Effectiveness of Smartphone Applications vs Conventional Care in Warfarin Therapy: A Randomized Controlled Trial on the Time in the Therapeutic Range
DOI:
https://doi.org/10.33192/smj.v76i7.268122Keywords:
Warfarin, smartphone, application, patient compliance, anticoagulationAbstract
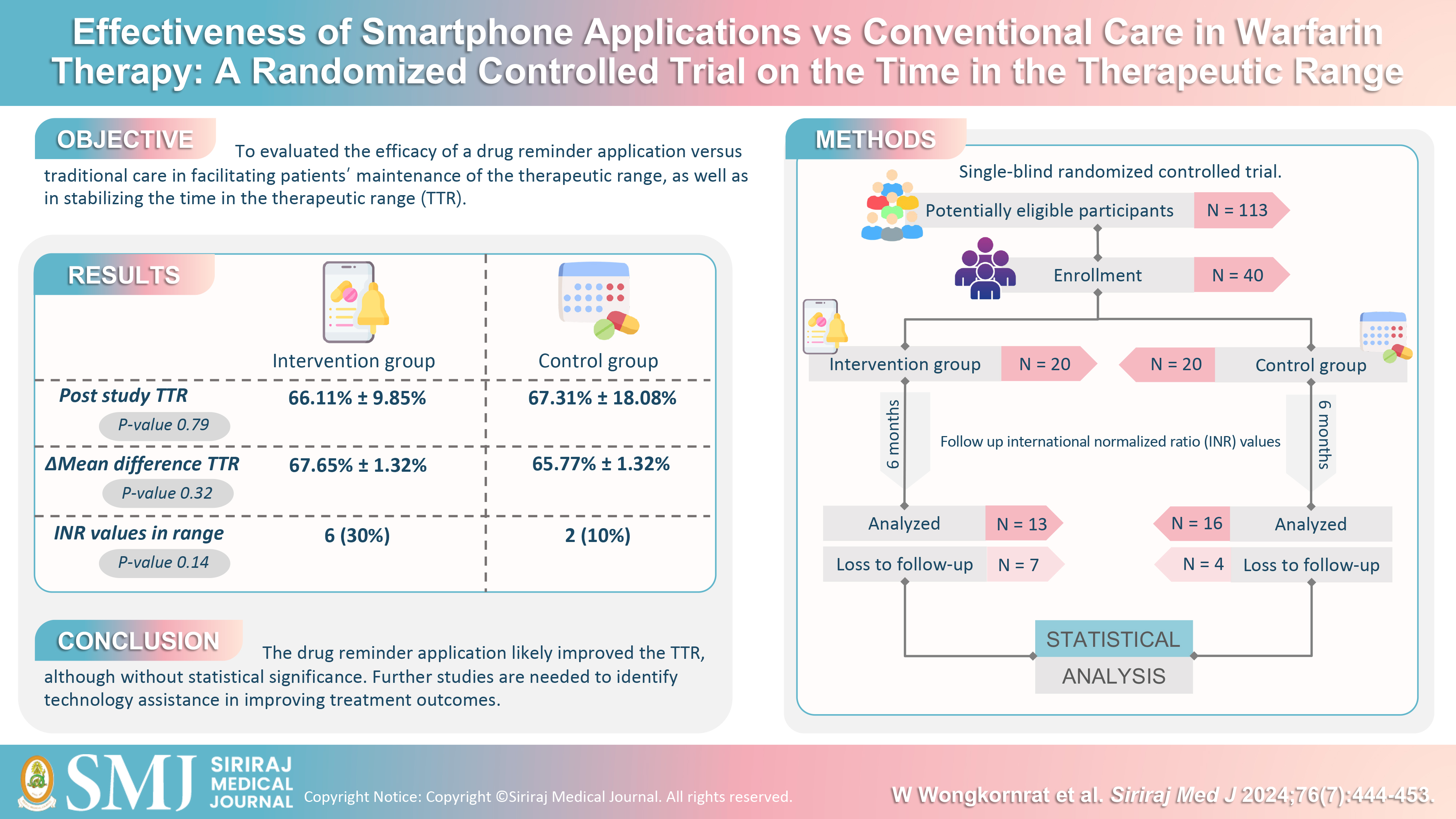
Objective: Warfarin is extensively used as an oral anticoagulant; however, its clinical application is complicated by a narrow therapeutic index. This investigation evaluated the efficacy of a drug reminder application versus traditional care in facilitating patients’ maintenance of the therapeutic range, as well as in stabilizing the time in the therapeutic range (TTR).
Material and Methods: A single-blind randomized controlled trial recruited 40 warfarin users (≥3 months) with stable INR for 6 months. The intervention group received a smartphone app reminder. All INR values were collected for 6 months. Primary outcomes were TTR, INR, TTR during drug-drug interactions, and warfarin complications.
Results: Forty patients were recruited between January 2021 and August 2023. The mean TTR was 66.11%±9.8% for the intervention group and 67.31%±18.08% for the control group. With analysis of covariance, the results were slightly better in the intervention group, but the differences were not statistically significant (95%CI = -5.67 – 1.92, P-value = 0.323). For the 6-month INR monitoring, 6 out of 8 patients who could maintain the therapeutic INR range were in the intervention group. There were no statistically significant differences in warfarin-related complications between the two groups (20% vs 15%, RR 1.333, 95%CI = 0.3413 – 5.2086, P-value = 0.6790).
Conclusion: The drug reminder application likely improved the TTR, although without statistical significance. Further studies are needed to identify technology assistance in improving treatment outcomes.
References
Chen WC, Chen YH, Hsu PI, Tsay FW, Chan HH, Cheng JS, et al. Gastrointestinal Hemorrhage in Warfarin Anticoagulated Patients: Incidence, Risk Factor, Management, and Outcome. BioMed Res Int. 2014;2014:463767.
Kotirum S, Chaiyakunapruk N, Jampachaisri K, Wattanasombat S, Rojnuckarin P. Utilization review of concomitant use of potentially interacting drugs in Thai patients using warfarin therapy. Pharmacoepidemiol Drug Saf. 2007;16(2):216-22.
Zhao S, Zhao H, Wang X, Gao C, Qin Y, Cai H, et al. Factors influencing medication knowledge and beliefs on warfarin adherence among patients with atrial fibrillation in China. Patient Preference and Adherence [Internet]. 2017 [cited 2021 Aug 15];11:213-20. Available from: https://pubmed.ncbi.nlm.nih.gov/28223782/#article-details
Krittathanmakul S, Silapachote P, Pongwecharak J, Wongsatit U. Effects of pharmacist counseling on outpatients receiving warfarin at Songklanagarind Hospital. Songkla Med J. 2006;24(2):93-99.
Boonbaichaiyapruck S, Panchavinnin P, Suthichaiyakul T, Benjanuwatra T, Sukanandachai B, Mahawanakul W, et al. Behavior of Prothrombin Time (INR) in Response to Warfarin Therapy in a Thai Population. Thai Heart Journal. 2006;19(3):85-9.
Priksri W, Rattanavipanon W, Saejear W, Tanyasaensook K, Phrommintikul A, Chulavatnatol S, et al. Incidence, risk factors, and outcomes of warfarin-associated major bleeding in Thai population. Pharmacoepidemiol Drug Saf. 2019;28(7):942-50.
Uaprasert N, editor. Treatment of venous thromboembolism in the era of non-vitamin K antagonist oral anticoagulants. Thai Heart Journal. 2015;98(1):111-7.
Dilokthornsakul P, Nathisuwan S, Krittayaphong R, Chutinet A, Permsuwan U. Cost-Effectiveness Analysis of Non-Vitamin K Antagonist Oral Anticoagulants Versus Warfarin in Thai Patients With Non-Valvular Atrial Fibrillation. Heart Lung Circ. 2020;29(3):390-400.
Kim JH, Song YB, Shin DH, Kim JS, Choi JO, On YK, et al. How Well Does the Target INR Level Maintain in Warfarin-Treated Patients with Non-Valvular Atrial Fibrillation? Yonsei Med J. 2009;50(1):83-8.
Waterman AD, Milligan PE, Bayer L, Banet GA, Gatchel SK, Gage BF. Effect of warfarin nonadherence on control of the International Normalized Ratio. Am J Health Syst Pharm. 2004;61(12):1258-64.
Ghaswalla PK, Harpe SE, Tassone D, Slattum PW. Warfarin-antibiotic interactions in older adults of an outpatient anticoagulation clinic. Am J Geriatr Pharmacother. 2012;10(6):352-60.
Platt AB, Localio AR, Brensinger CM, Cruess DG, Christie JD, Gross R, et al. Risk factors for nonadherence to warfarin: results from the IN-RANGE study. Pharmacoepidemiol Drug Saf. 2008;17(9):853-60.
Aidit S, Soh YC, Yap CS, Khan TM, Neoh CF, Shaharuddin S, et al. Effect of Standardized Warfarin Treatment Protocol on Anticoagulant Effect: Comparison of a Warfarin Medication Therapy Adherence Clinic with Usual Medical Care. Front Pharmacol. 2017;8:637.
Falamić S, Lucijanić M, Hadžiabdić MO, Marušić S, Bačić Vrca V. Pharmacist’s interventions improve time in therapeutic range of elderly rural patients on warfarin therapy: a randomized trial. Int J Clin Pharm. 2018;40(5):1078-85.
Sudas Na Ayutthaya N, Sakunrak I, Dhippayom T. Clinical Outcomes of Telemonitoring for Patients on Warfarin after Discharge from Hospital. Int J Telemed Appl. 2018;2018:7503421.
Li Y, Dong L, Xiang D, Zhang Y, Chen X, Long J, et al. Patient compliance with an anticoagulation management system based on a smartphone application. J Thromb Thrombolysis. 2019;48(2):263-9.
Gateman D, Melissa Elizabeth Trojnar, Agarwal G. Time in therapeutic range: Warfarin anticoagulation for atrial fibrillation in a community-based practice. Can Fam Physician. 2017;63(10):e425-31.
Reiffel J. Time in the Therapeutic Range (TTR): An Overly Simplified Conundrum. J Innov Card Rhythm Manag. 2017;8(3):2643-6.
WARFARIN: MANAGEMENT OF OUT-OF-RANGE INRS OBJECTIVE: BACKGROUND [Internet]. 2020. [cited 2024 Mar. 23]. Available from: https://thrombosiscanada.ca/wp-content/uploads/2021/01/16.-Warfarin-Out-of-Range-INR_31July2020.pdf
Crader MF, Johns T, Arnold JK. Warfarin Drug Interactions [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2022. [cited 2024 Mar. 23]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441964
Chartrungsan A, Laksanabunsong P, Nimmannit A, Suwanawiboon B, Poungvarin N, Wongkornrat W, et al. Comparison of Temporary Interruption of Warfarin Therapy for 3 and 5 days before Surgery in Thailand: A Randomized Controlled Trial. Siriraj Med J [Internet]. 2017 Apr. 4 [cited 2024 Mar. 23];65(3):69-72. Available from: https://he02.tci-thaijo.org/index.php/sirirajmedj/article/view/82143
Kimmel SE. The Influence of Patient Adherence on Anticoagulation Control With Warfarin. Arch Intern Med. 2007;167(3):229-35.
Trachtenberg F, Dugan E, Hall MA. How patients’ trust relates to their involvement in medical care. The Journal of Family Practice [Internet]. 2005 Apr 1 [cited 2024 Mar. 23];54(4):344–52. Available from: https://pubmed.ncbi.nlm.nih.gov/15833226/
Smith VA, Coffman CJ, Hudgens MG. Interpreting the Results of Intention-to-Treat, Per-Protocol, and As-Treated Analyses of Clinical Trials. JAMA. 2021;326(5):433.
Siddiqui S, DeRemer CE, Waller JL, Gujral JS. Variability in the Calculation of Time in Therapeutic Range for the Quality Control Measurement of Warfarin. J Innov Card Rhythm Manag. 2018;9(12):3428-34.
IBM Corp. Released 2021. IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY: IBM Corp
Katchamart W, Narongroeknawin P. Drug Diary - Apps on Google Play [Internet]. play.google.com. Available from: https://play.google.com/store/apps/details?id=com.thaimedreminder.reminder
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














