Outcomes of Microscopic Residual Tumor after Curative-Intent Surgery in Adenocarcinoma of Esophagogastric Junction
DOI:
https://doi.org/10.33192/smj.v76i11.269480Keywords:
Adenocarcinoma of esophagogastric junction, Microscopic residual tumor, Positive margin, PrognosisAbstract
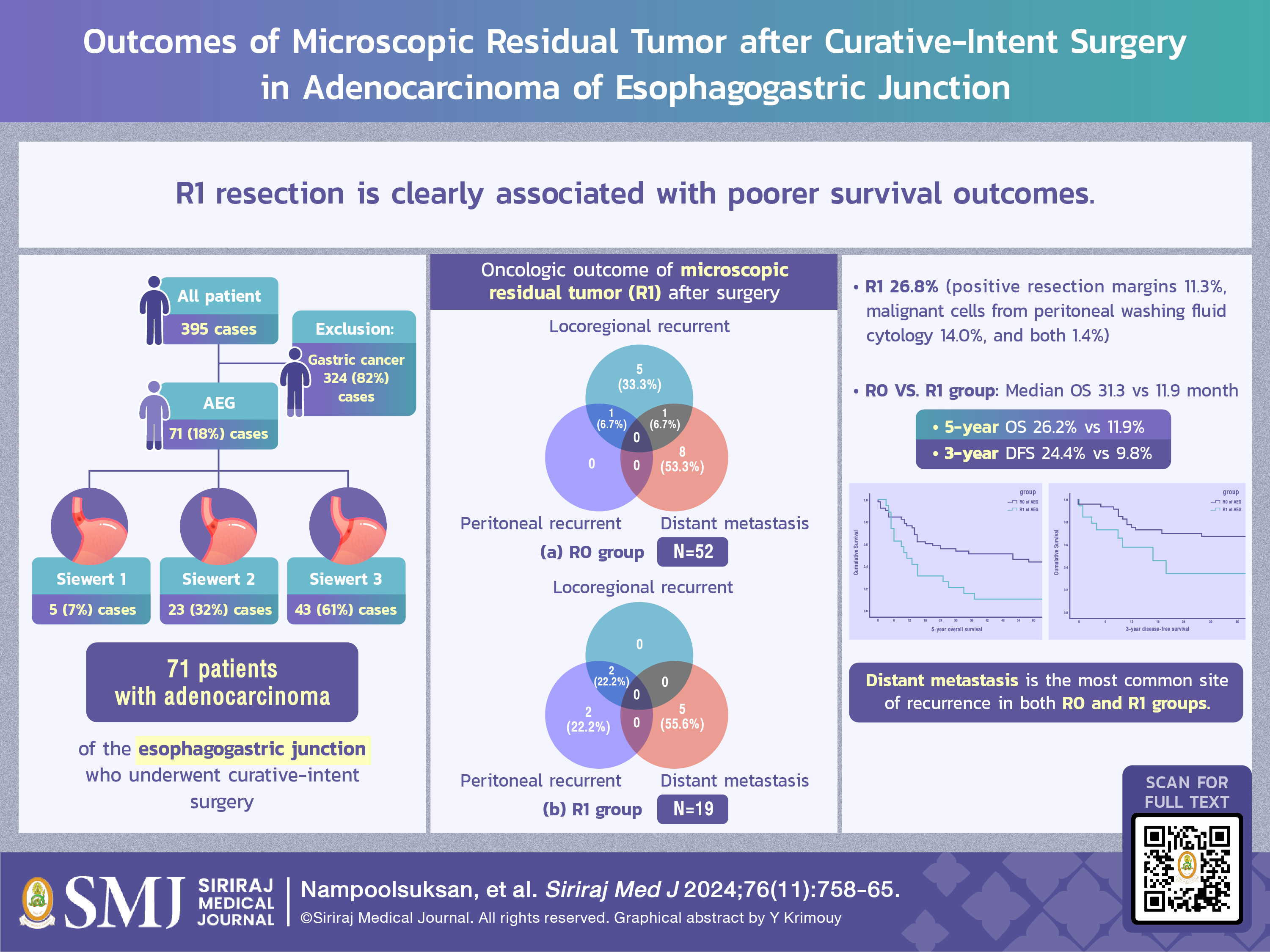
Objective: Radical surgery is the mainstay treatment for adenocarcinoma of the esophagogastric junction. The presence of microscopic residual tumor tissue after curative-intent surgery is associated with recurrence. This study compared the outcomes of patients with microscopic residual tumor (Residual+ group) and those without microscopic residual tumor (Residual- group).
Material and Methods: We retrospectively reviewed the medical records of 71 patients with adenocarcinomas of the esophagogastric junction who underwent curative-intent surgery between January 2005 and August 2018. We evaluated the clinical and pathological characteristics and compared recurrences, rates and patterns, between groups. Five-year overall survival (OS) and 3-year disease-free survival (DFS) were analyzed by Kaplan-Meier analysis.
Results: Nineteen (26.8%) patients had microscopic residual tumors, consisting of 8 (11.3%) with positive resection margins, 10 (14.0%) with malignant cells from peritoneal washing fluid cytology, and 1 (1.4%) with both. The median OS in the Residual- group was significantly better than that in the Residual+ group (31.3 vs 11.9 months, P = 0.003). The Residual- group had better 5-year OS (26.2% vs 11.9%, P = 0.015) and 3-year DFS (24.4% vs 9.8%, P = 0.003) than the Residual+ group. During follow-up period, 48% of the patients in the Residual+ group experienced recurrent disease, with a median follow-up time at 7.7 months. Distant metastasis was the most common site of recurrence.
Conclusion: Microscopic residual tumor after resection is associated with poorer survival outcomes and higher recurrence rates. Curative surgery should aim to achieve R0 resection in all patients with resectable adenocarcinomas of the esophagogastric junction.
References
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101-12.
Buas MF, Vaughan TL. Epidemiology and risk factors for gastro-esophageal junction tumors: understanding the rising incidence of this disease. Semin Radiat Oncol. 2013; 23:3-9.
Hasegawa S, Yoshikawa T. Adenocarcinoma of the esophagogastric junction: incidence, characteristics, and treatment strategies. Gastric Cancer. 2010;13:63-73.
Gao F, Chen J, Wang T, Wang G, Zhang Z, Shen L. Incidence of microscopically positive proximal margins in adenocarcinoma of the gastroesophageal junction. PLoS One. 2014;9(2):e88010.
Siewert J, Stein H. Carcinoma of the gastroesophageal junction-Classification, pathology, and extent of resection. Dis Esophagus.1996;9:173-82.
Siewert J, Feith M. Adenocarcinoma of the esophagogastric junction, results of Surgical Therapy Based on Anatomical/Topographic Classification in 1,002 Consecutive Patients. Ann Surg. 2000;232(3):353-61.
Van Laethem JL, Carneiro F, Ducreux M, Messman H, Lordick F, Ilson DH, et al. The multidisciplinary management of gastro-oesophageal junction tumours: European Society of Digestive Oncology (ESDO): Expert discussion and report from the 16th ESMO World Congress on Gastrointestinal Cancer, Barcelona. Dig Liver Dis. 2016;48(11):1283-9.
Hölscher AH, Law S. Esophagogastric junction adenocarcinomas: individualization of resection with special considerations for Siewert type II, and Nishi types EG, E=G and GE cancers. Gastric Cancer. 2002;23(1):3-9.
Hosokawa Y, Kinoshita T, Konishi M, Takahashi S, Gotohda N, Kato Y, et al. Recurrence patterns of esophagogastric junction adenocarcinoma according to Siewert’s classification after radical resection. Anticancer Res. 2014;34(8):4391-7.
Wang G, Wu A, Cheng X, Ji J. Risk factors associated with early recurrence of adenocarcinoma of gastroesophageal junction after curative resection. Chin J Cancer Res. 2013;25(3):334-8.
Xu H, Zhang L, Miao J, Liu S, Liu H, Jia T, et al. Patterns of recurrence in adenocarcinoma of the esophagogastric junction: a retrospective study. World J Surg Oncol. 2020;18(1):144.
Parakonthun T, Parichardsombat N, Salomon H, Paredes R, Phalanusittheph C, Taweerutchana V, et al. Significance of Microscopic Residual Tumor in Adenocarcinoma of Stomach and Esophagogastric Junction after Gastrectomy with D2 Lymphadenectomy. Siriraj Med J. 2018;70(2):95-102.
Mariette C, Castel B. Surgical management of and long-term survival after adenocarcinoma of the cardia. Br J Surg. 2002;89(9):1156-63.
Greally M, Agarwal R, Ilson DH. Optimal Management of Gastroesophageal Junction Cancer. Cancer 2019;125(12):1990-2001.
Oo AM, Ahmed S. Overview of gastroesophageal junction cancers. Mini-invasive Surg. 2019;3:13.
Kurokawa Y, Sasako M, Doki Y. Treatment Approaches to Esophagogastric Junction Tumors. Dig Surg. 2013;30(2):169-73.
Maruyama S, Imamura Y, Kanie Y, Sakamoto K, Fujiwara D, Okamura A, et al. Recent updates of therapeutic strategy of esophagogastric junction adenocarcinoma. J Cancer Metastasis Treat. 2021;7:53.
Leers JM, DeMeester SR, Chan N, Lipham JC, Hagen JA, DeMeester TR. Clinical characteristics, biologic behavior, and survival after esophagectomy are similar for adenocarcinoma of the gastroesophageal junction and the distal esophagus. J Thorac Cardiovasc Surg. 2009;138(3):594-602.
Carboni F, Lorusso R, Santoro R, Lepiane P, Mancini P, Sperduti I, et al. Adenocarcinoma of the esophagogastric junction : the role of abdominal-transhiatal resection . Ann Surg Oncol. 2009; 16(2):304-10.
Bissolati M, Desio M, Rosa F, Rausei S, Marrelli D, Baiocchi GL, et al. Risk factor analysis for involvement of resection margins in gastric and esophagogastric junction cancer: an Italian multicenter study. Gastric Cancer. 2017; 20(1):70-82 .
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














