Effectiveness of Personalized Multifactorial Fall Risk Assessment and Intervention in Reducing Fall Rates Among Older Adults: A Retrospective Study
DOI:
https://doi.org/10.33192/smj.v77i1.271422Keywords:
Aged, Balance, Exercise therapy, Falls, Gait disorders, Rehabilitation, Risk factorsAbstract
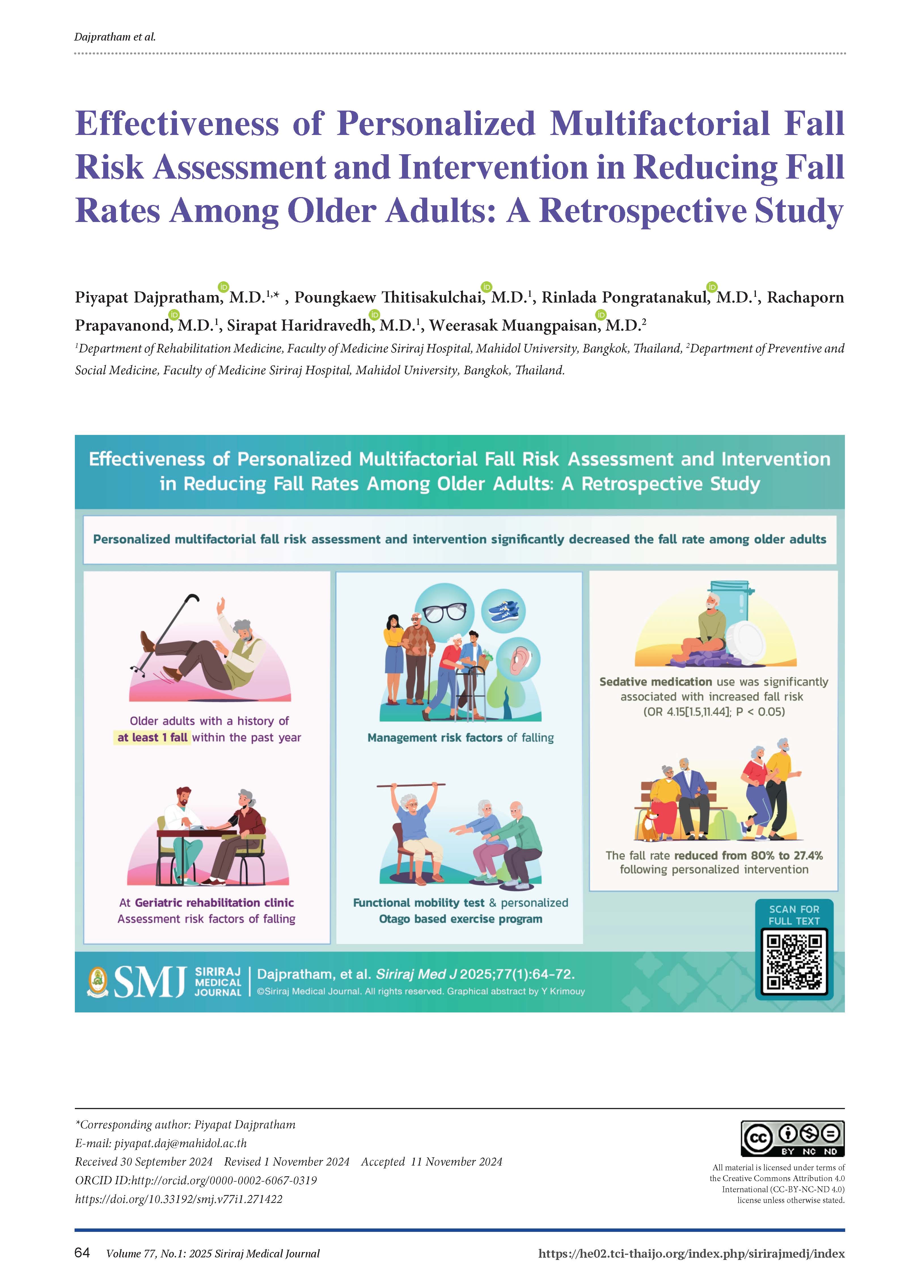
Objective: This study aimed to investigate the effectiveness of personalized multifactorial fall risk assessment and intervention in reducing the incidence of recurrent falls after one year.
Materials and Methods: This retrospective study reviewed medical records from the Geriatric Rehabilitation Clinic at Siriraj Hospital, including data from patients with a history of falls (fallers) or gait instability (non-fallers) between April 2016 and April 2021. Upon entering the clinic, older patients received personalized multifactorial fall risk assessment and intervention. Functional mobility was also evaluated using the Timed Up and Go (TUG) test, Functional Reach, and 30-second Chair Stand test. Fallers were followed for one year, and classified into recurrent fallers or zero-fallers based on whether they experienced at least one fall during the follow-up period.
Results: Of the 134 patients initially reviewed, 105 met the criteria for analysis. The cohort was predominantly female (65.5%) with an average age of 81.5 years (SD 6.8). Common risk factors included hypertension, back/leg pain, and cognitive impairment. After 12 months, 27.4% of fallers experienced recurrent falls. Sedative medication use was significantly associated with increased fall risk (OR 4.15[1.5,11.44]; P < 0.05). Other risk factors were not statistically significant. The fall rate reduced from 80% to 27.4% following personalized intervention.
Conclusion: Personalized multifactorial fall risk assessment and intervention significantly decreased the fall rate among older patients. Sedative medications were notably linked to increased fall risk, highlighting the need for careful medication management and targeted fall prevention strategies.gies.
References
Xing L, Bao Y, Wang B, Shi M, Wei Y, Huang X, et al. Falls caused by balance disorders in the elderly with multiple systems involved: pathogenic mechanisms and treatment strategies. Front Neurol. 2023;14(1):1128092.
Haddad YK, Bergen G, Florence CS. Estimating the economic burden related to older adult falls by state. J Public Health Manag Pract. 2019;25(2):E17-E24.
Chantharamani K, Kaewsarn P, Tipkanjanaraykha K. The development of a fall risk assessment form for elderly patients with visual impairment at the ophthalmic ward. J Royal Thai Army Nurses 2023;24(3):330-8.
American geriatrics society and british geriatrics society. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148-57.
Center for disease control and prevention. STEADI-older adult fall prevention: clinical resource [Internet]. Atlanta: U.S Department of Health and Human services; [cited 2024 Sep 1]. Available from: https://www.cdc.gov/steadi/hcp/clinical-resources/index.html.
Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;1(1):CD012424.
Cheng P, Tan L, Ning P, Li L, Gao Y, Wu Y, et al. Comparative effectiveness of published interventions for elderly fall prevention: a systematic review and network meta-analysis. Int J Environ Res Public Health. 2018;15(3):1-14.
Rimland JM, Abraha I, Dell'Aquila G, Cruz-Jentoft A, Soiza R, Gudmusson A, et al. Effectiveness of non-pharmacological interventions to prevent falls in older people: a systematic overview. The SENATOR Project ONTOP Series. PLoS One. 2016;11(8):e0161579.
Rehabilitation Institute of Chicago d/b/a Shirley Ryan AbilityLab. AbilityLab Home[Internet]. Shirley Ryan AbilityLab 2022 [cited 2024 Jul 27]. Available from: https://www.sralab.org/.
Graf C. The Lawton instrumental activities of daily living scale. Am J Nurs. 2008;108(4):52-62.
Gardner MM, Buchner DM, Robertson MC, Campbell AJ. Practical implementation of an exercise-based falls prevention programme. Age Ageing. 2001;30(1):77-83.
Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med. 1994;331(13):821-7.
SPSS Inc. Released 2009. PASW Statistics for Windows, Version 18.0. Chicago: SPSS Inc.
Rosenthai JA. Qualitative descriptors of strength of association and effect size. J Soc Serv Res 1996;21(4): 37–59.
Assantachai P, Praditsuwan R, Chatthanawaree W, Pisalsarakij D, Thamlikitkul V. Risk factors for falls in the Thai elderly in an urban community. J Med Assoc Thai. 2003;86(2):124-30.
Assantachai P, Watanapa W, Chiempittayanuwat S, Thipanunt P. Hypertension in the elderly: a community study. J Med Assoc Thai. 1998;81(4):243-9.
Lee SH, Yu S. Effectiveness of multifactorial interventions in preventing falls among older adults in the community: A systematic review and meta-analysis. Int J Nurs Stud. 2020;106(1):103564.
Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169(21):1952-60.
Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc. 1999;47(1):30-9.
Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: II. Cardiac and analgesic drugs. J Am Geriatr Soc. 1999;47(1):40-50.
de Vries M, Seppala LJ, Daams JG, van de Glind EMM, Masud T, van der Velde N. Fall-risk-increasing drugs: a systematic review and meta-analysis: I. cardiovascular drugs. J Am Med Dir Assoc. 2018;19(4):371.e1-.e9.
Seppala LJ, van de Glind EMM, Daams JG, Ploegmakers KJ, de Vries M, Wermelink A, et al. Fall-Risk-Increasing Drugs: a systematic review and meta-analysis: III. others. J Am Med Dir Assoc. 2018;19(4):372.e1-.e8.
Seppala LJ, Wermelink A, de Vries M, Ploegmakers KJ, van de Glind EMM, Daams JG, et al. Fall-Risk-Increasing Drugs: a systematic review and meta-analysis: II. psychotropics. J Am Med Dir Assoc. 2018;19(4):371.e11-.e17.
Xue L, Boudreau RM, Donohue JM, Zgibor JC, Marcum ZA, Costacou T, et al. Persistent polypharmacy and fall injury risk: the health, aging and body composition study. BMC Geriatr. 2021;21(1):710.
Wouters H, Van Campen JP, Kuitert MJ, Kikkert L, Hilmer SN, Taxis K, et al. Anticholinergic and sedative medications and dynamic gait parameters in older patients. Drugs Aging. 2021;38(12):1087-96.
Gnjidic D, Bell JS, Hilmer SN, Lönnroos E, Sulkava R, Hartikainen S. Drug Burden Index associated with function in community-dwelling older people in Finland: a cross-sectional study. Ann Med. 2012;44(5):458-67.
Herrero A, Velilla N, Renedo F. Deterioro cognitivo y riesgo de caída en el anciano [cognitive impairment and the risk of falling in the elderly]. Rev Esp Geriatr Gerontol. 2011;46(6):311-8.
Clemson L, Stark S, Pighills AC, Fairhall NJ, Lamb SE, Ali J, et al. Environmental interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2023;3(3):CD013258.
Yang Y, Wang K, Liu H, Qu J, Wang Y, Chen P, Zhang T, Luo J. The impact of Otago exercise programme on the prevention of falls in older adult: A systematic review. Front Public Health. 2022;10:953593.
Xu Q, Ou X, Li J. The risk of falls among the aging population: a systematic review and meta-analysis. Front Public Health. 2022;10:902599. DOI: 10.3389/fpubh.2022.902599.
Ha VT, Nguyen TN, Nguyen TX, Nguyen HTT, Nguyen TTH, Nguyen AT, et al. Prevalence and factors associated with falls among older outpatients. Int J Environ Res Public Health. 2021;18(8):4041.
Vongsirinavarat M, Kraiwong R. Falls among older adults with type 2 diabetes mellitus with peripheral neuropathy. Siriraj Med J. 2021;73(2):92-8.
Yang Y, Hu X, Zhang Q, Zou R. Diabetes mellitus and risk of falls in older adults: a systematic review and meta-analysis. Age Ageing. 2016;45(6):761-7.
Montero-Odasso MM, Kamkar N, Pieruccini-Faria F, Osman A, Sarquis-Adamson Y, Close J, et al. Evaluation of clinical practice guidelines on fall prevention and management for older adults: a systematic review. JAMA Netw Open. 2021;4(12):e2138911.
Dautzenberg L, Beglinger S, Tsokani S, Zevgiti S, Raijmann R, Rodondi N, et al. Interventions for preventing falls and fall-related fractures in community-dwelling older adults: a systematic review and network meta-analysis. J Am Geriatr Soc. 2021;69(10):2973-84.
Guirguis-Blake JM, Michael YL, Perdue LA, Coppola EL, Beil TL. Interventions to prevent falls in older adults: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2018;319(16):1705-16.
Yang Y, Wang K, Liu H, Qu J, Wang Y, Chen P, et al. The impact of Otago exercise programme on the prevention of falls in older adult: a systematic review. Front Public Health. 2022;10:953593.
Duckham RL, Masud T, Taylor R, Kendrick D, Carpenter H, Iliffe S, et al. Randomised controlled trial of the effectiveness of community group and home-based falls prevention exercise programmes on bone health in older people: the ProAct65+ bone study. Age Ageing. 2015;44(4):573-9.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














