A Survey of Home-Based Cognitive Stimulation Activities in Thai Patients with Mild Cognitive Impairment and Mild Dementia
DOI:
https://doi.org/10.33192/smj.v77i1.271344Keywords:
home-based activity, cognitive activity, mild cognitive impairment, mild dementia, ThaiAbstract
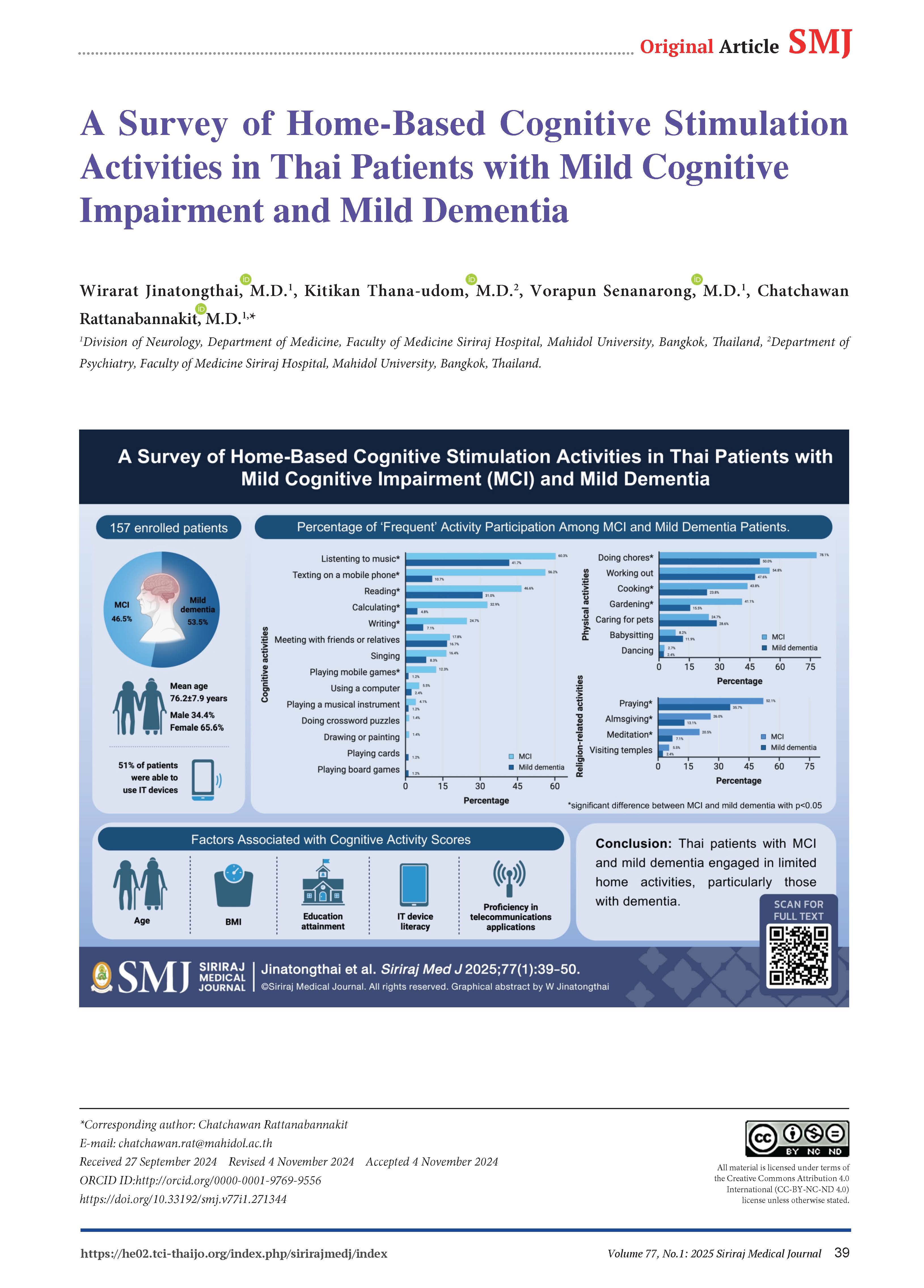
Objective: This study investigated the characteristics of home-based activities in individuals with mild cognitive impairment (MCI) and mild dementia, as well as factors related with those activities.
Materials and Methods: A cross-sectional, questionnaire-based study was conducted on patients with MCI and mild dementia at Siriraj Hospital. Data on patient and caregiver characteristics, home cognitive activities, and proficiency in using information technology (IT) devices and telecommunications applications were collected. Home activities were categorized into cognitive, physical, and religion-related activities based on their type and frequency.
Results: Of 157 enrolled patients with a mean age of 76.2±7.9 years, 46.5% were diagnosed with MCI and 53.5% with mild dementia. The MCI group exhibited significantly higher frequencies of activities such as reading, writing, playing mobile games, texting, calculating, music listening, meditation, praying, almsgiving, doing chores, cooking, and gardening (all p<0.05). Approximately 51% of patients were able to use IT devices. MCI patients demonstrated greater proficiency in using smart IT devices and teleconferencing applications than those with mild dementia (79.5% vs. 26.2%, and 49.3% vs. 11.9%, both p<0.001). Cognitive activity scores were associated with age (r=-0.34, p<0.001), body mass index (r=0.16, p=0.04), educational attainment (r=0.38, p<0.001), IT device literacy (r=0.41, p<0.001), and proficiency in using telecommunications applications (r=0.55, p<0.001).
Conclusion: Thai patients with MCI and mild dementia engaged in limited home activities, particularly those with dementia. IT device literacy was surprisingly prevalent and contributed to higher cognitive activity scores. Developing home-based cognitive stimulation programs for Thai patients facing cognitive challenges utilizing telecommunication may be feasible.
References
Verghese J, Lipton RB, Katz MJ, Hall CB, Derby CA, Kuslansky G, et al. Leisure activities and the risk of dementia in the elderly. N Engl J Med. 2003;348(25):2508-16.
Pothisiri W. COVID-19 and older persons: Evidence from the survey in Thailand: The United Nations Population Fund (UNFPA) Thailand; 2020 [cited 2022 Feb 16]. Available from: https://thailand.unfpa.org/sites/default/files/pub-pdf/covid-19_report-online-revised_2021.pdf.
Tondo G, Sarasso B, Serra P, Tesser F, Comi C. The Impact of the COVID-19 Pandemic on the Cognition of People with Dementia. Int J Environ Res Public Health. 2021;18(8).
Ismail, II, Kamel WA, Al-Hashel JY. Association of COVID-19 Pandemic and Rate of Cognitive Decline in Patients with Dementia and Mild Cognitive Impairment: A Cross-sectional Study. Gerontol Geriatr Med. 2021;7:23337214211005223.
Bahar‐Fuchs A, Martyr A, Goh AMY, Sabates J, Clare L. Cognitive training for people with mild to moderate dementia. Cochrane Database Syst Rev. 2019;3(3):CD013069.
Orrell M, Yates L, Leung P, Kang S, Hoare Z, Whitaker C, et al. The impact of individual Cognitive Stimulation Therapy (iCST) on cognition, quality of life, caregiver health, and family relationships in dementia: A randomised controlled trial. PLoS Med. 2017;14(3):e1002269.
Park J, Kim SE, Kim EJ, Lee BI, Jeong JH, Na HR, et al. Effect of 12-week home-based cognitive training on cognitive function and brain metabolism in patients with amnestic mild cognitive impairment. Clin Interv Aging. 2019;14:1167-75.
Livingston G, Huntley J, Liu KY, Costafreda SG, Selbæk G, Alladi S, et al. Dementia prevention, intervention, and care: 2024 report of the Lancet standing Commission. Lancet. 2024;404(10452):572-628.
Tantanokit T, Bosittipichet T, Leesri T. The Study of Prevalence and Associated Factors of Dementia in the Elderly. Siriraj Med J. 2021;73(4):224-35.
Sukhatunga K, Phattarayuttawat S, Luchom M, Chantra J, Chaiyasit W, Bunnagulrote K. Depression and Dementia in Thai Elderly in Urban and Rural Communities. Siriraj Med J. 1999;51(4):232-43.
Miljanovic Damjanovic V, Obradovic Salcin L, Ostojic D, Ostojic L, Gilic B, Geets Kesic M, et al. Exploring Factors Associated with Physical Activity in the Elderly: A Cross-Sectional Study during the COVID-19 Pandemic. Behav Sci (Basel). 2024;14(1):62.
Roberts RO, Cha RH, Mielke MM, Geda YE, Boeve BF, Machulda MM, et al. Risk and protective factors for cognitive impairment in persons aged 85 years and older. Neurology. 2015;84(18):1854-61.
Wilson RS, Boyle PA, Yu L, Barnes LL, Schneider JA, Bennett DA. Life-span cognitive activity, neuropathologic burden, and cognitive aging. Neurology. 2013;81(4):314-21.
Akbaraly T, Portet F, Fustinoni S, Dartigues J, Artero S, Rouaud O, et al. Leisure activities and the risk of dementia in the elderly Results from the Three-City Study. Neurology. 2009;73:854-61.
Almeida OP, Yeap BB, Alfonso H, Hankey GJ, Flicker L, Norman PE. Older men who use computers have lower risk of dementia. PLoS One. 2012;7(8):e44239.
Fritsch T, Smyth KA, Debanne SM, Petot GJ, Friedland RP. Participation in novelty-seeking leisure activities and Alzheimer's disease. J Geriatr Psychiatry Neurol. 2005;18(3):134-41.
Lindstrom HA, Fritsch T, Petot G, Smyth KA, Chen CH, Debanne SM, et al. The relationships between television viewing in midlife and the development of Alzheimer's disease in a case-control study. Brain Cogn. 2005;58(2):157-65.
Wilson RS, Scherr PA, Schneider JA, Tang Y, Bennett DA. Relation of cognitive activity to risk of developing Alzheimer disease. Neurology. 2007;69(20):1911-20.
Sommerlad A, Sabia S, Livingston G, Kivimäki M, Lewis G, Singh-Manoux A. Leisure activity participation and risk of dementia: An 18-year follow-up of the Whitehall II Study. Neurology. 2020;95(20):e2803-e15.
Yates LA, Ziser S, Spector A, Orrell M. Cognitive leisure activities and future risk of cognitive impairment and dementia: systematic review and meta-analysis. Int Psychogeriatr. 2016;28(11):1791-806.
Tangwongchai S, Charernboon T, Phanasathit M, Akkayagorn L, Hemrungrojn S, Phanthumchinda K, et al. The validity of thai version of the montreal cognitive assessment (MoCA-T). Dement Neuropsychol. 2009;3(2):172.
Train the brain forum committee. Thai Mental State Examination (TMSE). Siriraj Hosp Gaz. 1993;45:359-74.
Sclan SG, Reisberg B. Functional assessment staging (FAST) in Alzheimer's disease: reliability, validity, and ordinality. Int Psychogeriatr. 1992;4 Suppl 1:55-69.
Reisberg B, Ferris SH, de Leon MJ, Crook T. Global Deterioration Scale (GDS). Psychopharmacol Bull. 1988;24(4):661-3.
Wongpakaran N, Wongpakaran T, Van Reekum R. The Use of GDS-15 in Detecting MDD: A Comparison Between Residents in a Thai Long-Term Care Home and Geriatric Outpatients. J Clin Med Res. 2013;5(2):101-11.
Han F, Luo C, Lv D, Tian L, Qu C. Risk Factors Affecting Cognitive Impairment of the Elderly Aged 65 and Over: A Cross-Sectional Study. Frontiers in Aging Neuroscience. 2022;14.
Sun L, Diao X, Gang X, Lv Y, Zhao X, Yang S, et al. Risk Factors for Cognitive Impairment in Patients with Type 2 Diabetes. J Diabetes Res. 2020;2020:4591938.
Myhre JW, Mehl MR, Glisky EL. Cognitive Benefits of Online Social Networking for Healthy Older Adults. J Gerontol B Psychol Sci Soc Sci. 2017;72(5):752-60.
Choi EY, Wisniewski KM, Zelinski EM. Information and Communication Technology Use in Older Adults: A Unidirectional or Bi-directional Association with Cognitive Function? Comput Human Behav. 2021;121:106813.
Guzman-Parra J, Barnestein-Fonseca P, Guerrero-Pertiñez G, Anderberg P, Jimenez-Fernandez L, Valero-Moreno E, et al. Attitudes and Use of Information and Communication Technologies in Older Adults With Mild Cognitive Impairment or Early Stages of Dementia and Their Caregivers: Cross-Sectional Study. J Med Internet Res. 2020;22(6):e17253.
Hosseini S, Chaurasia A, Oremus M. The Effect of Religion and Spirituality on Cognitive Function: A Systematic Review. Gerontologist. 2019;59(2):e76-e85.
Lin KP, Chou YC, Chen JH, Chen CD, Yang SY, Chen TF, et al. Religious affiliation and the risk of dementia in Taiwanese elderly. Arch Gerontol Geriatr. 2015;60(3):501-6.
Kaufman Y, Anaki D, Binns M, Freedman M. Cognitive decline in Alzheimer disease: Impact of spirituality, religiosity, and QOL. Neurology. 2007;68(18):1509-14.
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














