The Correlation between Small Placental Volume Measured by Three-dimensional Ultrasonography and Adverse Pregnancy Outcomes: An Observational Study
DOI:
https://doi.org/10.33192/smj.v76i9.269444Keywords:
Placental volume, 3DUS, adverse pregnancy outcomesAbstract
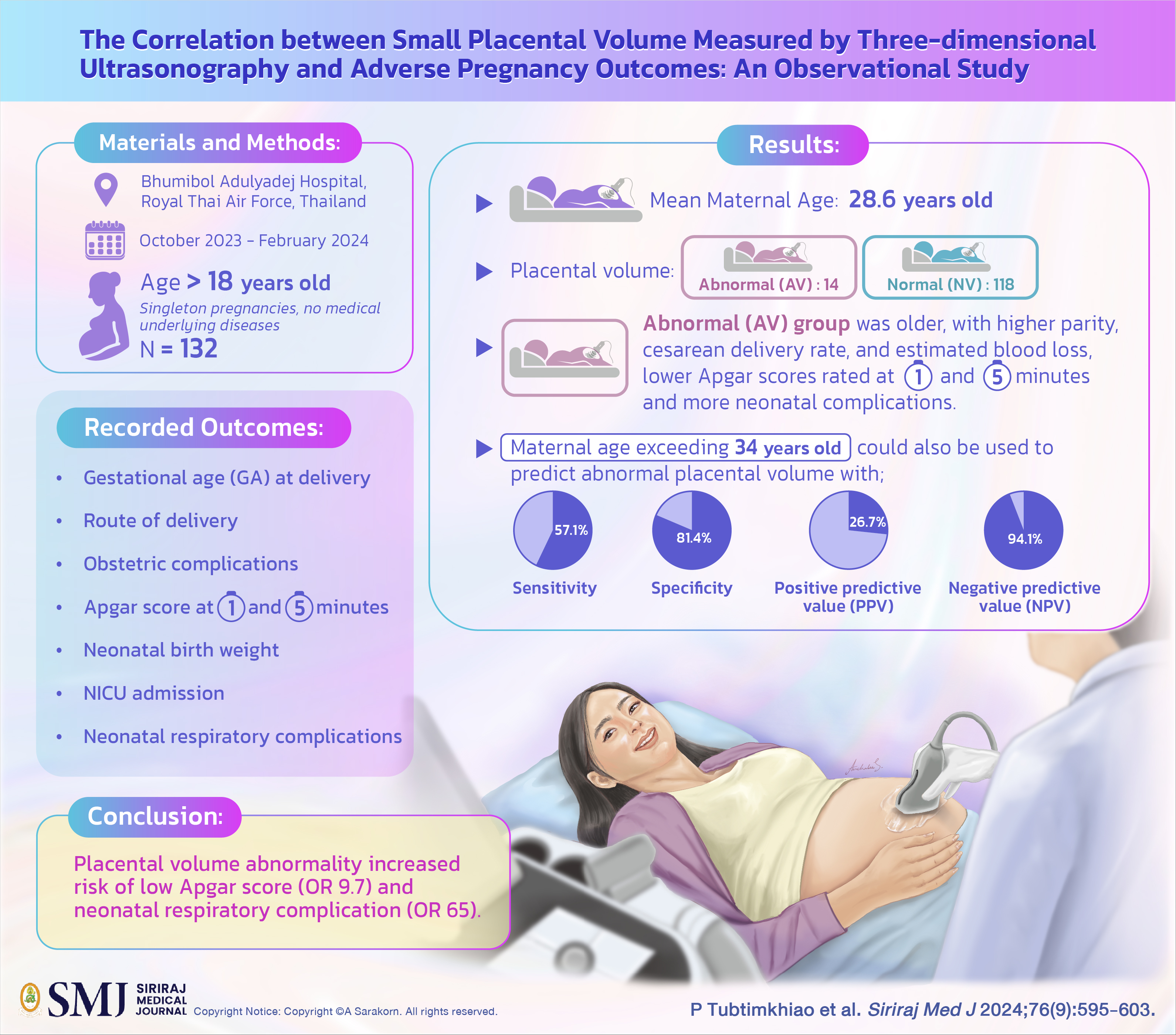
Objective: The placenta is a vital organ in the growth and development of fetuses within the uterus. The size of the placenta is positively associated with fetal well-being. The aim of this study was to investigate any potential correlation between placental volume and negative pregnancy outcomes.
Materials and Methods: This prospective cohort study was conducted at the department of obstetrics and gynecology, Bhumibol Adulyadej Hospital, Thailand between October 2023 and February 2024. Subjects were singleton pregnant women ever the age of 18 without underlying diseases, namely: diabetes mellitus, hypertension, and autoimmune diseases. Ultrasonography was performed between the gestational ages of 28 and 36 weeks. Placental volume was measured via 3-dimensional ultrasonography and analyzed with maternal and neonatal outcomes.
Results: A total of 132 participants were recruited. The mean age of participants was 28.6 years old. The abnormal (AV) and normal (NV) placental volume groups consisted of 14 and 118 cases, respectively. The AV group was older, with higher parity, cesarean delivery rate, and estimated blood loss. This group’s newborns had lower Apgar scores rated at 1 and 5 minutes and more neonatal complications than the NV group (with statistical significance). Maternal age exceeding 34 years could also be used to predict abnormal placental volume with sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) at percentages of 57.1, 81.4, 26.7 and 94.1, respectively.
Conclusion: There is a correlation between placental volume abnormality and certainly adverse outcomes for newborns. Maternal age greater than 34 is associated with higher occurrence of placental volume abnormality.
References
Soongsatitanon A, Phupong V. First trimester 3D ultrasound placental volume for predicting preeclampsia and/or intrauterine growth restriction. J Obstet Gynaecol. 2019; 39:474-9.
Isakov KMM, Emerson JW, Campbell KH, Galerneau F, Anders AM, Lee YK, et al. Estimated Placental Volume and Gestational Age. Am J Perinatol. 2018;35:748-57.
Reijnders IF, Mulders AGMGJ, Koster MPH, Kropman ATM, de Vos ES, Koning AHJ, et al. First-trimester utero-placental (vascular) development and embryonic and fetal growth: The Rotterdam periconception cohort. Placenta. 2021;108:81-90.
Bootchaingam P, Charoenratana C, Tongsong T, Luewan S. Effectiveness of placental volume measured by virtual organ computer-aided analysis in prediction of fetal hemoglobin Bart's disease in late first trimester. J Clin Ultrasound. 2021;49:533-7.
González-González NL, González-Dávila E, González Marrero L, Padrón E, Conde JR, Plasencia W. Value of placental volume and vascular flow indices as predictors of intrauterine growth retardation. Eur J Obstet Gynecol Reprod Biol. 2017;212:13-9.
Soares MJ, Iqbal K, Kozai K. Hypoxia and Placental Development. Birth Defects Res. 2017;109:1309-29.
Liu W, Liu Q, Liu W, Qiu C. Maternal risk factors and pregnancy complications associated with low birth weight neonates in preterm birth. J Obstet Gynaecol Res. 2021;47:3196-202.
Zhang K, Jia X, Yu W, Cheng X, Li Y, Wang X, et al. The associations of gestational weight gain and midpregnancy lipid levels with placental size and placental-to-birth weight ratio: findings from a Chinese birth cohort study. BMC Pregnancy Childbirth. 2023;23:725.
Surányi A, Altorjay Á, Kaiser L, Nyári T, Németh G. Evaluation of placental vascularization by three-dimensional ultrasound examination in second and third trimester of pregnancies complicated by chronic hypertension, gestational hypertension or pre-eclampsia. Pregnancy Hypertens. 2017;8:51-9.
Schwartz N, Oguz I, Wang J, Pouch A, Yushkevich N, Parameshwaran S, et al. Fully Automated Placental Volume Quantification From 3D Ultrasound for Prediction of Small-for-Gestational-Age Infants. J Ultrasound Med. 2022;41:1509-24.
Farina A. Systematic review on first trimester three-dimensional placental volumetry predicting small for gestational age infants. Prenat Diagn. 2016;36:135-41.
WHO. antenatal care recommendations for a positive pregnancy experience: Maternal and fetal assessment update: imaging ultrasound before 24 weeks of pregnancy [Internet]. Geneva: World Health Organization; 2022.
Salinaro JR, McNally PJ, Nickenig Vissoci JR, Ellestad SC, Nelson B, Broder JS. A prospective blinded comparison of second trimester fetal measurements by expert and novice readers using low-cost novice-acquired 3D volumetric ultrasound. J Matern Fetal Neonatal Med. 2021;34:1805-13.
Perkovic-Kepeci S, Cirkovic A, Milic N, Dugalic S, Stanisavljevic D, Milincic M, et al. Doppler Indices of the Uterine, Umbilical and Fetal Middle Cerebral Artery in Diabetic versus Non-Diabetic Pregnancy: Systematic Review and Meta-Analysis. Medicina (Kaunas). 2023;59:1502.
Leung KY. Application of Color Doppler with 3- and 4-Dimensional Ultrasonography in the Prenatal Evaluation of Fetal Extracardiac and Placental Abnormalities. Healthcare (Basel). 2023;11:488.
Santana EFM, Castello RG, Rizzo G, Grisolia G, Araujo Júnior E, Werner H, et al. Placental and Umbilical Cord Anomalies Diagnosed by Two- and Three-Dimensional Ultrasound. Diagnostics (Basel). 2022;12:2810.
Wong CH, Chen CP, Sun FJ, Chen CY. Comparison of placental three-dimensional power Doppler indices and volume in the first and the second trimesters of pregnancy complicated by gestational diabetes mellitus. J Matern Fetal Neonatal Med. 2019;32:3784-91.
Lonimitdee, Kesinee and Sinart Prommas. Placental Weight for Gestational Age and Adverse Neonatal Outcome at Bhumibol Adulyadej Hospital. Thai J Obstet Gynaecol. 2015;23:211-5.
Cunningham FG, Leveno KJ. Implantation and placental development. In: Cunningham FG, Leveno KJ, editors. Williams obstetrics. 26th ed. New York: McGraw Hill Education; 2022.p.82-106.
Stampalija T, Quadrifoglio M, Casati D, Zullino S, Maggi V, Di Martino D, et at. First trimester placental volume is reduced in hypertensive disorders of pregnancy associated with small for gestational age fetus. J Matern Fetal Neonatal Med. 2021;34:1304-11.
Quant HS, Sammel MD, Parry S, Schwartz N. Second-Trimester 3-Dimensional Placental Sonography as a Predictor of Small-for-Gestational-Age Birth Weight. J Ultrasound Med. 2016;35:1693-702.
Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin, Number 222. Obstet Gynecol. 2020;135:e237-60.
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














