Health Survey of Monks Residing in Urban Areas: The Bangkok Noi Model
DOI:
https://doi.org/10.33192/smj.v76i11.269296Keywords:
Buddhist monks, Health survey, Noncommunicable diseases, Thailand, UrbanAbstract
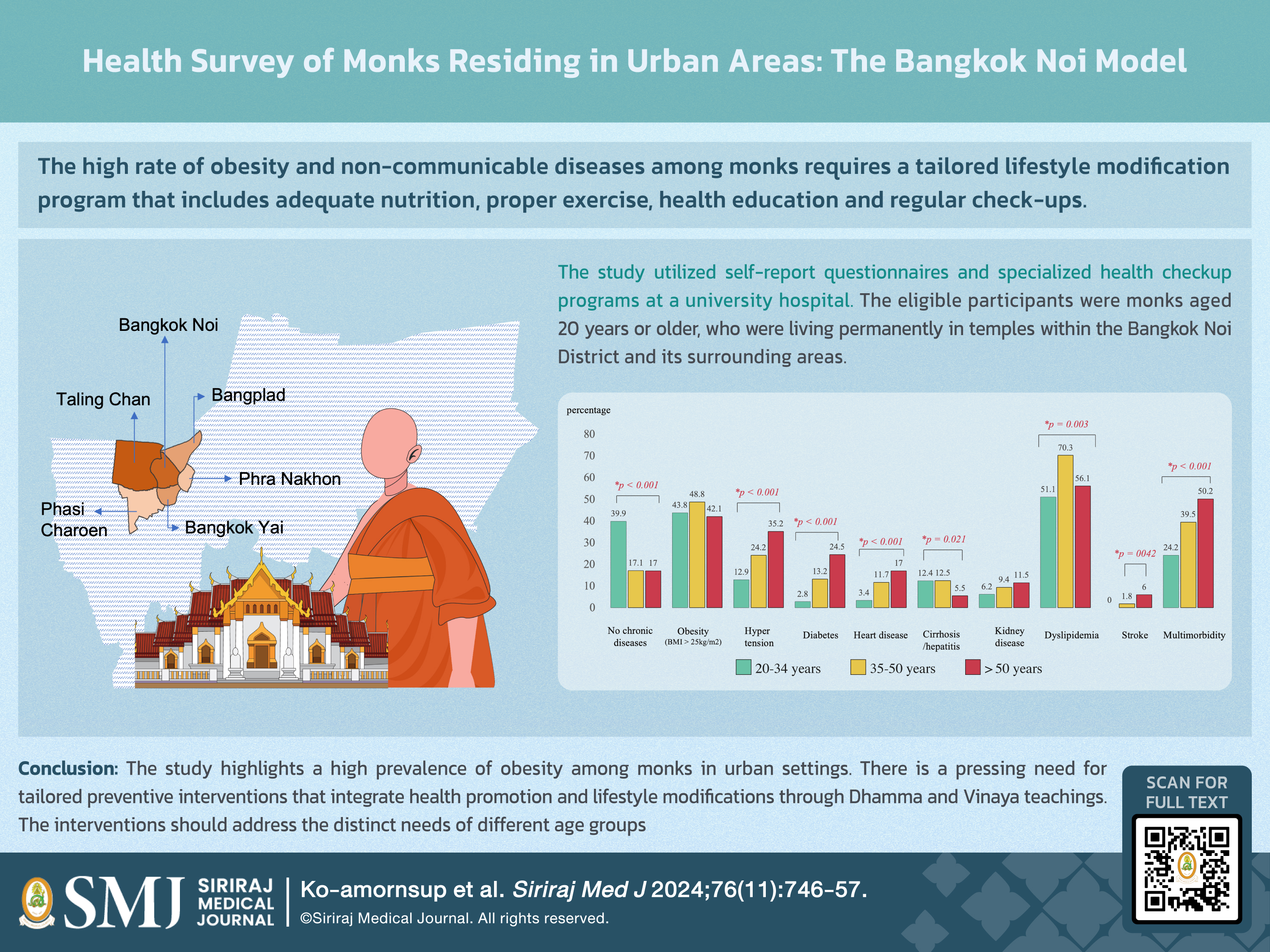
Objective: This study aimed to assess the prevalence of obesity and identify associated health problems and behaviors among monks residing in Bangkok Noi and its adjacent districts.
Materials and Methods: Employing a cross-sectional design, this research incorporated self-report questionnaires and specialized health checkup programs at a university hospital. Eligible participants were monks aged 20 years or older, living permanently in temples within the Bangkok Noi District and its adjacent districts. Monks in shortterm ordination were excluded. Data collection occurred between February 2022 and July 2023.
Results: Out of 560 monks who participated by completing both the questionnaires and health examinations, the average age was 46.49±16.97 years. Most participants resided in the Taling Chan (35.4%) and Bangkok Noi (31.8%) districts. Significant health issues included non-communicable diseases, with dyslipidemia affecting 57.8% and obesity 44.2% of the cohort. Monks over the age of 50 exhibited a remarkably higher rate of multimorbidity (50.2%) than their younger counterparts (24.2%, p < 0.001, 95% CI 20.71–27.97). Dietary habits revealed that younger monks were more prone to consuming fried, sweet and instant foods (74.5%, p < 0.001, 95% CI 70.67–78.07). Moreover, a significant proportion of younger monks demonstrated proficient e-health literacy (74.2%, p < 0.001, 95% CI 70.37–77.78).
Conclusion: The study highlights a high prevalence of obesity among monks in urban settings. There is a pressing need for tailored preventive interventions that integrate health promotion and lifestyle modifications through Dhamma and Vinaya teachings. The interventions should address the distinct needs of different age groups.
References
Hackett C, Grim B, Stonawski M, Skirbekk V, Potančoková M, Abel G. The Global Religious Landscape: A Report on the Size and Distribution of the World's Major Religious Groups as of 20102012.
Arunsutalangkarn P. role of thai buddhist monks and education in thai society. Journal of Buddhist Anthropology. 2023;8(2):96-103.
Attaworakun S, Ngamdee N, Cherdsuntia V. Monk’s health in urban area: The Problem that should be considered. Vajira Medical Journal: Journal of Urban Medicine. 2019;63(Supplement):S177-S84.
WHO. Urban health ; 2021[cite 2024 June 20] [Available from: https://www.who.int/health-topics/urban-health.
World Health Organization. Noncommunicable diseases country profiles 2018. Geneva; 2018. Licence: CC BY-NC-SA 3.0 IGO.
World Health Organization (WHO) SEA, Thailand. Prevention and Control of Noncommunicable Diseases in Thailand – The Case for Investment. 2021.
Phra Maha Wichian Wachiramotamonuen KA, Kanchanaphet, Phra Khru Sutthakit Somso. The role of monks in modern Thai society development. Journal Maha Chula tani Mahachulalongkornrajavidyalaya University. 2021;3(6):42–9.
Puckcharern; WALM-sNRWSH. Thai National Health Examination Survey, NHES V. Health Systems Research Institute (HSRI). 2016.
Jeamjitvibool T, Tankumpuan T, Lukkahatai N, Davidson PM. Noncommunicable diseases and social determinants of health in Buddhist monks: An integrative review. Res Nurs Health. 2022;45(2):249-60.
Angkatavanich J, Ariyapitipun, T., Wisesrith, W., Prasobtham, J., &Punpanich, D. . Situation of Nutritional Problem in Buddhist Monks from Project “Sonkthaiglairok”. Bangkok: Thai Health Promotion Foundation (in Thai). 2016.
Srimantayamas V, Fongkaew W, Suksatit B, Aree P, Kosachunhanun N. Health Behaviors and Health-Related Quality of Life among Buddhist Monks with Metabolic Syndrome. Pacific Rim Int J Nurs Res. 2020;24(2):159-71.
Phrakru Phiphit Sutatorn, PC, WB, TP, PL, NY, et al. National Monks Health Statute. 3rd Floor, National Health Building, 88/39 Tiwanon Road 14, Village No. 4, Talat Khwan Subdistrict, Mueang District, Nonthaburi Province 11000: National Health Commission Office (NHCO); 2017.
University FoMSHM. Bangkok Noi Model 2020 [Available from: https://www2.si.mahidol.ac.th/en/sustainable/good-health-and-well-being/bangkok-noi-model/.
Gozzoli P, Rongrat T, Gozzoli R. Design Thinking and Urban Community Development: East Bangkok. Sustainability. 2022;14:4117.
Group IT, Department OotS, Buddhism NOo. Basic Information on Buddhism for the Year 20212021.
Suchar C. The Relationship between Food Consumption Behavior, and Blood Sugar, Lipid Levels, AND Body Mass Index Among Monks in Samutprakarn Province. HCU Journal. 2018;21(42):107-21.
Skou ST, Mair FS, Fortin M, Guthrie B, Nunes BP, Miranda JJ, et al. Multimorbidity. Nat Rev Dis Primers. 2022;8(1):48.
World Health Organization. Multimorbidity: Technical Series on Safer Primary Care. Geneva; 2016. Licence: CC BY-NC-SA 3.0 IGO.
CDC. Physical Activity ; 2022 [cite 2024 June 20]. Available from: https://www.cdc.gov/physicalactivity/basics/adults/index.htm.
Health Promotion Division FoMSHMU. Basal Metabolic Rate (BMR) 2021. Available from: https://www.si.mahidol.ac.th/th/healthdetail.asp?aid=1472.
Wellmon R. Chapter 32 - Gait Assessment and Training. In: Cameron MH, Monroe LG, editors. Physical Rehabilitation. Saint Louis: W.B. Saunders; 2007. p. 844-76.
de Fátima Ribeiro Silva C, Ohara DG, Matos AP, Pinto A, Pegorari MS. Short Physical Performance Battery as a Measure of Physical Performance and Mortality Predictor in Older Adults: A Comprehensive Literature Review. Int J Environ Res Public Health. 2021;18(20):10612.
Laochai W TD, Jiraprapapong N. Promoting Physical Activity among Buddhist Monks: The Role of Nurse. J Food Health Bioenv Sci. 2023;13(2):59-66.
Angthawanich J SA. Thai remote distant media of disease: integrated nutrituon to the Buddhist way 4 sectors. Bangkok: Chor Langa. 2015.
hospital P. Health examination program for novice monks 2017. Nonthaburi: Department of Medical Services, Ministry of Public Health2017
Bureau H. Screning of the health of monks in Bangkok in 2013: Bangkok: Health Bureau; 2014.
Palmer AK JM. Metabolic changes in aging humans: current evidence and therapeutic strategies. J Clin Invest. 2022;27(5):29-35.
Shimokata H, Kuzuya F. [Aging, basal metabolic rate, and nutrition]. Nihon Ronen Igakkai Zasshi. 1993;30(7):572-6.
Pilgrim AL RS, Sayer AA, Roberts HC. An overview of appetite decline in older people. Nurs Older People. 2015;27(5):29-35.
Wang X LW. Research progress on digital health literacy of older adults: A scoping review. Front Public Health. 2022;10:906089.
De Santis KK JT, Sina E, Wienert J, Zeeb H. Digitization and Health in Germany: Cross-sectional Nationwide Survey. JMIR Public Health Surveill 2021;7(11):e32951.
Papp-Zipernovszky O HM, Schulz PJ, Csabai M. Generation Gaps in Digital Health Literacy and Their Impact on Health Information Seeking Behavior and Health Empowerment in Hungary. Front Public Health. 2021;9:635943.
Lin CY GM, Griffiths MD, Bravell ME, Broström A, Pakpour AH. Mediated effects of insomnia, psychological distress and medication adherence in the association of eHealth literacy and cardiac events among Iranian older patients with heart failure: a longitudinal study. Eur J Cardiovasc Nurs. 2020;19(2):155-64.
Rees J TR, Burton A, Walters K, Cooper C. Supporting self-care of long-term conditions in people with dementia: A systematic review. Int J Nurs Stud. 2021;116:103432.
Clark JE. Diet, exercise or diet with exercise: comparing the effectiveness of treatment options for weight-loss and changes in fitness for adults (18-65 years old) who are overfat, or obese; systematic review and meta-analysis. J Diabetes Metab Disord 2015;14:31.
Strasser B FD. Diet Versus Exercise in Weight Loss and Maintenance: Focus on Tryptophan. Int J Tryptophan Res. 2016;9:9-16.
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














