Success Rates and Prognostic Factors in the Management of Keratoconus: A 10-Year Retrospective Cohort Study at Siriraj Hospital
DOI:
https://doi.org/10.33192/smj.v76i12.269895Keywords:
Keratoconus, Success rate, Progression, Contact lensAbstract
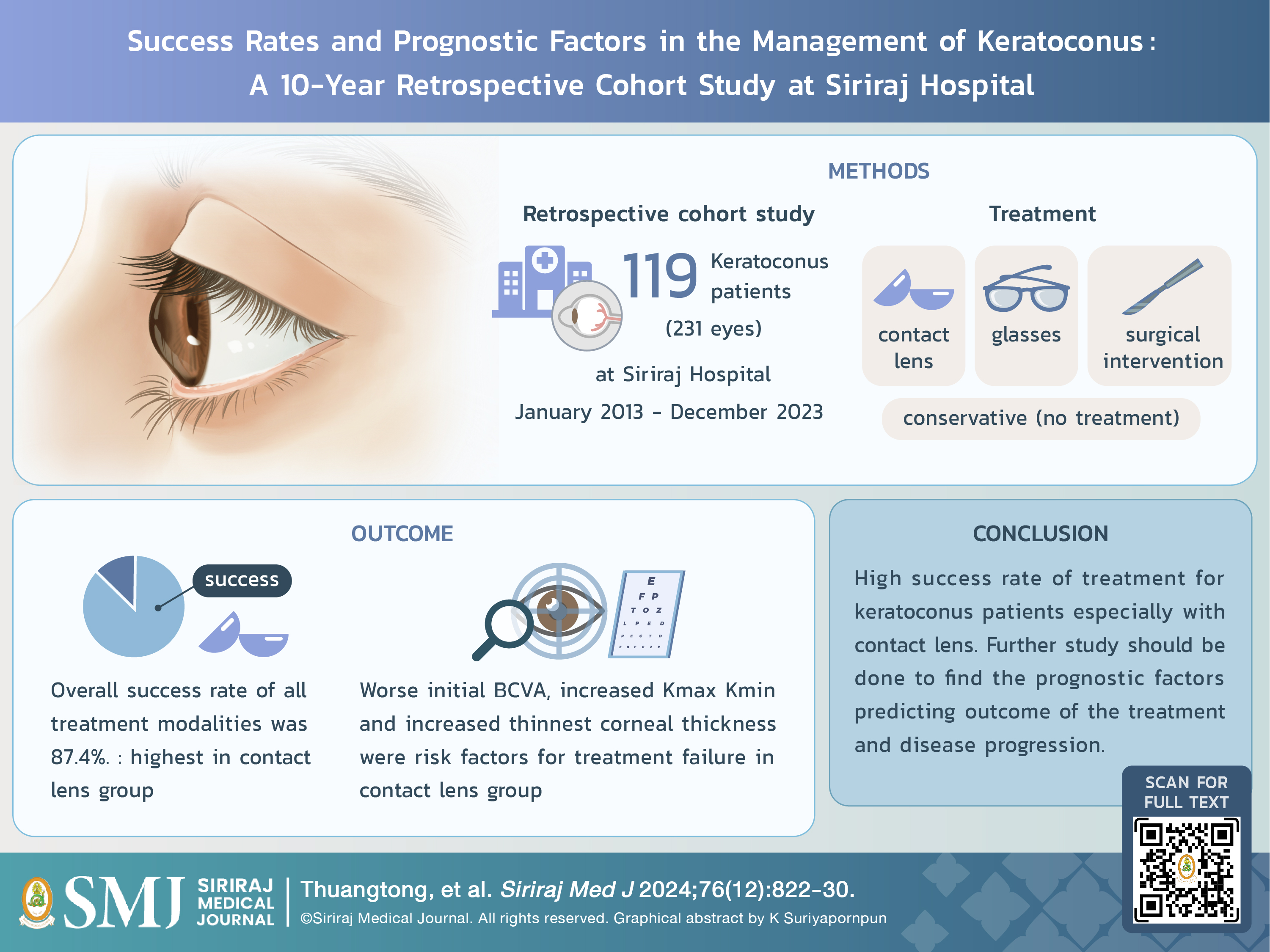
Objective: To evaluate the success rates of different treatment modalities, identify prognostic factors associated with treatment outcomes and factors influencing disease progression in keratoconus patients.
Materials and Methods: A retrospective cohort study of keratoconus patients at Siriraj Hospital during January 2013 to December 2023 was done. Patient characteristics, symptoms and signs related to keratoconus, outcomes of corneal topography, treatment modalities, and best-corrected visual acuity (BCVA) before and after treatment were recorded. Treatment outcome was defined as a “success” when the BCVA post-treatment was equal to or better than 6/12. Progression of keratoconus was based on the Belin ABCD progression criteria.
Results: Total 119 patients (231 eyes) were analyzed. The mean age at diagnosis was 28.0 ± 9.5 years. Two hundred and sixteen eyes (93.5%) were clinical keratoconus. The overall success rate of all treatment modalities was 87.4%. Contact lenses were the most frequent treatment modality (147 eyes, 72.4%) with the highest success rate (90.5%). A worse initial BCVA, high keratometric reading and thinner cornea were risk factors for treatment failure in this group. Of 133 eyes disease progression could be evaluated (median follow-up time; 33 months) and 58 eyes
(43.6%) met criteria for disease progression (median survival time; 8.8 years). No significant factors were found to be associated with disease progression.
Conclusion: Success rate in keratoconus treatment at Siriraj Hospital was 87.4%. Contact lenses were most frequently applied 72.4%. Factors associated with treatment failure were found in this group but for disease progression
remained unclear due to limitations of the study.
References
Ferdi A, Nguyen V, Kandel H, Tan JC, Arnalich-Montiel F, Abbondanza M, et al. Predictors of progression in untreated keratoconus: a Save Sight Keratoconus Registry study. Br J Ophthalmol. 2022;106(9):1206-11.
Thuangtong A, Samsen P, Boonyakiatwatana S. Clinical Characteristics of Patients in Contact Lens Clinic, Siriraj Hospital. Siriraj Med J. 2012;64(1):7-10.
Arnold A, Dunn R, Taylor H, Keeffe J, Fox S, Goujon N, et al. National indigenous eye health survey: Minum Barreng (Tracking Eyes). National indigenous eye health survey: Minum Barreng (Tracking Eyes). 2009.
Wollensak G. Crosslinking treatment of progressive keratoconus: new hope. Curr Opin Ophthalmol. 2006;17(4):356-60.
Shabayek MH, Alió JL. Intrastromal corneal ring segment implantation by femtosecond laser for keratoconus correction. Ophthalmology. 2007;114(9):1643-52.
Chotikavanich S, Kosrirukvongs P, Duangpatra J, Prabhasawat P, Booranapong W, Chirapapaisan C, et al. A two-year outcome of intrastromal corneal ring segment implantation in keratoconus: Initial report in Thai patients. Siriraj Med J. 2019;71(4):302-9.
Rico-Del-Viejo L, Garcia-Montero M, Hernández-Verdejo JL, García-Lázaro S, Gómez-Sanz FJ, Lorente-Velázquez A. Nonsurgical Procedures for Keratoconus Management. J Ophthalmol. 2017;2017:9707650.
Abdalla YF, Elsahn AF, Hammersmith KM, Cohen EJ. SynergEyes lenses for keratoconus. Cornea. 2010;29(1):5-8.
Itoi M, Itoi M. Management of keratoconus with corneal rigid gas-permeable contact lenses. Eye Contact Lens. 2022;48(3):110-4.
Mandathara PS, Stapleton FJ, Willcox MD. Outcome of keratoconus management: review of the past 20 years' contemporary treatment modalities. Eye Contact Lens. 2017;43(3):141-54.
Ozalp O, Atalay E. Belin ABCD Progression Display identifies keratoconus progression earlier than conventional metrics. Am J Ophthalmol. 2022;236:45-52.
Tuft SJ, Moodaley LC, Gregory WM, Davison CR, Buckley RJ. Prognostic factors for the progression of keratoconus. Ophthalmology. 1994;101(3):439-47.
Wagner H, Barr J, Zadnik K, Group CLEoKS. Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study: methods and findings to date. Contact Lens Anterior Eye. 2007;30(4):223-32.
Rabinowitz YS. Videokeratographic indices to aid in screening for keratoconus. J Refract Surg. 1995;11(5):371-9.
Amsler M. The" forme fruste" of keratoconus. Wiener Klin Wochenschr. 1961;73:842-3.
Gomes JA, Tan D, Rapuano CJ, Belin MW, Ambrósio Jr R, Guell JL, et al. Global consensus on keratoconus and ectatic diseases. Cornea. 2015;34(4):359-69.
Piyacomn Y, Kasetsuwan N, Puangsricharern V, Reinprayoon U, Satitpitakul V, Chantaren P. Keratoconus in Thai population–a cross-sectional hospital-based study. Asian Biomedicine. 2022;16(6):316-21.
Gokul A, Patel DV, Watters GA, McGhee CN. The natural history of corneal topographic progression of keratoconus after age 30 years in non-contact lens wearers. Br J Ophthalmol. 2017;101(6):839-44.
Choi JA, Kim M-S. Progression of keratoconus by longitudinal assessment with corneal topography. Invest Ophthalmol Vis Sci. 2012;53(2):927-35.
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














