Comparative Evaluation of Phacoemulsification with Goniosynechialysis and Phacoemulsification with Viscogonioplasty in Angle-Closure: A Randomized Clinical Trial
DOI:
https://doi.org/10.33192/smj.v76i12.270908Keywords:
Phacoemulsification, Goniosynechialysis, Viscogonioplasty, Angle-closure, Primary angle-closure glaucomaAbstract
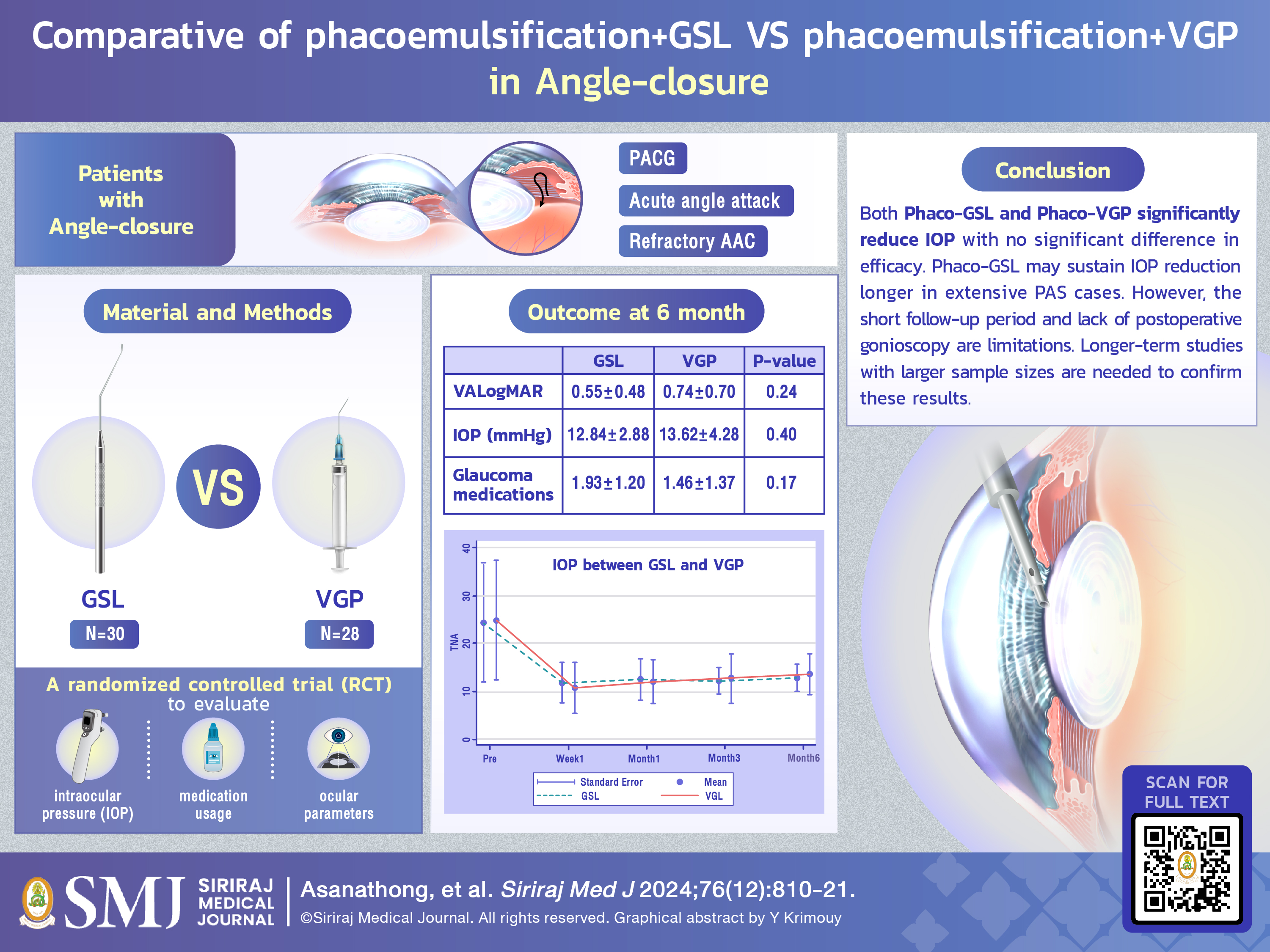
Objective: To compare the effects of phacoemulsification with goniosynechialysis (GSL) versus viscogonioplasty (VGP) on intraocular pressure (IOP) reduction and medication use in angle-closure patients.
Materials and Methods: This randomized controlled trial at Sisaket Hospital, Thailand, from November 2021 to May 2024, enrolled patients with angle-closure and cataracts. Group 1 underwent phacoemulsification with GSL, and Group 2 with VGP. Visual acuity, IOP, and medication use were assessed before surgery, then at 1 week, 1 month, 3 months, and 6 months post-surgery.
Results: 58 eyes were included: 30 in Group 1 and 28 in Group 2. The average age was 67.16±9.65 years in Group 1 and 67.78±7.38 years in Group 2 (P=0.79). Baseline IOP was 24.31±12.34 mmHg in Group 1 and 24.92±12.50 mmHg in Group 2 (P=0.85). After 6 months, IOP decreased to 12.84±2.88 mmHg in Group 1 and 13.62±4.28 mmHg in Group 2 (P=0.40). Glaucoma medications decreased from 3.47±0.94 to 1.93±1.20 in Group 1 and from 3.54±0.58 to 1.46±1.37 in Group 2 (P=0.17). Hazard ratio: 4.29 (P=0.066, 95% CI: 0.91–20.18).
Conclusion: Both Phaco-GSL and Phaco-VGP significantly reduce IOP, with no significant difference in efficacy. Phaco-GSL may sustain IOP reduction longer in extensive PAS cases. However, the short follow-up period and lack of postoperative gonioscopy are limitations. Longer-term studies with larger sample sizes are needed to confirm these results.
References
European Glaucoma Society Terminology and Guidelines for Glaucoma, 4th Edition - Chapter 3: Treatment principles and options Supported by the EGS Foundation. Br J Ophthalmol. 2017;101(6):130-95.
Teekhasaenee C. Combined phacoemulsification and goniosynechialysis for uncontrolled chronic angle-closure glaucoma after acute angle-closure glaucoma. Ophthalmology. 1999;106(4):669-74.
Anderson DR, Jai Chi Jin, Wright MM. The Physiologic Characteristics of Relative Pupillary Block. Am J Ophthalmol. 1991;111(3):344-50.
Husain R, Gazzard G, Aung T, Chen Y, Padmanabhan V, Oen FTS, et al. Initial management of acute primary angle closure: a randomized trial comparing phacoemulsification with laser peripheral iridotomy. Ophthalmology [Internet]. 2012 Nov 1 [cited 2021 Aug 8];119(11):2274–81. Available from: https://pubmed.ncbi.nlm.nih.gov/22885123/
Lam DSC, Leung DYL, Tham CCY, Li FCH, Kwong YYY, Chiu TYH, et al. Randomized Trial of Early Phacoemulsification versus Peripheral Iridotomy to Prevent Intraocular Pressure Rise after Acute Primary Angle Closure. Ophthalmology. 2008 ;115(7):1134-40.
Petchyim S. Secondary Acute Angle-Closure Attack: Diagnosis and Management. Siriraj Med J [Internet]. 2018 Mar. 9 [cited 2024 Oct. 26];70(1):91-4. Available from: https://he02.tci-thaijo.org/index.php/sirirajmedj/article/view/114934
Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global Prevalence of Glaucoma and Projections of Glaucoma Burden through 2040. Ophthalmology [Internet]. 2014 Nov;121(11):2081–90. Available from: https://www.aaojournal.org/article/S0161-6420(14)00433-3/fulltext
Zhang N, Wang J, Chen B, Li Y, Jiang B. Prevalence of Primary Angle Closure Glaucoma in the Last 20 Years: A Meta-Analysis and Systematic Review. Front Med (Lausanne). 2021;7:624179.
Knighton EA, Zoltoski RK, Roberts DK, Wilensky JT, Kuszak JR. Rate of Increase in Lens Thickness Decreases With Age. Investigative Ophthalmology & Visual Science [Internet]. 2011 Apr 22 [cited 2024 Sep 2];52(14):1540–0. Available from: https://iovs.arvojournals.org/article.aspx?articleid=2352248
Shin HC, Subrayan V, Tajunisah I. Changes in anterior chamber depth and intraocular pressure after phacoemulsification in eyes with occludable angles. J Cataract Refract Surg. 2010;36(8):1289-95.
Tai MC, Chien KH, Lu DW, Chen JT. Angle changes before and after cataract surgery assessed by Fourier-domain anterior segment optical coherence tomography. J Cataract Refract Surg. 2010;36(10):1758-62.
Huang G, Gonzalez E, Lee R, Chen YC, He M, Lin SC. Association of biometric factors with anterior chamber angle widening and intraocular pressure reduction after uneventful phacoemulsification for cataract. J Cataract Refract Surg. 2012;38(1):108-16.
H Viet Tran, Liebmann JM, Ritch R. Iridociliary apposition in plateau iris syndrome persists after cataract extraction. Am J Ophthalmol. 2003;135(1):40-3.
Yang CH, Hung PT. Intraocular lens position and anterior chamber angle changes after cataract extraction in eyes with primary angle-closure glaucoma. J Cataract Refract Surg. 1997;23(7):1109-13.
Tham CCY, Leung DYL, Kwong YYY, Li FCH, Lai JSM, Lam DSC. Effects of phacoemulsification versus combined phaco-trabeculectomy on drainage angle status in primary angle closure glaucoma (PACG). Journal of Glaucoma [Internet]. 2010 [cited 2019 Nov 13];19(2):119–23. Available from: https://www.ncbi.nlm.nih.gov/pubmed/19373107
Yu JG, Zhao F, Xiang Y. Phacoemulsification with Goniosynechialysis versus Phacoemulsification Alone in Angle-Closure Glaucoma: A Meta-Analysis of Randomized Controlled Trials. J Ophthalmol. 2021;2021:8831479.
Wang N, Jia S-B. Phacoemulsification with or without goniosynechialysis for angle-closure glaucoma: a global Meta-analysis based on randomized controlled trials. Int J Ophthalmol. 2019;12(5):826-33.
Wanichwecharungruang B, Phumratprapin C, Kongsomboon K, Seresirikachorn K. Real-world Surgical Outcomes of Primary Angle-closure Glaucoma. Clin Ophthalmol. 2021;15:2823-33.
Tian T, Li M, Pan Y, Cai Y, Fang Y. The effect of phacoemulsification plus goniosynechialysis in acute and chronic angle closure patients with extensive goniosynechiae. BMC Ophthalmol. 2019;19(1):65.
Husain R, Do T, Lai J, Kitnarong N, Nongpiur ME, Perera SA, et al. Efficacy of Phacoemulsification Alone vs Phacoemulsification With Goniosynechialysis in Patients With Primary Angle-Closure Disease. JAMA Ophthalmol. 2019;137(10):1107-13.
Campbell DG, Vela A. Modern Goniosynechialysis for the Treatment of Synechial Angle-closure Glaucoma. Ophthalmology. 1984;91(9):1052-60.
Angmo D, Shakrawal J, Gupta B, Yadav S, Pandey RM, Dada T. Comparative Evaluation of Phacoemulsification Alone versus Phacoemulsification with Goniosynechialysis in Primary Angle-Closure Glaucoma. Ophthalmol Glaucoma. 2019;2(5):346-56.
Varma D, Baylis O, Wride N, Phelan PS, Fraser SG. Viscogonioplasty: an effective procedure for lowering intraocular pressure in primary angle closure glaucoma. Eye [Internet]. 2006 Jan 13 [cited 2019 Nov 13];21(4):472-5. Available from: https://www.nature.com/articles/6702224
Fraser S, Adams, Varma, Phelan P, Bunce C, Fraser S. Viscogonioplasty in narrow angle glaucoma: a randomized controlled trial. Clin Ophthalmol. 2010;4:1475-9.
Eslami Y, Latifi G, Moghimi S, Ghaffari R, Fakhraie G, Zarei R, et al. Effect of adjunctive viscogonioplasty on drainage angle status in cataract surgery: a randomized clinical trial. Clin Exp Ophthalmol [Internet]. 2012 Oct 29 [cited 2019 Nov 13];41(4):368-78. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/j.1442-9071.2012.02871.x
Moghimi S, Latifi G, ZandVakil N, Mohammadi M, Khatibi N, Soltani-Moghadam R, et al. Phacoemulsification Versus Combined Phacoemulsification and Viscogonioplasty in Primary Angle-Closure Glaucoma: A Randomized Clinical Trial. J Glaucoma [Internet]. 2015 [cited 2019 Nov 13];24(8):575-82. Available from: http://journals.lww.com/glaucomajournal/Abstract/2015/10000/Phacoemulsification_Versus_Combined.3.aspx
Tian T, Li M, Pan Y, Cai Y, Fang Y. The effect of phacoemulsification plus goniosynechialysis in acute and chronic angle closure patients with extensive goniosynechiae. BMC Ophthalmol. 2019;19(1):65.
Kitnarong N, Dagvadorj D. Effect of Multifocal Intraocular Lens on Contrast Sensitivity in Primary Angle-Closure Patients. Siriraj Med J [Internet]. 2023 Jul. 1 [cited 2024 Oct. 26];75(7):501-7. Available from: https://he02.tci-thaijo.org/index.php/sirirajmedj/article/view/263254
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














