Incidence and Factors Associated with Breastfeeding at Six Months in Very-Low-Birthweight Infants: A Single-Center Prospective Study
DOI:
https://doi.org/10.33192/smj.v76i8.268307Keywords:
Breastfeeding, cesarean section, maternal education, hospital discharge, very-low birthweight infantsAbstract
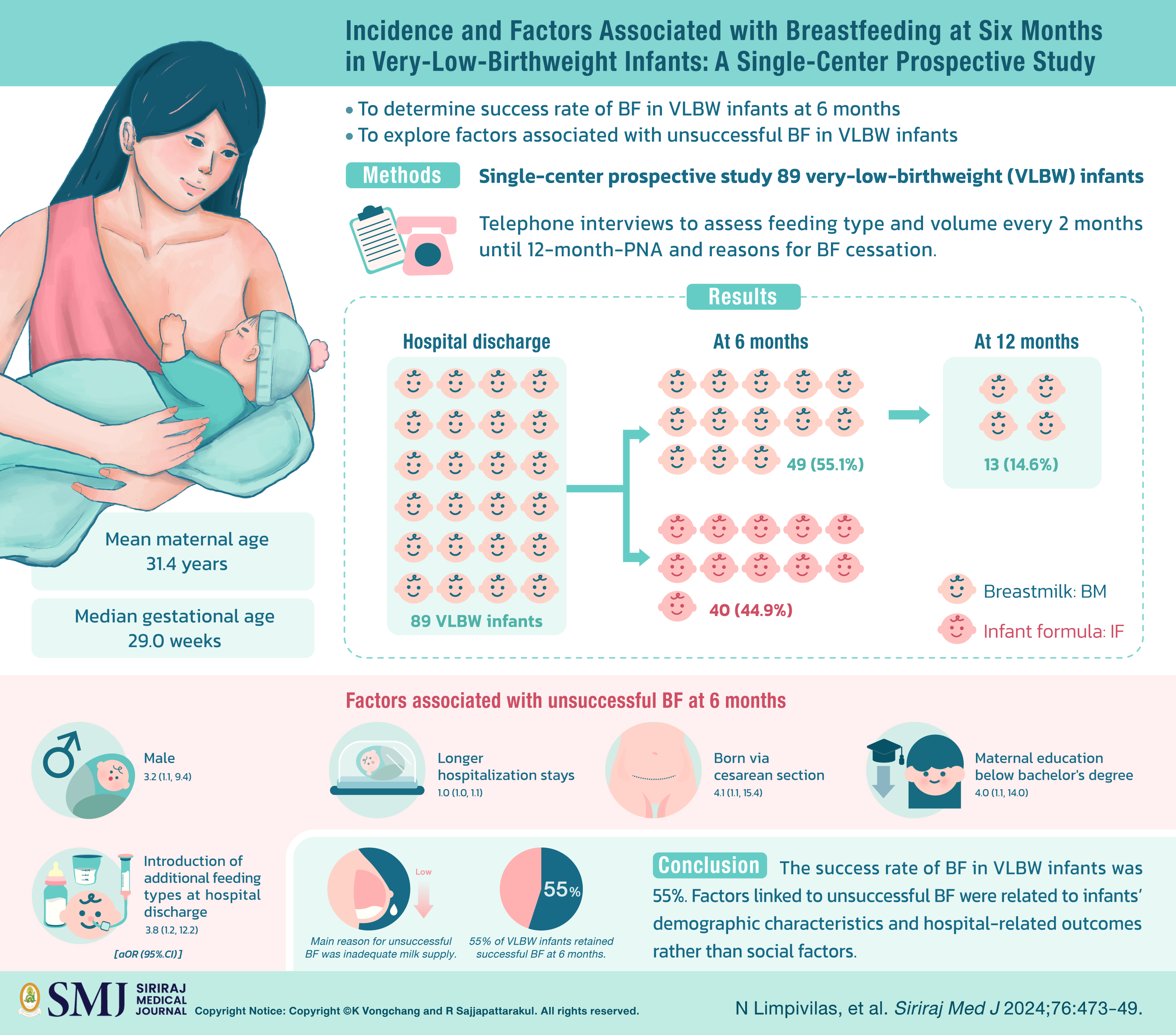
Objective: Primary objective was to determine success rate of breastfeeding (BF) at 6-month-postnatal age (PNA). Secondary objective was to explore factors associated with unsuccessful BF at 6-month-PNA in very-low-birthweight (VLBW) infants.
Materials and Methods: Single-center, prospective, observational study was conducted. Inclusion criteria were discharged VLBW infants and maternal desire for BF. We conducted telephone interviews to assess feeding type and volume every 2 months until 12-month-PNA and reasons for BF cessation.
Results: Eighty-nine VLBW infants were included. Mean (±standard deviation) maternal age was 31.4 ± 6.5 years. Median [P25, P75] gestational age was 29.0 [28.0, 31.5] weeks. At 6-month-PNA, 22 infants (24.7%) were exclusively breastfed, which decreased to 2 infants (2.2%) by 12 months. Rate of successful BF at 6 months was 55.1%. After controlling for potential confounders, factors associated with unsuccessful BF at 6 months were male [aOR (95% CI) 3.2 (1.1, 9.4), p = 0.04], longer hospitalization stays [aOR 1.0 (1.0, 1.1), p = 0.02], born via cesarean section [aOR 4.1 (1.1, 15.4), p = 0.04], maternal education below bachelor's degree [aOR 4.0 (1.1, 14.0), p = 0.03], and introduction of additional feeding types at hospital discharge [aOR 3.8 (1.2, 12.2), p = 0.03]. Main reason for unsuccessful breastfeeding at 6 months was inadequate milk supply (77.5%).
Conclusion: Fifty-five percent of VLBW infants retained successful BF at 6 months. Main reason for unsuccessful BF was inadequate milk supply.
References
Agostoni C, Braegger C, Decsi T, Kolacek S, Koletzko B, Michaelsen KF, et al. Breast-feeding: A commentary by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2009;49(1):112-25.
Hou L, Li X, Yan P, Li Y, Wu Y, Yang Q, et al. Impact of the duration of breastfeeding on the intelligence of children: a systematic review with network meta-analysis. Breastfeed Med. 2021;16(9):687-96.
Kramer MS, Kakuma R. Optimal duration of exclusive breastfeeding. Cochrane Database Syst Rev. 2012;2012(8):Cd003517.
Jedrychowski W, Perera F, Jankowski J, Butscher M, Mroz E, Flak E, et al. Effect of exclusive breastfeeding on the development of children's cognitive function in the Krakow prospective birth cohort study. Eur J Pediatr. 2012;171(1):151-8.
Eidelman AI, Schanler RJ, Johnston M, Landers S, Noble L, Szucs K, et al. Section on breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):e827-41.
World Health Organization. Global strategy for infant and young child feeding. Geneva: WHO; 2003.
World Health Organization. WHO recommendations for care of the preterm or low birth weight infant. Geneva: WHO; 2022.
World Health Organization. Guidelines on optimal feeding of low birth-weight infants in low- and middle-income countries. Geneva: WHO; 2011.
Bharwani SK, Green BF, Pezzullo JC, Bharwani SS, Bharwani SS, Dhanireddy R. Systematic review and meta-analysis of human milk intake and retinopathy of prematurity: a significant update. J Perinatol. 2016;36(11):913-20.
Abrams SA, Schanler RJ, Lee ML, Rechtman DJ. Greater mortality and morbidity in extremely preterm infants fed a diet containing cow milk protein products. Breastfeed Med. 2014;9(6):281-5.
Alshaikh B, Kostecky L, Blachly N, Yee W. Effect of a quality improvement project to use exclusive mother's own milk on rate of necrotizing enterocolitis in preterm infants. Breastfeed Med. 2015;10(7):355-61.
Lechner BE, Vohr BR. Neurodevelopmental outcomes of preterm infants fed human milk: a systematic review. Clin Perinatol. 2017;44(1):69-83.
United Nations Children’s Fund. Breastfeeding [internet]. New York: UNICEF; 2022 [cited 2022 Nov 18]. Available from: https://data.unicef.org/topic/nutrition/breastfeeding/.
Lechosa-Muñiz C, Paz-Zulueta M, Sota SM, de Adana Herrero MS, del Rio EC, Llorca J, et al. Factors associated with duration of breastfeeding in Spain: a cohort study. Int Breastfeed J. 2020;15(1):79.
Forster DA, McLachlan HL, Lumley J. Factors associated with breastfeeding at six months postpartum in a group of Australian women. Int Breastfeed J. 2006;1(1):18.
Ahmed AH, Sands LP. Effect of pre- and postdischarge interventions on breastfeeding outcomes and weight gain among premature infants. J Obstet Gynecol Neonatal Nurs. 2010;39(1):53-63.
Ahlqvist-Bjorkroth S, Vaarno J, Junttila N, Pajulo M, Raiha H, Niinikoski H, et al. Initiation and exclusivity of breastfeeding: association with mothers' and fathers' prenatal and postnatal depression and marital distress. Acta Obstet Gynecol Scand. 2016;95(4):396-404.
Alianmoghaddam N, Phibbs S, Benn C. Reasons for stopping exclusive breastfeeding between three and six months: a qualitative study. J Pediatr Nurs. 2018;39:37-43.
Lauer EA, Armenti K, Henning M, Sirois L. Identifying barriers and supports to breastfeeding in the workplace experienced by mothers in the New Hampshire special supplemental nutrition program for women, infants, and children utilizing the total worker health framework. Int J Environ Res Public Health. 2019;16(4).
Balkam JA, Cadwell K, Fein SB. Effect of components of a workplace lactation program on breastfeeding duration among employees of a public-sector employer. Matern Child Health J. 2011;15(5):677-83.
Acuna-Muga J, Ureta-Velasco N, de la Cruz-Bertolo J, Ballesteros-Lopez R, Sanchez-Martinez R, Miranda-Casabona E, et al. Volume of milk obtained in relation to location and circumstances of expression in mothers of very low birth weight infants. J Hum Lact. 2014;30(1):41-6.
Spatz DL. Ten steps for promoting and protecting breastfeeding for vulnerable infants. J Perinat Neonatal Nurs. 2004;18(4):385-96.
Scott JA, Landers MC, Hughes RM, Binns CW. Factors associated with breastfeeding at discharge and duration of breastfeeding. J Paediatr Child Health. 2001;37(3):254-61.
Wong C, Schreiber V, Crawford K, Kumar S. Male infants are at higher risk of neonatal mortality and severe morbidity. Aust N Z J Obstet Gynaecol. 2023;63:550-5.
Fu M, Song W, Yu G, Yu Y, Yang Q. Risk factors for length of NICU stay of newborns: A systematic review. Front Pediatr. 2023;11:1121406.
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














