Post-biopsy to Surgery Interval Tends to Increase Axillary Nodal Metastasis, Especially in Early Breast Cancer Patients
DOI:
https://doi.org/10.33192/smj.v76i12.270986Keywords:
breast cancer, time to surgery, lymph node stagingAbstract
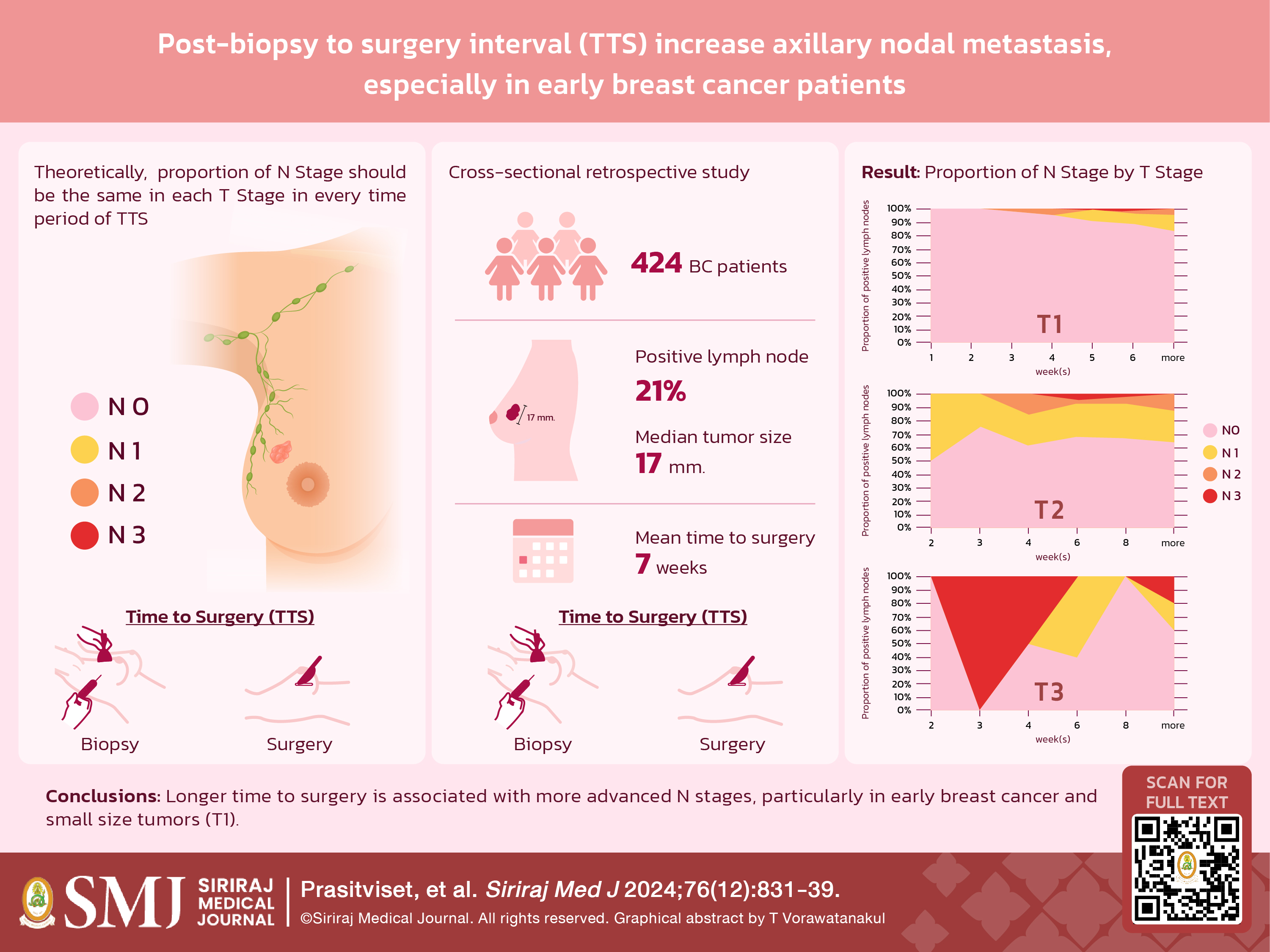
Objective: Delays between diagnosis and breast cancer surgery may raise concerns about tumor progression. Tumors of the same size should exhibit same proportions of N staging. We aimed to evaluate the impact of time to surgery (TTS) on the proportion of metastatic axillary lymph nodes (N-Staging), controlled by tumor size.
Materials and Methods: A cross-sectional study of primary breast cancer patients treated between October 2021 - December 2022 at the Division of Head Neck and Breast Surgery, Siriraj Hospital, Thailand examined the association between lymph node staging and TTS, stratified by primary tumor size. Patients with neoadjuvant therapy, DCIS, or underwent excisional biopsy were excluded.
Results: Of 424 patients, mean age 60.95 years, had an average tumor size 17±13.38 mm, and 20.8% LNs metastasis. The mean TTS was 7 ± 3.11 weeks. The proportion of + LNs patients stratified by tumor size was 10.6% for T1, 34.56% for T2, and 43.75% for T3 lesions. There was no significant difference between TTS and the proportion of
N-staging for all T2 and T3 tumors. In contrast, a significant finding was observed among T1 tumors. Axillary nodal metastasis became more advanced as TTS increased (p-value = 0.022); and increased N2 and N3 nodal staging was noted in patients with delayed surgery. No significant additional differences were found concerning breast cancer subtype, pathological grading, or lympho-vascular/perineural invasion.
Conclusion: Increasing TTS was significantly associated with more advanced N staging. This finding highlights the need for timely intervention in early breast cancer, particularly in T1 tumors.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66(1):7-30.
Rosenberg J, Chia YL, Plevritis S. The effect of age, race, tumor size, tumor grade, and disease stage on invasive ductal breast cancer survival in the U.S. SEER database. Breast Cancer Res Treat. 2005;89(1):47-54.
Fitzgibbons PL, Page DL, Weaver D, Thor AD, Allred DC, Clark GM, et al. Prognostic factors in breast cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med. 2000;124(7):966-78.
Axelsson CK, Mouridsen HT, Zedeler K. Axillary dissection of level I and II lymph nodes is important in breast cancer classification. The Danish Breast Cancer Cooperative Group (DBCG). Eur J Cancer. 1992;28a(8-9):1415-8.
Beenken SW, Urist MM, Zhang Y, Desmond R, Krontiras H, Medina H, et al. Axillary lymph node status, but not tumor size, predicts locoregional recurrence and overall survival after mastectomy for breast cancer. Ann Surg. 2003;237(5):732-8; discussion 8-9.
Stevens A, Lowe JS, Scott I, Stevens A. Core pathology. 3rd ed. St. Louis, Mo: Elsevier; 2009.
Dahan M, Hequet D, Bonneau C, Paoletti X, Rouzier R. Has tumor doubling time in breast cancer changed over the past 80 years? A systematic review. Cancer Med. 2021;10(15):5203-17.
Carter CL, Allen C, Henson DE. Relation of tumor size, lymph node status, and survival in 24,740 breast cancer cases. Cancer. 1989;63(1):181-7.
Sivaramakrishna R, Gordon R. Detection of breast cancer at a smaller size can reduce the likelihood of metastatic spread: a quantitative analysis. Acad Radiol. 1997;4(1):8-12.
Laura S, Coombs NJ, Ung O, Boyages J. Tumour size as a predictor of axillary node metastases in patients with breast cancer. ANZ J Surg. 2006;76(11):1002-6.
Yu KD, Jiang YZ, Shao ZM. Difference between observed and expected number of involved lymph nodes reflects the metastatic potential of breast cancer independent to intrinsic subtype. Oncotarget. 2015;6(18):16686-97.
Richards MA, Westcombe AM, Love SB, Littlejohns P, Ramirez AJ. Influence of delay on survival in patients with breast cancer: a systematic review. Lancet. 1999;353(9159):1119-26.
Bleicher RJ, Ruth K, Sigurdson ER, Beck JR, Ross E, Wong YN, et al. Time to Surgery and Breast Cancer Survival in the United States. JAMA Oncol. 2016;2(3):330-9.
Sopik V, Narod SA. The relationship between tumour size, nodal status and distant metastases: on the origins of breast cancer. Breast Cancer Res Treat. 2018;170(3):647-56.
Wo JY, Chen K, Neville BA, Lin NU, Punglia RS. Effect of very small tumor size on cancer-specific mortality in node-positive breast cancer. J Clin Oncol. 2011;29(19):2619-27.
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














