Clinical Effectiveness Evaluation and Cost-effectiveness Analysis of Comprehensive Geriatric Assessment and Multidisciplinary Team for Ambulatory Older Patients: A Cohort Study
DOI:
https://doi.org/10.33192/smj.v77i1.271623Keywords:
clinical effectiveness evaluation, cost-effectiveness, incremental cost-effectiveness, comprehensive geriatric assessment, multidisciplinary team, geriatric clinicAbstract
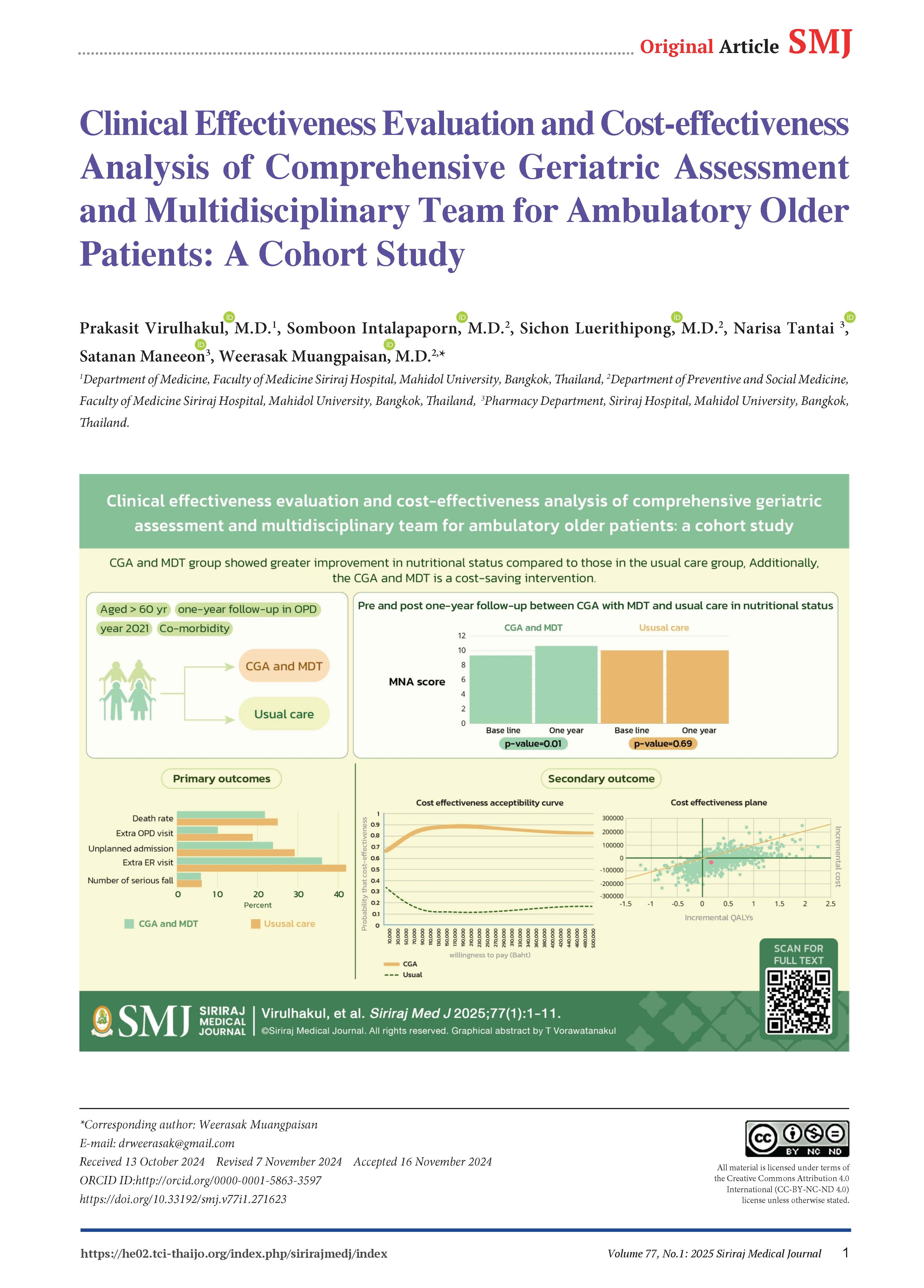
Objective: The comprehensive geriatric assessment (CGA) and multidisciplinary team (MDT) services are essential components of clinics that promote holistic care for older patients. However, their clinical and cost-effectiveness have not been fully established.
Materials and Methods: This study was a 1-year cohort, two-arm observational study conducted in ambulatory older patients at the Geriatric and Internal Medicine OPD. The primary endpoint was clinical effectiveness: activity of daily living (ADL), Thai mental status examination (TMSE), Mini-nutritional assessment (MNA), extra-visit, hospitalization, length of stay, fall rate, and death rate. The secondary endpoint was a cost-utility analysis using a decision-tree and Markov model. Outcomes included the incremental cost-effectiveness ratio (ICER), and quality of life, assessed by the European Quality of Life Five Dimensions Five Levels (EQ-5D-5L). Sensitivity analysis was conducted through probabilistic methods.
Results: Older adults who received the CGA and MDT service in the geriatric OPD showed improved nutritional status, with the MNA-SF score increasing from 9.3 (± 3.3) to 10.9 (± 2.9) (p=0.01). There were no significant differences between groups in terms of extra-visits, hospitalizations, length of stay, fall rate, or death rate. After one year, the ICER for the CGA and MDT group was US$-3,073 per quality-adjusted life year (QALY) gained to usual care, indicating cost savings at a threshold of $4, 564.9 US dollar per QALY gained.
Conclusion: The CGA and MDT service in a geriatric clinic is clinically effective compared to usual care over a one-year follow-up, as demonstrated by the improvement in nutritional status. Additionally, the CGA and MDT is a cost-saving intervention.
References
Carl H. Fact sheet: World population trends 2012. Population reference bureau. 2012.
Chewasopit W. AGING SOCIETY: THE CHANGED MARKETING FACTOR. Journal of MCU Nakhondhat. 2019;6:38-54.
Rakbumned C. Expenditure budget burden,The Secretariat of The House of Representatives. 2017.
Ellis G, Whitehead MA, Robinson D, O’Neill D, Langhorne P. Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ 2011;343:d6553.
Lundqvist M, Alwin J, Henriksson M, Husberg M, Carlsson P, Ekdahl AW. Cost-effectiveness of comprehensive geriatric assessment at an ambulatory geriatric unit based on the AGe-FIT trial. BMC geriatrics. 2018;18(1):32.
Boorsma M, Frijters DH, Knol DL, Ribbe ME, Nijpels G, van Hout HPJC. Effects of multidisciplinary integrated care on quality of care in residential care facilities for elderly people: a cluster randomized trial. CMAJ. 2011;183(11):E724-E32.
Amelie M. Outpatient comprehensive geriatric assessment: effects on frailty and mortality in old people with multimorbidity and high health care utilization. Aging Clin Exp Res. 2019;31(4):519-25.
Poudel A, Peel NM, Mitchell CA, Gray LC, Nissen LM, Hubbard RE. Geriatrician interventions on medication prescribing for frail older people in residential aged care facilities. J Clinical interventions in aging. 2015;10:1043.
Ellis G, Langhorne P. Comprehensive geriatric assessment for older hospital patients. BMJ. 2005;71(1):45-59.
Ekdahl AW, Wirehn A-B, Alwin J, Jaarsma T, Unosson M, Husberg M, et al. Costs and effects of an ambulatory geriatric unit (the AGe-FIT study): a randomized controlled trial. J Am Med Dir Assoc. 2015;16(6):497-503.
Jeppesen SS, Matzen LE, Brink C, Bliucukiene R, Kasch S, Schytte T, et al. Impact of comprehensive geriatric assessment on quality of life, overall survival, and unplanned admission in patients with non-small cell lung cancer treated with stereotactic body radiotherapy. J Geriatr Oncol. 2018;9(6):575-82.
Morley JE, Arai H, Cao L, Dong B, Merchant RA, Vellas B, et al. Integrated care: enhancing the role of the primary health care professional in preventing functional decline: a systematic review. J Am Med Dir Assoc. 2017;18(6):489-94.
Ellis G, Whitehead MA, Robinson D, O’Neill D, Langhorne PJB. Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ. 2011;343:d6553.
Soejono CH. The impact of'comprehensive geriatric assessment (CGA)'implementation on the effectiveness and cost (CEA) of healthcare in an acute geriatric ward. Acta Med Indones. 2008;40(1):3-10.
Sumonthip P, Boonkerd J, Phrayai N, Permkrietkajorn R. Program evaluation Comprehensive geriatric assessment clinic Satisfaction Older patients. Ramathibodi Nursing Journal. 2013;16(3):443-55.
Stineman MG, Xie D, Pan Q, Kurichi JE, Zhang Z, Saliba D, et al. All‐cause 1‐, 5‐, and 10‐year mortality in elderly people according to activities of daily living stage. J Am Geriatr Soc. 2012;60(3):485-92.
Stineman MG. All‐cause 1‐, 5‐, and 10‐year mortality in elderly people according to activities of daily living stage. J Am Geriatr Soc. 2012;60(3):485-92.
Podgorelec V. Decision trees: an overview and their use in medicine. J Med Syst. 2002;26(5):445-63.
Komorowski M. Markov models and cost effectiveness analysis: applications in medical research. J Secondary analysis of electronic health records. 2016:351-67.
Pattanaphesaj J. Health-related quality of life measure (EQ-5D-5L): measurement property testing and its preference-based score in Thai population: Mahidol University Salaya, Thailand; 2014.
PATTANAPRATEEP DO. CLINICAL ECONOMICS. 2019.
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes: Oxford university press; 2015.
Barreto H, Howland F. Introductory econometrics: using Monte Carlo simulation with Microsoft excel: Cambridge University Press; 2006.
Nimdet K, Ngorsuraches S. Willingness-To-Pay For Life-Saving Treatments In Thailand: A Discrete Choice Experiment. Value Health. 2017;20(9):A682.
Tanajewski L, Franklin M, Gkountouras G, Berdunov V, Edmans J, Conroy S, et al. Cost-effectiveness of a specialist geriatric medical intervention for frail older people discharged from acute medical units: economic evaluation in a two-centre randomised controlled trial (AMIGOS). PLoS One. 2015;10(5):e0121340.
Hay JW, Gong CL, Jiao X, Zawadzki NK, Zawadzki RS, Pickard AS, et al. A US population health survey on the impact of COVID-19 using the EQ-5D-5L. 2021;36(5):1292-301.
Gray RS, Hahn L, Thapsuwan S, Thongcharoenchupong N. Strength and stress: Positive and negative impacts on caregivers for older adults in T hailand. Australas J Ageing. 2016;35(2):E7-E12.
Bergmann M, Wagner M. The Impact of COVID-19 on Informal Caregiving and Care Receiving Across Europe During the First Phase of the Pandemic. 2021;9.
Lim SL, Woo KL, Lim E, Ng F, Chan MY, Gandhi M. Impact of COVID-19 on health-related quality of life in patients with cardiovascular disease: a multi-ethnic Asian study. Health Qual Life Outcomes. 2020;18(1):1-7.
Wei Y-J, Hsieh C-F, Huang Y-T, Huang M-S, Fang T-J. The influence of integrated geriatric outpatient clinics on the health care utilization of older people. J BMC geriatrics. 2020;20(1):1-12.
Ulmer MJ. Chapter III. The Theory of the Cost of Living Index. The Economic Theory of Cost of Living Index Numbers: Columbia University Press; 1949. p. 26-43.
Ranhoff AH. Out-patient geriatric assessment by a hospital-based general practitioner: Results and financial implications. Norsk Epidemiologic. 1998;8(2).
Salagre S, Kundawar A, Srivastava P, Saha T, Mantri A, Jain S, et al. Comprehensive Geriatric Assessment (CGA) Screening of Geriatric Patients in a Tertiary Care Hospital: a Cross-sectional Study in India. J Assoc Physicians India. 2022;70(1):11-2.
Hosoi T, Yamana H, Tamiya H, Matsui H, Fushimi K, Akishita M, et al. Association between comprehensive geriatric assessment and short-term outcomes among older adult patients with stroke: A nationwide retrospective cohort study using propensity score and instrumental variable methods. E Clinical Medicine. 2020;23:100411.
Dahlqvist J, Ekdahl A, Friedrichsen M. Does comprehensive geriatric assessment (CGA) in an outpatient care setting affect the causes of death and the quality of palliative care? A subanalysis of the age-FIT study. Eur Geriatr Med. 2019;10(3):455-62.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














