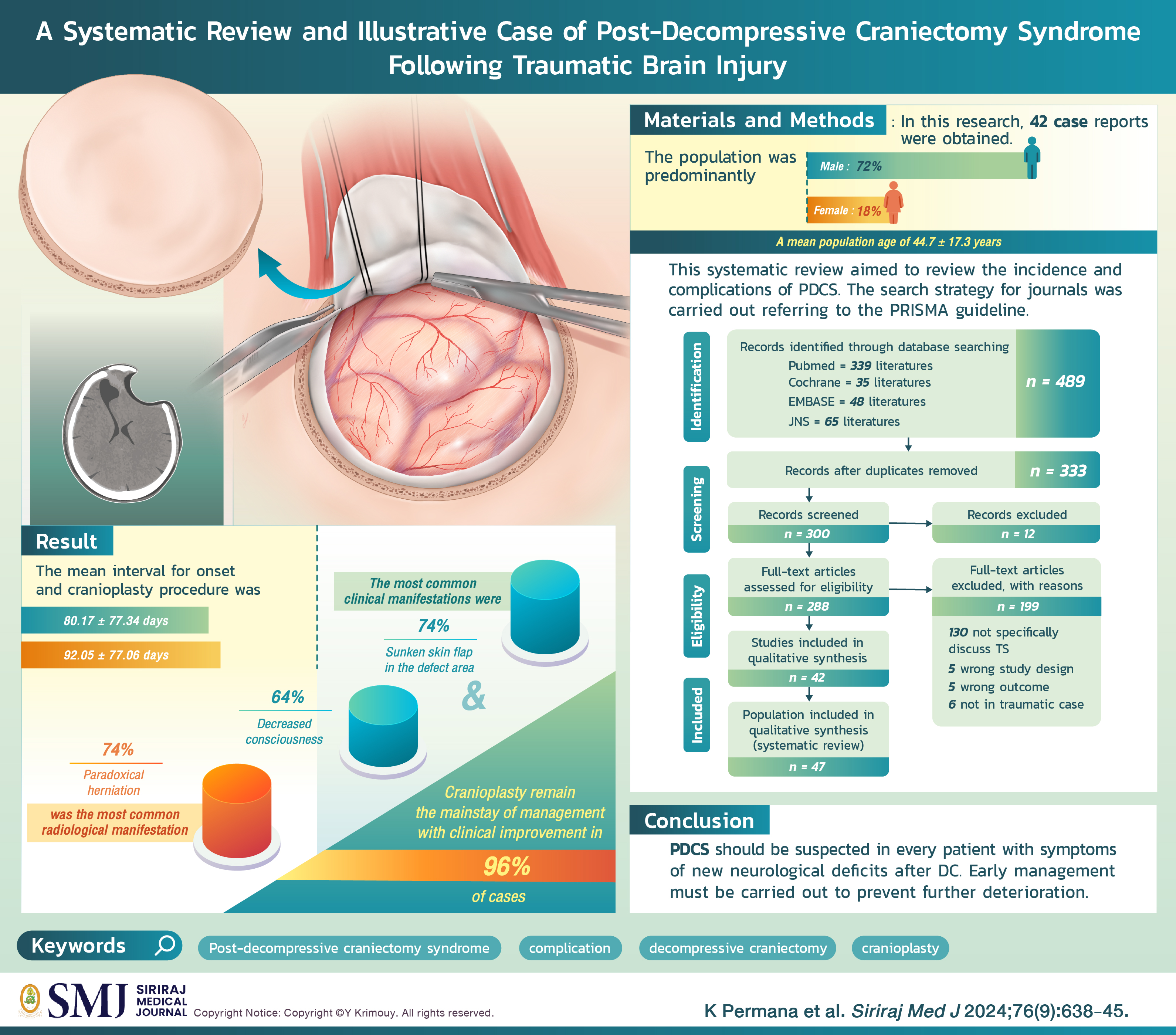
A Systematic Review and Illustrative Case of Post- Decompressive Craniectomy Syndrome Following Traumatic Brain Injury
DOI:
https://doi.org/10.33192/smj.v76i9.269127Keywords:
Post-decompressive craniectomy syndrome, complication, decompressive craniectomy, cranioplastyAbstract
Post-decompressive craniectomy syndrome (PDCS) is a complication following decompressive craniectomy (DC). PDCS or also known as trephine or sunken skin flap syndrome has an indirect relationship with traumatic brain injury (TBI). The mechanism of PDCS is not yet fully understood and the clinical manifestations are diverse, causing PDCS to often be underdiagnosed. In this study, the authors aim to create a systematic review of PDCS following TBI including a discussion of incidence, clinical and radiological manifestations, management and outcome. This systematic review is conducted based on the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guideline. The literature search included electronic databases PubMed, Cochrane, JNS and EMBASE. All studies included were available in English and full-text format. In this research, 42 case reports were obtained. The population was predominantly male (72%) with a mean population age of 44.7 ± 17.3 years. The mean interval for onset and cranioplasty procedure was 80.17 ± 77.34 days and 92.05 ± 77.06, respectively. The most common clinical manifestations were sunken skin flap in the defect area (74%) and decreased consciousness (64%). Paradoxical herniation (74%) was the most common radiological manifestation. There was no connection between the occurrence of PDCS and the size of the defect. Cranioplasty remains the mainstay of management with clinical improvement in 96% of cases. PDCS should be suspected in every patient with symptoms of new neurological deficits after DC. Early management must be carried out to prevent further deterioration.
References
Joseph V, Reilly P. Syndrome of the trephined. J Neurosurg. 2009;111(4):650-2.
Annan M, De Toffol B, Hommet C, Mondon K. Sinking skin flap syndrome (or Syndrome of the trephined): A review. Br J Neurosurg. 2015;4;29(3):314-8.
Grant FC, Norcross NC. Repair of Cranial Defects by Cranioplasty. Ann Surg. 1939;110(4):488-512.
Di Rienzo A, Colasanti R, Gladi M, Pompucci A, Della Costanza M, Paracino R, et al. Sinking flap syndrome revisited: the who, when and why. Neurosurg Rev. 2020;1;43(1):323-35.
Yang XF, Wen L, Shen F, Li G, Lou R, Liu WG, et al. Surgical complications secondary to decompressive craniectomy in patients with a head injury: a series of 108 consecutive cases. Acta Neurochir (Wien). 2008;13;150(12):1241-8.
Sveikata L, Vasung L, El Rahal A, Bartoli A, Bretzner M, Schaller K, et al. Syndrome of the trephined: clinical spectrum, risk factors, and impact of cranioplasty on neurologic recovery in a prospective cohort. Neurosurg Rev. 2021;7;45(2):1431-43.
Fodstad H, Love JA, Ekstedt J, Friden H, Liliequist B. Effect of cranioplasty on cerebrospinal fluid hydrodynamics in patients with the syndrome of the trephined. Acta Neurochir (Wien). 1984;70(1-2):21-30.
Romero FR, Zanini MA, Ducati LG, Gabarra RC. Sinking Skin Flap Syndrome with Delayed Dysautonomic Syndrome—An atypical presentation. Int J Surg Case Rep. 2013;4(11):1007-9.
Vasung L, Hamard M, Soto MCA, Sommaruga S, Sveikata L, Leemann B, et al. Radiological signs of the syndrome of the trephined. Neuroradiology. 2016;58(6):557-68.
Ghajar J. Traumatic brain injury. Lancet. 2000;356(9233):923-9.
Noble KA. Traumatic Brain Injury and Increased Intracranial Pressure. J Perianesth Nurs. 2010;25(4):242-8.
Jha RM, Kochanek PM, Simard JM. Pathophysiology and treatment of cerebral edema in traumatic brain injury. Neuropharmacology. 2019;145:230-46.
Jha RM, Kochanek PM. A Precision Medicine Approach to Cerebral Edema and Intracranial Hypertension after Severe Traumatic Brain Injury: Quo Vadis? Curr Neurol Neurosci Rep. 2018;18(12):105.
Rossini Z, Nicolosi F, Kolias AG, Hutchinson PJ, De Sanctis P, Servadei F. The History of Decompressive Craniectomy in Traumatic Brain Injury. Front Neurol. 2019;10:458.
Wilson MH. Monro-Kellie 2.0: The dynamic vascular and venous pathophysiological components of intracranial pressure. J Cereb Blood Flow Metab. 2016;36(8):1338-50.
Moon JW, Hyun DK. Decompressive Craniectomy in Traumatic Brain Injury: A Review Article. Korean J Neurotrauma. 2017;13(1):1-8.
Gopalakrishnan MS, Shanbhag NC, Shukla DP, Konar SK, Bhat DI, Devi BI. Complications of Decompressive Craniectomy. Front Neurol. 2018;9:977.
Borha A, Chagnot A, Goulay R, Emery E, Vivien D, Gaberel T. Cranioplasty Reverses Dysfunction of the Solutes Distribution in the Brain Parenchyma After Decompressive Craniectomy. Neurosurgery. 2020;87(5):1064-9.
Cassagne M, Claes AS. Sinking Skin Flap Syndrome, a Rare Complication of Craniectomy. J Belg Soc Radiol. 2022;106(1):52.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Santander X, Hidalgo YG, Flores JC, Gómez-Jordana B. Sinking skin syndrome in a decompressive craniectomy series: Clinical and radiological features. Surg Neurol Int. 2022;13:422.
Sedney CL, Dillen W, Julien T. Clinical spectrum and radiographic features of the syndrome of the trephined. J Neurosci Rural Pract. 2015;6(03):438-41.
Sveikata L, Vasung L, El Rahal A, Bartoli A, Bretzner M, Schaller K, et al. Syndrome of the trephined: clinical spectrum, risk factors, and impact of cranioplasty on neurologic recovery in a prospective cohort. Neurosurg Rev. 2021;45(2):1431-43.
Vasung L, Hamard M, Soto MCA, Sommaruga S, Sveikata L, Leemann B, et al. Radiological signs of the syndrome of the trephined. Neuroradiology. 2016;58(6):557-68.
Stiver SI, Wintermark M, Manley GT. Reversible monoparesis following decompressive hemicraniectomy for traumatic brain injury. J Neurosurg. 2008;109(2):245-54.
Chugh A, Punia P, Gotecha S. Sinking Skin Flap Syndrome following Posttraumatic Hydrocephalus. Case Rep Neurol Med. 2021;2021:1-8.
Zhao J, Li G, Zhang Y, Zhu X, Hou K. Sinking skin flap syndrome and paradoxical herniation secondary to lumbar drainage. Clin Neurol Neurosurg. 2015;133:6-10.
Samson G, Kumar S, Chacko AG, Rajshekhar V. Unusual presentation of the ‘syndrome of the trephined’. Neurol India. 2004;52(4):504-5.
Arai N, Abe H, Nishitani H, Kanemaru S, Yasunaga M, Yamamoto S, et al. Characteristics of Patients with Trephine Syndrome: A Retrospective Study. Prog Rehabil Med. 2022;7:20220008.
Dillen WL, Pittman TA, Grupke SL. Novel Temporary Treatment for a Severe Case of Syndrome of Trephined. World Neurosurg. 2018;120:200-4.
Joseph V, Reilly P. Syndrome of the trephined: Case report. J Neurosurg. 2009;111(4):650-2.
Jeyaraj P. Importance of Early Cranioplasty in Reversing the “Syndrome of the Trephine/Motor Trephine Syndrome/Sinking Skin Flap Syndrome”. J Maxillofac Oral Surg. 2015;14(3):666-73.
O’Connell MT, Seal A, Nortje J, Al-Rawi PG, Coles JP, Fryer TD, et al. Glucose metabolism in traumatic brain injury: a combined microdialysis and [18F]-2-fluoro-2-deoxy-D-glucose — positron emission tomography (FDG-PET) study. Acta Neurochir Suppl. 2005;95;165-8.
Tarr JT, Hagan M, Zhang B, Tanna N, Andrews BT, Lee JC, et al. Syndrome of the Trephined: Quantitative Functional Improvement after Large Cranial Vault Reconstruction. Plast Reconstr Surg. 2020;145(6):1486-94.
Lilja-Cyron A, Andresen M, Kelsen J, Andreasen TH, Fugleholm K, Juhler M. Long-Term Effect of Decompressive Craniectomy on Intracranial Pressure and Possible Implications for Intracranial Fluid Movements. Neurosurgery. 2020;86(2):231-40.
Corallo F, De Cola MC, Lo Buono V, Marra A, De Luca R, Trinchera A, et al. Early vs late cranioplasty: what is better? Int J Neurosci. 2017;127(8):688-93.
Lilja-Cyron A, Andresen M, Kelsen J, Andreasen TH, Petersen LG, Fugleholm K, et al. Intracranial pressure before and after cranioplasty: insights into intracranial physiology. J Neurosurg. 2020;133(5):1548-58.
Kurland DB, Khaladj-Ghom A, Stokum JA, Carusillo B, Karimy JK, Gerzanich V, et al. Complications Associated with Decompressive Craniectomy: A Systematic Review. Neurocrit Care. 2015;23(2):292-304.
Santos De Araujo Junior A, Arlant PA, Salvestrini A, Altieri CE, Santos JG, Figueira Pinto L, et al. Asymmetric optic nerve sheath diameter as an outcome fator following cranioplasty in ‘syndrome of the trephined’. Arq Neuropsiquiatr. 2013;71(12):963-6.
Park HY, Kim S, Kim JS, Lim SH, Kim Y Il, Lee DH, et al. Sinking skin flap syndrome or syndrome of the trephined: A report of two cases. Ann Rehabil Med. 2019;43(1):111-4.
Safi S, Ali A, Abdelhafez I, Salam A, Alrabayah T, Alyafei A, et al. Predictors of Clinical Outcomes in Autologous Cranioplasty. World Neurosurg. 2022;167:e561-6.
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














