Impact of Frailty on Healthcare Utilization in Older Patients Admitted to Medical Wards: A Study from a Large Medical School in a Middle-income Setting
DOI:
https://doi.org/10.33192/smj.v77i1.271497Keywords:
Frailty, Length of hospital stay, Health care cost, Mortality, Older patientsAbstract
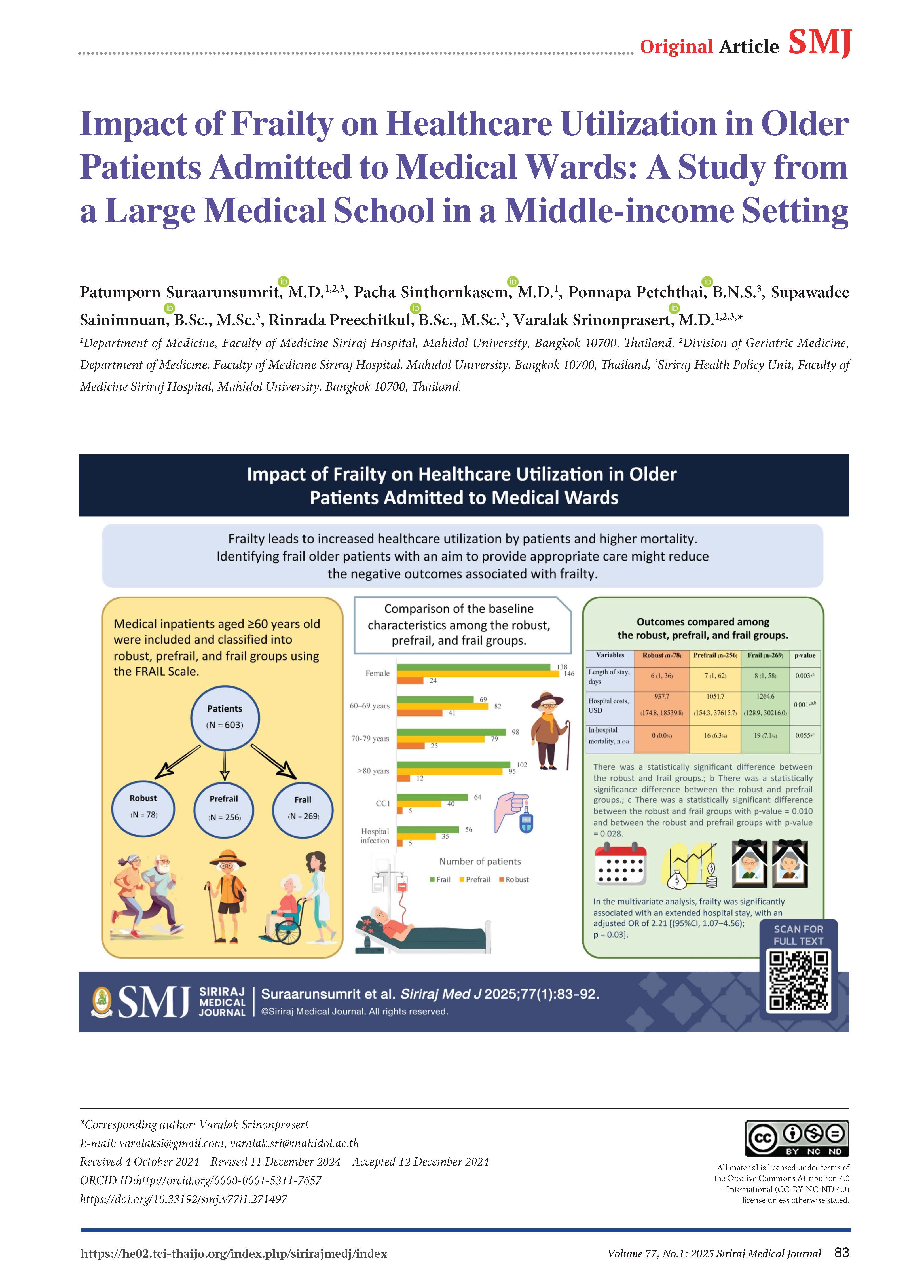
Objective: The study aimed to evaluate healthcare utilization and mortality in patients stratified by frailty status and explore the factors associated with a prolonged length of hospital stay (LOS).
Materials and Methods: This retrospective cohort study included medical inpatients aged ≥60 years old. They were classified into robust, prefrail, and frail groups using the FRAIL Scale. The primary outcome was LOS, while the secondary outcomes were hospital costs, in-hospital mortality, and factors associated with a prolonged LOS. Multivariate analysis was used to explore the factors that influenced the prolonged LOS, and the results were expressed using an adjusted odds ratio (AOR).
Results: Of the 603 enrolled participants, 269 (44.6%) were classified as frail, 256 (42.5%) as prefrail, and 78 (12.9%) as robust. The frail group had longer hospital stays than the robust group (8 days [1,58] vs. 6 days [1,36]; p=0.003). Healthcare costs in the frail and prefrail groups were higher than in the robust group (1264.6 USD [128.9, 30216.0], 1051.7 USD [154.3, 37615.7], and 937.7 USD [174.8, 18539.8], respectively; p=0.001). Frail and prefrail patients were also more likely to die in hospital than the robust ones (7.1% vs. 0.0%, p=0.010; 6.3% vs. 0.0%, p =0.028, respectively). The multivariate analysis also revealed that frailty was associated with a prolonged LOS [AOR of 2.21(95%CI, 1.07–4.56); p=0.031].
Conclusion: Frailty leads to increased healthcare utilization by patients and higher mortality. Identifying frail older patients with an aim to provide appropriate care might reduce the negative outcomes associated with frailty.
References
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752-62.
Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. The Lancet. 2019;394(10206):1376-86.
Gómez Jiménez E, Avendaño Céspedes A, Cortés Zamora EB, García Molina R, Abizanda P. [Frailty prevalence in hospitalized older adults. A systematic review.]. Revista espanola de salud publica. 2021;95.
Suraarunsumrit P, Pathonsmith C, Srinonprasert V, Sangarunakul N, Jiraphorncharas C, Siriussawakul A. Postoperative cognitive dysfunction in older surgical patients associated with increased healthcare utilization: a prospective study from an upper-middle-income country. BMC Geriatr. 2022;22(1):213.
Cunha AIL, Veronese N, de Melo Borges S, Ricci NA. Frailty as a predictor of adverse outcomes in hospitalized older adults: A systematic review and meta-analysis. Ageing Res Rev. 2019;56:100960.
Chang SF, Cheng CL, Lin HC. Frail Phenotype and Disability Prediction in Community-Dwelling Older People: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. The journal of nursing research : JNR. 2019;27(3):e28.
Srinonprasert V, Chalermsri C, Aekplakorn W. Frailty index to predict all-cause mortality in Thai community-dwelling older population: A result from a National Health Examination Survey cohort. Archives of gerontology and geriatrics. 2018;77:124-8.
Kojima G, Iliffe S, Walters K. Frailty index as a predictor of mortality: a systematic review and meta-analysis. Age Ageing. 2018;47(2):193-200.
Hajek A, Bock JO, Saum KU, Matschinger H, Brenner H, Holleczek B, et al. Frailty and healthcare costs-longitudinal results of a prospective cohort study. Age Ageing. 2018;47(2):233-41.
García-Nogueras I, Aranda-Reneo I, Peña-Longobardo LM, Oliva-Moreno J, Abizanda P. Use of Health Resources and Healthcare Costs associated with Frailty: The FRADEA Study. J Nutr Health Aging. 2017;21(2):207-14.
Bock J-O, König H-H, Brenner H, Haefeli WE, Quinzler R, Matschinger H, et al. Associations of frailty with health care costs – results of the ESTHER cohort study. BMC Health Services Research. 2016;16(1):128.
Comans TA, Peel NM, Hubbard RE, Mulligan AD, Gray LC, Scuffham PA. The increase in healthcare costs associated with frailty in older people discharged to a post-acute transition care program. Age and ageing. 2016;45(2):317-20.
Vermeiren S, Vella-Azzopardi R, Beckwée D, Habbig AK, Scafoglieri A, Jansen B, et al. Frailty and the Prediction of Negative Health Outcomes: A Meta-Analysis. J Am Med Dir Assoc. 2016;17(12):1163.e1-.e17.
Ara R, Monisha UK, Nova TJ, Chowdhury S, Nabi MH, Hawlader MDH. Potential nonpharmacological interventions to prevent frailty among elderly in low-and middle-income countries: A protocol for systematic review. Medicine. 2022;101(4).
Gray WK, Richardson J, McGuire J, Dewhurst F, Elder V, Weeks J, et al. Frailty Screening in Low- and Middle-Income Countries: A Systematic Review. J Am Geriatr Soc. 2016;64(4):806-23.
Foundation of Thai Gerontology Research and Development institute (TGRI). Situation of Thai Elderly 2020. In: Foundation of Thai Gerontology Research and Development Institute, editor. Bangkok2021.
TDRI study report. Estimate public health expenditure in the next 15 years. 2562. Available from: htttps://tdri.or.th/2019/12/public-healthcare-evaluation/.
Sriwong W, Mahavisessin W, Srinonprasert V, Siriussawakul A, Aekplakorn W, Limpawattana P, et al. Validity and reliability of the Thai version of the simple frailty questionnaire (T-FRAIL) with modifications to improve its diagnostic properties in the preoperative setting. BMC geriatrics. 2022;22(1):161.
Subramaniam A, Tiruvoipati R, Green C, Srikanth V, Soh L, Yeoh AC, et al. Frailty status, timely goals of care documentation and clinical outcomes in older hospitalised medical patients. Intern Med J. 2021;51(12):2078-86.
Toh HJ, Lim ZY, Yap P, Tang T. Factors associated with prolonged length of stay in older patients. Singapore medical journal. 2017;58(3):134-8.
Bo M, Fonte G, Pivaro F, Bonetto M, Comi C, Giorgis V, et al. Prevalence of and factors associated with prolonged length of stay in older hospitalized medical patients. Geriatr Gerontol Int. 2016;16(3):314-21.
Marfil-Garza BA, Belaunzarán-Zamudio PF, Gulias-Herrero A, Zuñiga AC, Caro-Vega Y, Kershenobich-Stalnikowitz D, et al. Risk factors associated with prolonged hospital length-of-stay: 18-year retrospective study of hospitalizations in a tertiary healthcare center in Mexico. PLoS One. 2018;13(11):e0207203.
Liu T, Xuan H, Wang L, Li X, Lu Z, Tian Z, et al. The association between serum albumin and long length of stay of patients with acute heart failure: A retrospective study based on the MIMIC-IV database. PLoS One. 2023;18(2):e0282289.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146-56.
Kojima G. Frailty Defined by FRAIL Scale as a Predictor of Mortality: A Systematic Review and Meta-analysis. J Am Med Dir Assoc. 2018;19(6):480-3.
Hao Q, Zhou L, Dong B, Yang M, Dong B, Weil Y. The role of frailty in predicting mortality and readmission in older adults in acute care wards: a prospective study. Sci Rep. 2019;9(1):1207.
Ambagtsheer RC, Moussa RK. Association of frailty with health service utilisation and health care expenditure in sub-Saharan Africa: evidence from Côte d'Ivoire. BMC Geriatr. 2021;21(1):446.
Lujic S, Randall DA, Simpson JM, Falster MO, Jorm LR. Interaction effects of multimorbidity and frailty on adverse health outcomes in elderly hospitalised patients. Sci Rep. 2022;12(1):14139.
Xia F, Zhang J, Meng S, Qiu H, Guo F. Association of Frailty With the Risk of Mortality and Resource Utilization in Elderly Patients in Intensive Care Units: A Meta-Analysis. Front Med (Lausanne). 2021;8:637446.
Tal S. Length of hospital stay among oldest-old patients in acute geriatric ward. Archives of Gerontology and Geriatrics. 2021;94:104352.
Ekdahl AW, Sjöstrand F, Ehrenberg A, Oredsson S, Stavenow L, Wisten A, et al. Frailty and comprehensive geriatric assessment organized as CGA-ward or CGA-consult for older adult patients in the acute care setting: A systematic review and meta-analysis. European Geriatric Medicine. 2015;6(6):523-40.
Ellis G, Gardner M, Tsiachristas A, Langhorne P, Burke O, Harwood RH, et al. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev. 2017;9:CD006211.
Chen Z, Ding Z, Chen C, Sun Y, Jiang Y, Liu F, et al. Effectiveness of comprehensive geriatric assessment intervention on quality of life, caregiver burden and length of hospital stay: a systematic review and meta-analysis of randomised controlled trials. BMC Geriatr. 2021;21(1):377.
Jirakulsawat A, Noocharoen N, Somnuke P. Prehabilitation in Clinical Practice: A Review of Concepts and Implementation in Enhancing Post-operative Outcomes. Siriraj Med J. 2024;76(9):646-54.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














