Prehabilitation in Clinical Practice: A Review of Concepts and Implementation in Enhancing Postoperative Outcomes
DOI:
https://doi.org/10.33192/smj.v76i9.269392Keywords:
Prehabilitation, Perioperative, Postoperative outcomes, Enhanced Recovery After Surgery, Multidisciplinary, MultimodalAbstract
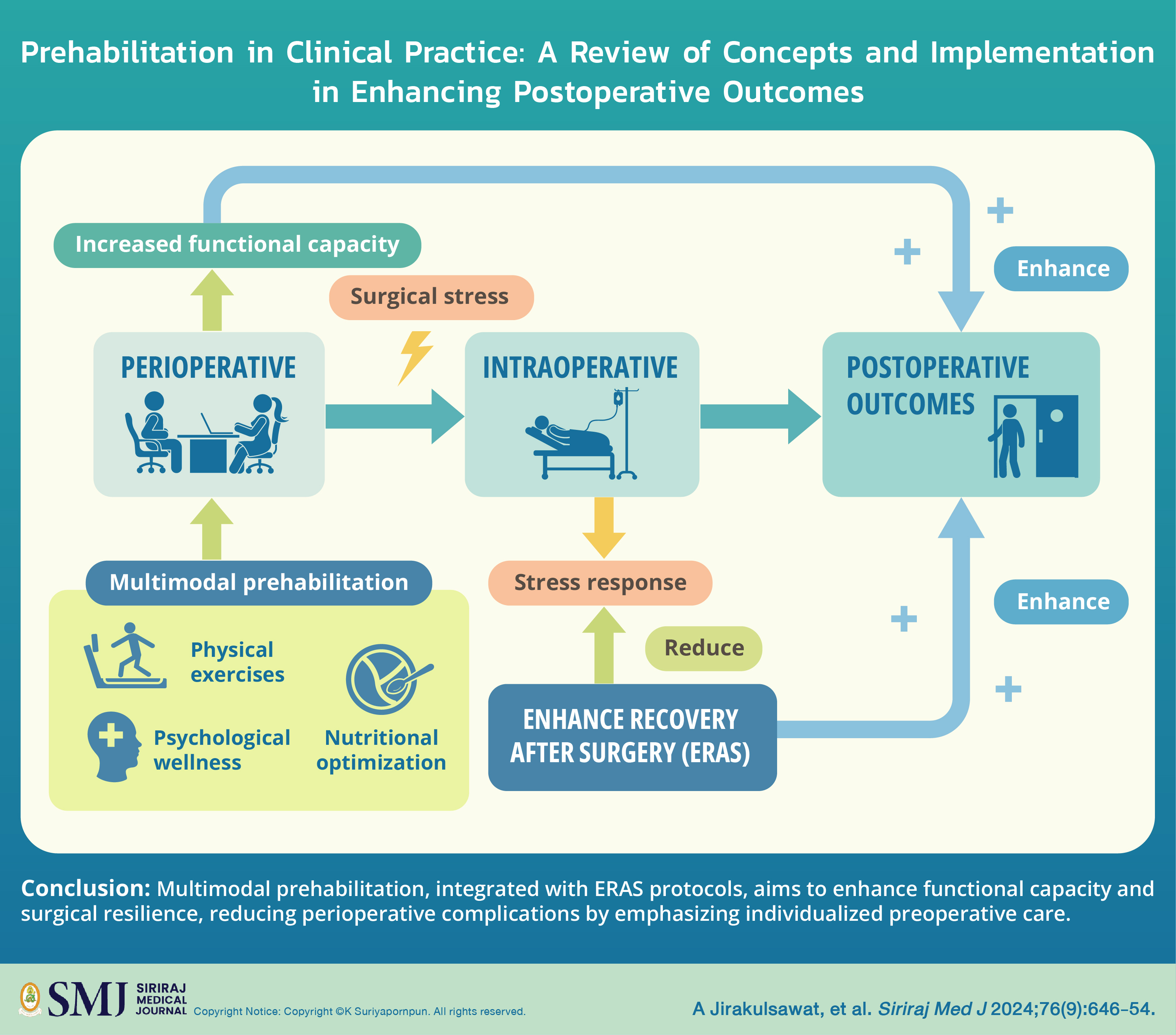
In the presence of globalization and advancing clinical knowledge, there is a paradigm shift from a single patient care sector to a multidisciplinary-collaborated health care team. In pursuit of favorable postoperative outcomes, reduced length of hospital stay, minimized complications and morbidity, and accelerated recovery, prehabilitation strategies assume a prominent role following preoperative assessment. Fundamental to prehabilitation are physical activity, nutrition, and psychological interventions, aimed at enhancing preoperative functional reserve through expert-designed program sessions spanning various specialties. Enhanced Recovery After Surgery (ERAS) serves as an intra- and postoperative strategy to facilitate the smooth return of patients to their baseline status postoperation by mitigating surgical stress. Integrating prehabilitation into ERAS protocols holds promise for optimizing
postoperative outcomes. Protocols for prehabilitation across diverse patient groups have been proposed, paving the way for the routine incorporation of prehabilitation into patient care.
References
World Health Organization. Ageing and health. WHO. 2022. [cited 2024 May 4]. Available from: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health
United Nations. World Social Report 2023: Leaving no one behind in an ageing world. Department of Economic and Social Affairs. 2023. [cited 2024 May 4]. Available from: https://www.un.org/development/desa/dspd/wp-content/uploads/sites/22/2023/01/WSR_2023_Chapter_Key_Messages.pdf
Ljungqvist O, Scott M, Fearon KC. Enhanced Recovery After Surgery: A Review. JAMA Surg. 2017;152(3):292-8.
Carli F. Prehabilitation for the Anesthesiologist. Anesthesiology. 2020; 133(3):645-52.
Molenaar CJL, Papen-Botterhuis NE, Herrle F, Slooter GD. Prehabilitation, making patients fit for surgery - a new frontier in perioperative care. Innov Surg Sci. 2019; 4(4):132-8.
Arena R, Myers J, Williams MA, Gulati M, Kligfield P, Balady GJ, et al.American Heart Association Committee on Exercise, Rehabilitation, and Prevention of the Council on Clinical Cardiology; American Heart Association Council on Cardiovascular Nursing. Assessment of functional capacity in clinical and research settings: a scientific statement from the American Heart Association Committee on Exercise, Rehabilitation, and Prevention of the Council on Clinical Cardiology and the Council on Cardiovascular Nursing. Circulation. 2007;116(3):329-43.
Snowden CP, Prentis JM, Anderson HL, Roberts DR, Randles D, Renton M, et al. Submaximal cardiopulmonary exercise testing predicts complications and hospital length of stay in patients undergoing major elective surgery. Ann Surg. 2010;251(3):535-41.
Carli F, Awasthi R, Gillis C, Baldini G, Bessissow A, Liberman AS, et al. Integrating prehabilitation in the preoperative clinic: a paradigm shift in perioperative care. Anesth Analg. 2021;132:1494-500.
Topp R, Ditmyer M, King K, Doherty K, Hornyak J 3rd. The effect of bed rest and potential of prehabilitation on patients in the intensive care unit. AACN Clin Issues. 2002;13(2):263-76.
Carli F, Zavorsky GS. Optimizing functional exercise capacity in the elderly surgical population. Curr Opin Clin Nutr Metab Care. 2005;8(1):23-32.
Gonçalves CG, Groth AK. Prehabilitation: how to prepare our patients for elective major abdominal surgeries? Rev Col Bras Cir. 2019;46(5):e20192267.
Kothmann E, Batterham AM, Owen SJ, Turley AJ, Cheesman M, Parry A, et al. Effect of short-term exercise training on aerobic fitness in patients with abdominal aortic aneurysms: a pilot study. Br J Anaesth. 2009;103(4):505-10.
Le Roy B, Selvy M, Slim K. The concept of prehabilitation: What the surgeon needs to know? J Visc Surg. 2016;153(2):109-12.
Ferguson M, Shulman M. Cardiopulmonary Exercise Testing and Other Tests of Functional Capacity. Curr Anesthesiol Rep. 2022;12(1):26-33.
Glaab T, Taube C. Practical guide to cardiopulmonary exercise testing in adults. Respir Res. 2022;23(1):9.
Myers J, Oliveira R, Dewey F, Arena R, Guazzi M, Chase P, et al. Validation of a cardiopulmonary exercise test score in heart failure. Circ Heart Fail. 2013;6(2):211-8.
Otto JM, Levett DZH, Grocott MPW. Cardiopulmonary Exercise Testing for Preoperative Evaluation: What Does the Future Hold? Curr Anesthesiol Rep. 2020;10:1-11.
Moran J, Wilson F, Guinan E, McCormick P, Hussey J, Moriarty J. Role of cardiopulmonary exercise testing as a risk-assessment method in patients undergoing intra-abdominal surgery: a systematic review. Br J Anaesth. 2016;116(2):177-91.
Hlatky MA, Boineau RE, Higginbotham MB, Lee KL, Mark DB, Califf RM, et al. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index). Am J Cardiol. 1989;64(10):651-4.
Wijeysundera DN, Beattie WS, Hillis GS, Abbott TEF, Shulman MA, Ackland GL, et al. Integration of the Duke Activity Status Index into preoperative risk evaluation: a multicentre prospective cohort study. Br J Anaesth. 2020;124(3):261-70.
Dias C, Torriani-Pasin C, Galvão ACJ, Costa PHV, Polese JC. Validation of the Duke Activity Status Index questionnaire by telephone in individuals after stroke. Int J Cardiol Cardiovasc Risk Prev. 2023;19:200208.
Sinclair RC, Batterham AM, Davies S, Cawthorn L, Danjoux GR. Validity of the 6 min walk test in prediction of the anaerobic threshold before major non-cardiac surgery. Br J Anaesth. 2012;108(1):30-5.
Shulman MA, Cuthbertson BH, Wijeysundera DN, Pearse RM, Thompson B, Torres E, et al. Using the 6-minute walk test to predict disability-free survival after major surgery. Br J Anaesth. 2019;122(1):111-9.
Giannitsi S, Bougiakli M, Bechlioulis A, Kotsia A, Michalis LK, Naka KK. 6-minute walking test: a useful tool in the management of heart failure patients. Ther Adv Cardiovasc Dis. 2019;13:1753944719870084.
Struthers R, Erasmus P, Holmes K, Warman P, Collingwood A, Sneyd JR. Assessing fitness for surgery: a comparison of questionnaire, incremental shuttle walk, and cardiopulmonary exercise testing in general surgical patients. Br J Anaesth. 2008;101(6):774-80.
Singh SJ, Morgan MD, Hardman AE, Rowe C, Bardsley PA. Comparison of oxygen uptake during a conventional treadmill test and the shuttle walking test in chronic airflow limitation. Eur Respir J. 1994;7(11):2016-20.
Rodseth RN, Biccard BM, Le Manach Y, Sessler DI, Lurati Buse GA, Thabane L, et al. The prognostic value of pre-operative and post-operative B-type natriuretic peptides in patients undergoing noncardiac surgery: B-type natriuretic peptide and N-terminal fragment of pro-B-type natriuretic peptide: a systematic review and individual patient data meta-analysis. J Am Coll Cardiol. 2014;63(2):170-80.
Schmidt G, Frieling N, Schneck E, Habicher M, Koch C, Rubarth K, et al. Preoperative routine measurement of NT-proBNP predicts postoperative morbidity after non-cardiac surgery with intermediate or high surgical risk: an observational study. BMC Anesthesiol. 2024;24(1):113.
Devereaux PJ, Ofori S. Utility of pre-operative cardiac biomarkers to predict myocardial infarction and injury after non-cardiac surgery. Eur Heart J Acute Cardiovasc Care. 2023;12(11):740-2.
Meister R, Puelacher C, Glarner N, Gualandro DM, Andersson HA, Pargger M, et al. Prediction of perioperative myocardial infarction/injury in high-risk patients after noncardiac surgery. Eur Heart J Acute Cardiovasc Care. 2023;12(11):729-39.
Duceppe E, Borges FK, Conen D, Tiboni M, Chan MTV, Patel A, et al. Association of Preoperative Growth Differentiation Factor-15 Concentrations and Postoperative Cardiovascular Events after Major Noncardiac Surgery. Anesthesiology. 2023;138(5):508-22.
West MA, Wischmeyer PE, Grocott MPW. Prehabilitation and Nutritional Support to Improve Perioperative Outcomes. Curr Anesthesiol Rep. 2017;7(4):340-9.
Weimann A, Braga M, Carli F, Higashiguchi T, Hübner M, Klek S, et al. ESPEN guideline: Clinical nutrition in surgery. Clin Nutr. 2017;36(3):623-50.
Weimann A, Braga M, Harsanyi L, Laviano A, Ljungqvist O, Soeters P, et al. ESPEN Guidelines on Enteral Nutrition: Surgery including organ transplantation. Clin Nutr. 2006;25(2):224-44.
Campbell WW, Leidy HJ. Dietary protein and resistance training effects on muscle and body composition in older persons. J Am Coll Nutr. 2007;26(6):696S-703S.
Burke LM, Hawley JA, Ross ML, Moore DR, Phillips SM, Slater GR, et al. Pre-exercise aminoacidemia and muscle protein synthesis after resistance exercise. Med Sci Sports Exerc. 2012;44(10):1968-77.
Tsimopoulou I, Pasquali S, Howard R, Desai A, Gourevitch D, Tolosa I, et al. Psychological prehabilitation before cancer surgery: a systematic review. Ann Surg Oncol. 2015;22(13):4117-23.
Shuldham C. A review of the impact of pre-operative education on recovery from surgery. Int J Nurs Stud. 1999;36(2):171-7.
Van Kuiken ME, Zhao S, Covinsky K, Boscardin J, Finlayson E, Suskind AM. Frailty Is Associated with an Increased Risk of Complications and Need for Repeat Procedures after Sling Surgery in Older Adults. J Urol. 2022;207(6):1276-84.
Baimas-George M, Watson M, Elhage S, Parala-Metz A, Vrochides D, Davis BR. Prehabilitation in Frail Surgical Patients: A Systematic Review. World J Surg. 2020;44(11):3668-78.
Wong HMK, Qi D, Ma BHM, Hou PY, Kwong CKW, Lee A, et al. Multidisciplinary prehabilitation to improve frailty and functional capacity in high-risk elective surgical patients: a retrospective pilot study. Perioper Med (Lond). 2024;13(1):6.
Meneses-Echavez JF, Loaiza-Betancur AF, Díaz-López V, Echavarría-Rodríguez AM, Triana-Reina HR. Prehabilitation programs for individuals with cancer: a systematic review of randomized-controlled trials. Syst Rev. 2023;12(1):219.
Carlisle JB. Pre-operative co-morbidity and postoperative survival in the elderly: beyond one lunar orbit. Anaesthesia. 2014;69 Suppl 1:17-25.
Malot C, Durand-Bouteau A, Barizien N, Bizard A, Kennel T, Fischler M, et al. Prehabilitation Program in Elderly Patients: A Prospective Cohort Study of Patients Followed Up Postoperatively for Up to 6 Months. J Clin Med. 2021;10(19):4500.
Heng G, Lohsiriwat V, Tan K-Y. Suitability of Enhanced Recovery after Surgery (ERAS) Protocols for Elderly Colorectal Cancer Patients. Siriraj Med J. 2019;72(1):18-23.
Suenghataiphorn T, Songwisit S, Tornsatitkul S, Somnuke P. An Overview on Postoperative Cognitive Dysfunction; Pathophysiology, Risk Factors, Prevention and Treatment. Siriraj Med J. 2022;74(10):705-13.
Tawantanakorn T, Phibalyart W, Parakonthun T, Nampoolsuksan C, Suwatthanarak T, Srisuworanan N, et al. Changes in Physical Components after Gastrectomy for Adenocarcinoma of Stomach and Esophagogastric Junction. Siriraj Med J. 2023;75(4):241-9.
Nampoolsuksan C, Parakonthun T, Tawantanakorn T, Mora A, Swangsri J, Akaraviputh T, et al. Short-term Postoperative Outcomes Before and After the Establishment of the Siriraj Upper Gastrointestinal Cancer Center: A Propensity Score Matched Analysis. Siriraj Med J. 2020;72(4):215-320.
Jiamton S, Jantanapornchai N, Nokdhes Y-N, Patthamalai P, Tantrapornpong P, Nanchaipruek Y, et al. Lidocaine Reducing Pain from Benzathine Penicillin Injection: A Controlled Trial. Siriraj Med J. 2022;74(10):699-704.
Lohsiriwat V, Jaturanon P. Effect of Intraoperative Hypothermia on Surgical Outcomes after Colorectal Surgery within an Enhanced Recovery after Surgery Pathway. Siriraj Med J. 2019;71(1):52-8.
Banyong C, Chanruangvanich W, Thosingha O, Lohsiriwat V. Factors Predicting Prolonged Postoperative Ileus in Patients Undergoing Major Gastrointestinal Surgery. Siriraj Med J. 2022;74(9):537-4.
Lohsiriwat V. Mosapride Reduces Prolonged Postoperative Ileus after Open Colorectal Surgery in the Setting of Enhanced Recovery after Surgery (ERAS): A Matched Case-Control Study. Siriraj Med J. 2019;71(3):181-8.
Gillis C, Fenton TR, Sajobi TT, Minnella EM, Awasthi R, Loiselle SÈ, et al. Trimodal prehabilitation for colorectal surgery attenuates post-surgical losses in lean body mass: A pooled analysis of randomized controlled trials. Clin Nutr. 2019;38(3):1053-60.
Li C, Carli F, Lee L, Charlebois P, Stein B, Liberman AS, et al. Impact of a trimodal prehabilitation program on functional recovery after colorectal cancer surgery: a pilot study. Surg Endosc. 2013;27(4):1072-82.
Hu WH, Eisenstein S, Parry L, Ramamoorthy S. Risk Factors Associated with Postoperative Outcomes in Diverticular Disease Undergoing Elective Colectomy-A Retrospective Cohort Study from the ACS-NSQIP Database. J Clin Med. 2023;12(23):7338.
Scheede-Bergdahl C, Minnella EM, Carli F. Multi-modal prehabilitation: addressing the why, when, what, how, who and where next? Anaesthesia. 2019;74 Suppl 1:20-6.
Durrand J, Singh SJ, Danjoux G. Prehabilitation. Clin Med (Lond). 2019;19(6):458-64.
Lobo DN, Pavel Skořepa, Gomez D, Greenhaff PL. Prehabilitation: high-quality evidence is still required. Br J Anaesth. 2023;130(1):9-14.
He Y, Zou W, Han X, Chen C, Zhang A, Sun N. Cognitive prehabilitation for geriatric patients undergoing elective surgery: a PRISMA-P-compliant protocol for a systematic review. BMJ Open. 2022;12(7):e060369.
Daksla N, Nguyen V, Jin Z, Bergese SD. Brain Prehabilitation for Oncologic Surgery. Curr Oncol Rep. 2022;24(11):1513-20.
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














