Correlation of American Urological Association Symptom Index Domains with Uroflowmetric Peak Flow in Thai Patients with Suspected Benign Prostatic Hyperplasia
DOI:
https://doi.org/10.33192/smj.v76i11.269863Keywords:
BPH, Benign Prostatic Hyperplasia, AUA-SI, UroflowmetryAbstract
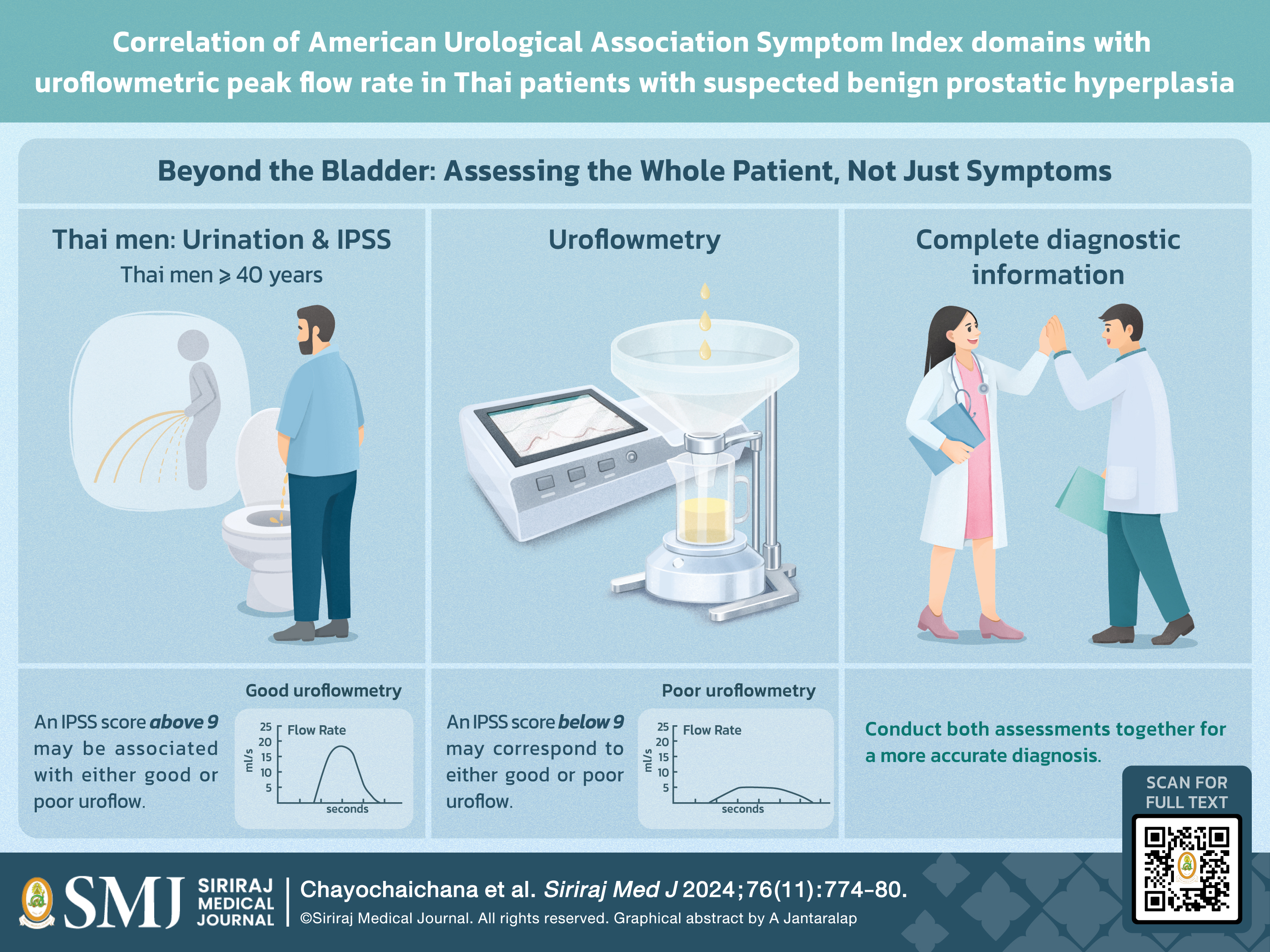
Objective: This study aimed to investigate the correlations between the obstructive and irritative domain scores of the total AUA-SI and the uroflowmetric peak flow rate (Qmax) in Thai patients suspected of having benign prostatic hyperplasia (BPH).
Materials and Methods: A retrospective observational study was conducted on 510 patients who presented with lower urinary tract symptoms (LUTSs) and were suspected of having BPH at the Urology Outpatient Department of King Chulalongkorn Memorial Hospital, Thailand. A self-administered AUA-SI score was used to determine the severity of symptoms, and uroflowmetry was conducted to determine parameters, including flow rate variable.
Results: A significant correlation was observed between the AUA-SI score and uroflowmetric peak flow (Qmax). The AUA-SI and its obstructive domain had weak negative Pearson correlations with uroflowmetric peak flow (r = −0.164 and −0.185, respectively; P < 0.01). The irritative domain was inversely associated with Qmax (r = 0.097, P = 0.028). However, when patients in each subgroup with mild (AUA-SI = 0 - 7), moderate (AUA-SI = 8–19), and severe symptoms (AUA-SI = 20–35) were considered, the relationship was found to be not significant.
Conclusion: The study revealed a significant weak negative correlation between the AUA-SI score and Qmax, but no significant correlations were found between the obstructive and irritative domains and Qmax in the subgroup analysis.
References
Platz EA, Joshu CE, Mondul AM, Peskoe SB, Willett WC, Giovannucci E. Incidence and progression of lower urinary tract symptoms in a large prospective cohort of United States men. J Urol. 2012;188(2):496-501.
Chughtai B, Forde JC, Thomas DDM, Laor L, Hossack T, Woo HH, Te AE, Kaplan SA. Benign prostatic hyperplasia. Nat Rev Dis Primers. 2016;2:16031.
Roehrborn CG, McConnell JD. Etiology, pathophysiology, epidemiology and natural history of benign prostatic hyperplasia. In: Walsh PC, Retik AB, Vaughan ED, Wein AJ, editors. Campbell’s Urology. 8th ed. Philadelphia: Saunders; 2002.p.1297-336.
Speakman M, Kirby R, Doyle S, Ioannou C. Burden of male lower urinary tract symptoms (LUTS) suggestive of benign prostatic hyperplasia (BPH) - focus on the UK. BJU Int. 2015;115(4):508-19.
Hongthong P, Santingamkun A. Correlation evaluation of a new visual prostate symptom score and the international prostate symptom score in Thai men with lower urinary tract symptoms. Insight Urol. 2013;34(2):29-35.
Nontakaew K, Kochakarn W, Kijvika K, Viseshsindh W, Silpakit C. Reliability of a Thai version of the International Prostate Symptom Score (IPSS) for the Thai population. J Med Assoc Thai. 2014;97(6):615-20.
Setthawong V, Mahawong P, Pattanachindakun N, Amnattrakul P, Dar FM, Thanavongvibul S. To investigate the correlation between the visual prostate symptom score, the international prostate symptom score, and uroflowmetry parameters in adult Thai males of different educational levels. Prostate Int. 2018;6(3):115-8.
Ezz el Din K, Kiemeney LA, de Wildt MJ, Debruyne FM, de la Rosette JJ. Correlation between uroflowmetry, prostate volume, postvoid residue, and lower urinary tract symptoms as measured by the International Prostate Symptom Score. Urology. 1996;48(3):393-7.
Bautista OM, Kusek JW, Nyberg LM, McConnell JD, Bain RP, Miller G, Crawford ED, et al. Study design of the Medical Therapy of Prostatic Symptoms (MTOPS) trial. Control Clin Trials. 2003;24(2):224-43.
Wehrberger C, Madersbacher S, Jungwirth S, Fischer P, Tragl KH. Lower urinary tract symptoms and urinary incontinence in a geriatric cohort - a population-based analysis. BJU Int. 2012;110(10):1516-21.
Roehrborn CG, Boyle P, Bergner D, Gray T, Gittelman M, Shown T, Melman A, et al. Serum prostate-specific antigen and prostate volume predict long-term changes in symptoms and flow rate: results of a four-year, randomized trial comparing finasteride versus placebo. PLESS Study Group. Urology. 1999;54(4):662-9.
Oranusi CK, Nwofor AE, Mbonu O. Correlation between International Prostate Symptom Score and uroflowmetry in patients with benign prostatic hyperplasia. Niger J Clin Pract. 2017;20(4):454-8.
Zambon JP, da Silva Batezini NS, Karam AJ, Oliveira Conceição RD, de Carvalho JAM, Almeida FG. Uroflowmetry in a large population of Brazilian men submitted to a health check up program and its correlation with IPSS and prostate size. Int Braz J Urol. 2013;39(6):841-6.
Chatterjee S, Kumar A, Pal DK. Study of correlation between visual prostate symptom score and international prostate symptom score in men with lower urinary tract symptoms with reference to uroflowmetry parameters in Indian population. Urologia. 2023;90(2):377-80.
Yee CH, Li JK, Lam HC, Chan ES, Hou SS, Ng CF. The prevalence of lower urinary tract symptoms in a Chinese population, and the correlation with uroflowmetry and disease perception. Int Urol Nephrol. 2014;46(4):703-10.
Bhomi KK, Subedi N, Panta PP. Correlation of visual prostate symptom score with international prostate symptom score and uroflowmetry parameters in Nepalese male patients with lower urinary tract symptoms. JNMA J Nepal Med Assoc. 2017;56(206):217-20.
Keskin MZ, Karaca E, Uçar M, Ateş E, Yücel C, İlbey YÖ. Comparison of uroflowmetry tests performed with a sensation of normal desire to void versus urgency and correlation of test results with IPSS. Turk J Urol. 2020;46(5):378-82.
Abhulimen V, Raphael JE. Correlation between uroflowmetry and International Prostate Symptoms Score in the evaluation of Nigerian men with benign prostatic enlargement. Niger Med J. 2021;62(5):219-25.
Affusim EA, Amu OC, Eneje CL, Iwenofu C, Ugwumba F. Correlation between physician-administered International Prostate Symptoms Score and peak urine flow rate in assessment of benign prostatic enlargement patients. Niger J Clin Pract. 2023;26(11):1642-6.
Huang Foen Chung JWNC, van Mastrigt R. Correlation of non-invasive urodynamics with International Prostate Symptom Score (IPSS) and prostate volume. Neurourol Urodyn. 2005;24(1):25-30.
Sabnis RB, Mulawkar PM, Joshi RN. The Urological Society of India guidelines on management of benign prostatic hyperplasia/benign prostatic obstruction (executive summary). Indian J Urol. 2021;37(3):210-3.
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














