychosom. 2022;91(1):8-35.
Salvi F, Miller MD, Grilli A, Giorgi R, Towers AL, Morichi V, et al. A Manual of Guidelines to Score the Modified Cumulative Illness Rating Scale and Its Validation in Acute Hospitalized Elderly Patients. J Am Geriatr Soc. 2008;56:1926-31.
Sheikh-Taha M, Asmar M. Polypharmacy and severe potential drug-drug interactions among older adults with cardiovascular disease in the United States. BMC Geriatr. 2021;21(1):233.
Ryg J, Engberg H, Mariadas P, Pedersen SGH, Jorgensen MG, Vinding KL, et al. Barthel Index at hospital admission is associated with mortality in geriatric patients: a Danish nationwide population-based cohort study. Clin Epidemiol. 2018;10:1789-1800.
Graf C. The Lawton instrumental activities of daily living scale. Am J Nurs. 2008;108(4):52-62
Suenghataiphorn T, Songwisit S, Tornsatitkul S, Somnuke P. An Overview on Postoperative Cognitive Dysfunction; Pathophysiology, Risk Factors, Prevention and Treatment. Siriraj Med J. 2022;74(10):705-13.
Pezzotti P, Scalmana S, Mastromattei A, Di Lallo D; Progetto Alzheimer Working Group. The accuracy of the MMSE in detecting cognitive impairment when administered by general practitioners: a prospective observational study. BMC Fam Pract. 2008;9:29.
Yang C, Wang L, Hu H, Dong X, Wang Y, Yang F. Montreal Cognitive Assessment: Seeking a Single Cutoff Score May Not Be Optimal. Evid Based Complement Alternat Med. 2021;2021:9984419.
Somnuke P, Srishewachart P, Jiraphorncharas C, Khempetch A, Weeranithan J, Suraarunsumrit P, et al. Early postoperative neurocognitive complications in elderly patients: comparing those with and without preexisting mild cognitive impairment- a prospective study. BMC Geriatr. 2024;24(1):84.
Schreiner AS, Hayakawa H, Morimoto T, Kakuma T. Screening for late life depression: cut-off scores for the Geriatric Depression Scale and the Cornell Scale for Depression in Dementia among Japanese subjects. Int J Geriatr Psychiatry. 2003;18(6):498-505.
Guigoz Y. The Mini Nutritional Assessment (MNA) review of the literature--What does it tell us? J Nutr Health Aging. 2006 Nov-Dec;10(6):466-85.
Strini V, Schiavolin R, Prendin A. Fall Risk Assessment Scales: A Systematic Literature Review. Nurs Rep. 2021;11(2):430-43.
Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80(9):896-903.
Wood BM, Nicholas MK, Blyth F, Asghari A, Gibson S. Assessing pain in older people with persistent pain: the NRS is valid but only provides part of the picture. J Pain. 2010;11(12):1259-66.
Aicher B, Peil H, Peil B, Diener HC. Pain measurement: Visual Analogue Scale (VAS) and Verbal Rating Scale (VRS) in clinical trials with OTC analgesics in headache. Cephalalgia. 2012;32(3):185-97.
Shuman-Paretsky MJ, Belser-Ehrlich J, Holtzer R. Psychometric properties of the Brief Fatigue Inventory in community-dwelling older adults. Arch Phys Med Rehabil. 2014;95(8):1533-9.
Merino-Soto C, Núñez Benítez MÁ, Domínguez-Guedea MT, Toledano-Toledano F, Moral de la Rubia J, Astudillo-García CI, et al. Medical outcomes study social support survey (MOS-SSS) in patients with chronic disease: A psychometric assessment. Front Psychiatry. 2023;13:1028342.
Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001;286(21):2703-10.
Evensen S, Hylen Ranhoff A, Lydersen S, Saltvedt I. The delirium screening tool 4AT in routine clinical practice: prediction of mortality, sensitivity and specificity. Eur Geriatr Med. 2021;12(4):793-800.
Gaudreau JD, Gagnon P, Harel F, Tremblay A, Roy MA. Fast, systematic, and continuous delirium assessment in hospitalized patients: the nursing delirium screening scale. J Pain Symptom Manage. 2005;29(4):368-75.
Somnuke P, Limprapassorn P, Srinonprasert V, Wongviriyawong T, Suraarunsumrit P, Morkphrom E, et al. The Thai version of the nursing delirium screening scale-Thai: Adaptation and validation study in postoperative patients. Front Med (Lausanne). 2022;9:956435.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al; Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146-56.
Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16(7):601-8.
Sriwong WT, Mahavisessin W, Srinonprasert V, Siriussawakul A, Aekplakorn W, Limpawattana P, et al. Validity and reliability of the Thai version of the simple frailty questionnaire (T-FRAIL) with modifications to improve its diagnostic properties in the preoperative setting. BMC Geriatr. 2022;22(1):161.
Navarro-Flores E, de Bengoa Vallejo RB, Losa-Iglesias ME, Palomo-López P, Calvo-Lobo C, López-López D, et al. The reliability, validity, and sensitivity of the Edmonton Frail Scale (EFS) in older adults with foot disorders. Aging (Albany NY). 2020;12(24):24623-24632.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489-95.
Raîche M, Hébert R, Dubois MF. PRISMA-7: a case-finding tool to identify older adults with moderate to severe disabilities. Arch Gerontol Geriatr. 2008;47(1):9-18.
Turner G, Clegg A; British Geriatrics Society; Age UK; Royal College of General Practioners. Best practice guidelines for the management of frailty: a British Geriatrics Society, Age UK and Royal College of General Practitioners report. Age Ageing. 2014 No;43(6):744-7.
Sabayan B, Westendorp RGJ. Neurovascular-glymphatic dysfunction and white matter lesions. Geroscience. 2021;43(4):1635-42.
Cole JH, Marioni RE, Harris SE, Deary IJ. Brain age and other bodily ‘ages’: implications for neuropsychiatry. Mol Psychiatry. 2019;24(2):266-81.
Agarwal P, Panda AK, Jena S, Mohapatra S. Correlation of Cerebral Atrophy and White Matter Hyperintensity Burden in MRI with Clinical Cognitive Decline. Siriraj Med J. 2022;74(5):323-9.
Sabayan B, Doyle S, Rost NS, Sorond FA, Lakshminarayan K, Launer LJ. The role of population-level preventive care for brain health in ageing. Lancet Healthy Longev. 2023;4(6):e274-e283.
Stern Y, Blumen HM, Rich LW, Richards A, Herzberg G, Gopher D. Space Fortress game training and executive control in older adults: a pilot intervention. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. 2011;18(6):653-77.
Mintzer J, Donovan KA, Kindy AZ, Lock SL, Chura LR, Barracca N. Lifestyle Choices and Brain Health. Front Med (Lausanne). 2019;6:204.
Scarmeas N, Stern Y, Tang MX, Mayeux R, Luchsinger JA. Mediterranean diet and risk for Alzheimer’s disease. Ann Neurol. 2006;59(6):912-21.
Männikkö R, Komulainen P, Schwab U, Heikkilä HM, Savonen K, Hassinen M, et al. The Nordic diet and cognition--The DR’s EXTRA Study. Br J Nutr. 2015;114(2):231-9.
Miyagi S, Iwama N, Kawabata T, Hasegawa K. Longevity and diet in Okinawa, Japan: the past, present and future. Asia Pac J Public Health. 2003;15 Suppl:S3-9.
Chmelo J, Chmelová I, Phillips AW. Prehabilitation, improving postoperative outcomes. Rozhl Chir. 2021;100(9):421-8.
Rivera R, Antognini JF. Perioperative drug therapy in elderly patients. Anesthesiology. 2009;110(5):1176-81.
Irwin MG, Ip KY, Hui YM. Anaesthetic considerations in nonagenarians and centenarians. Curr Opin Anaesthesiol. 2019;32(6):776-82.
Aceto P, Antonelli Incalzi R, Bettelli G, Carron M, Chiumiento F, Corcione A, et al. Perioperative Management of Elderly patients (PriME): recommendations from an Italian intersociety consensus. Aging Clin Exp Res. 2020;32(9):1647-73.
Liu B, Liu S, Zheng T, Lu D, Chen L, Ma T, et al. Neurosurgical enhanced recovery after surgery ERAS for geriatric patients undergoing elective craniotomy: A review. Medicine (Baltimore). 2022;101(33):e30043.
Ljungqvist O, Hubner M. Enhanced recovery after surgery-ERAS-principles, practice and feasibility in the elderly. Aging Clin Exp Res. 2018;30(3):249-52.
Millan M. Enhanced recovery after surgery in elderly and high-risk patients. Ann Laparosc Endosc Surg. 2020;5:39.
Zaed I, Marchi F, Milani D, Cabrilo I, Cardia A. Role of Enhanced Recovery after Surgery (ERAS) Protocol in the Management of Elderly Patients with Glioblastoma. J Clin Med. 2023;12(18):6032.
Zhu W, Yan Y, Sun Y, Fan Z, Fang N, Zhang Y, et al. Implementation of Enhanced Recovery After Surgery (ERAS) protocol for elderly patients receiving surgery for intertrochanteric fracture: a propensity score-matched analysis. J Orthop Surg Res. 2021;16(1):469.
Heng G, Lohsiriwat V, Tan K-Y. Suitability of Enhanced Recovery after Surgery (ERAS) Protocols for Elderly Colorectal Cancer Patients. Siriraj Med J. 2019;72(1):18-23.
Lohsiriwat V, Jaturanon P. Effect of Intraoperative Hypothermia on Surgical Outcomes after Colorectal Surgery within an Enhanced Recovery after Surgery Pathway. Siriraj Med J. 2019;71(1):52-8.
Herzig SJ, Anderson TS, Jung Y, Ngo L, Kim DH, McCarthy EP. Relative risks of adverse events among older adults receiving opioids versus NSAIDs after hospital discharge: A nationwide cohort study. PLoS Med. 2021;18(9):e1003804.
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














