Reliability and Validity of the Thai Version of the PAINAD Scale: An Extended Application of Pain Assessment in the Moderately Severe Stage of Dementia
DOI:
https://doi.org/10.33192/smj.v77i1.271644Keywords:
Pain, Dementia, Reproducibility of ResultsAbstract
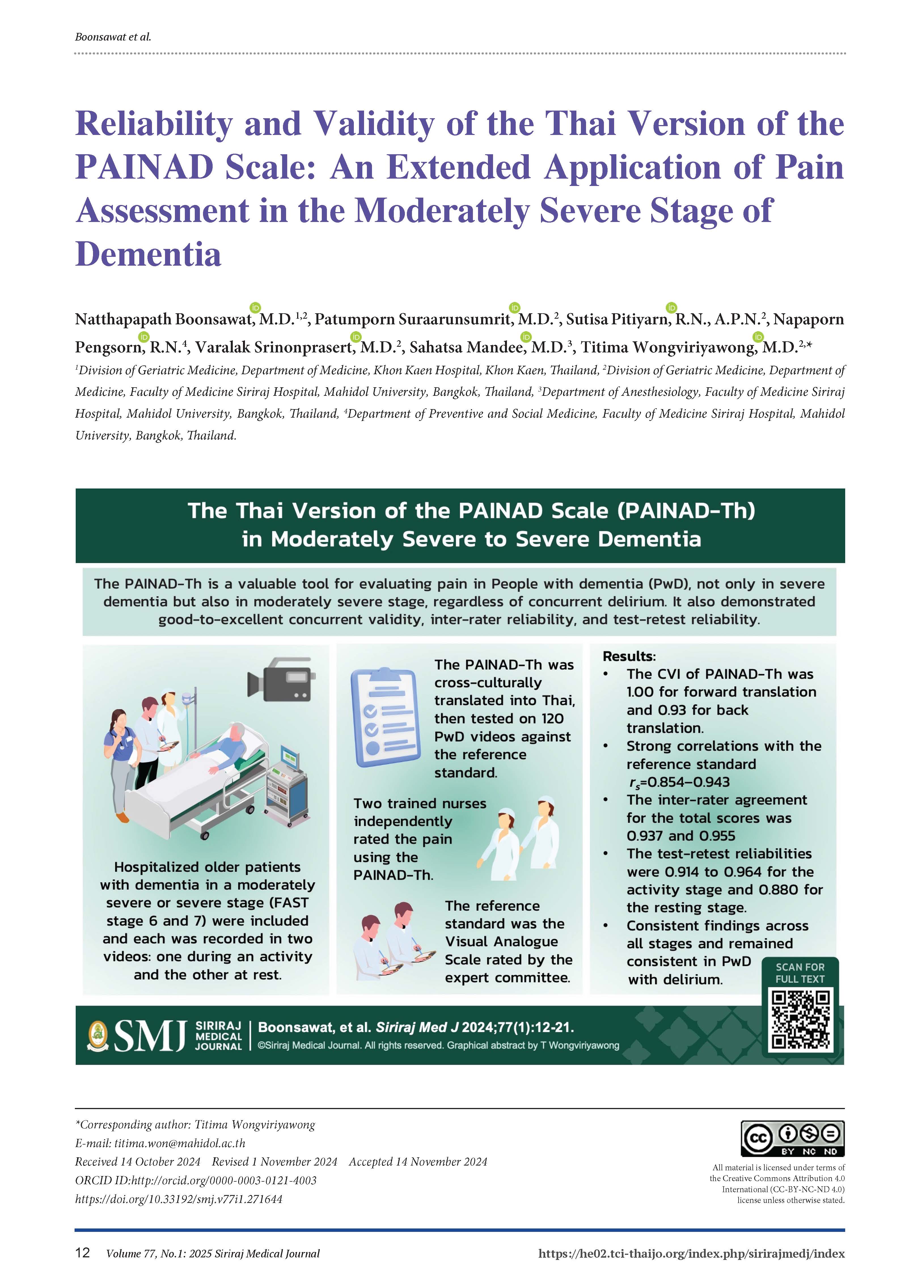
Objective: To evaluate the reliability and validity of the Thai version of the PAINAD (PAINAD-Th) scale for assessing pain in people with dementia (PwD).
Materials and methods: A cross-cultural translation of the PAINAD scale involving forward and back-translation to and from Thai was conducted, and then the content validity index (CVI) of semantic equivalence was evaluated. The PAINAD-Th was tested on 120 videos of PwD. Each participant was recorded in two videos: one during an activity and the other at rest. Subsequently, two trained nurses independently observed the videos and rated the PAINAD-Th to assess inter-rater reliability. The rating process was repeated in one week to investigate the test-retest reliability. The concurrent validity was assessed against the Visual Analogue Scale rated by the expert committee.
Results: The CVI of PAINAD-Th was 1.00 for forward translation and 0.93 for back translation. The PAINAD-Th showed strong correlations with the reference standard (rs=0.854–0.943, p-value <0.001). The inter-rater agreement for the total scores was 0.937 and 0.955, and the test-retest reliabilities were 0.914 to 0.964 for the activity stage and 0.880 for the resting stage, respectively. The concurrent validity index did not vary significantly across different stages of dementia; the findings remained consistent in the delirium subgroup analysis.
Conclusions: The PAINAD-Th is a valuable tool for evaluating pain in PwD, not only in severe dementia but also in moderately severe stage, regardless of concurrent delirium. It also demonstrated good-to-excellent concurrent validity, inter-rater reliability, and test-retest reliability.
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders : DSM-5. Arlington, VA: American Psychiatric Association; 2013.
Taemeeyapradit U, Udomittipong D, Tepparak N. Characteristics of behavioral and psychological symptoms of dementia, severity and levels of distress on caregivers. J Med Assoc Thai. 2014;97(4):423-30.
Reisberg B, Ferris SH, de Leon MJ, Crook T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982;139(9):1136-9.
Lin PC, Li CH, Chou PL, Chen YM, Lin LC. Prevalence of pain-related diagnoses in patients with dementia: a nationwide study. J Pain Res. 2018;11:1589-98.
Tan EC, Jokanovic N, Koponen MP, Thomas D, Hilmer SN, Bell JS. Prevalence of Analgesic Use and Pain in People with and without Dementia or Cognitive Impairment in Aged Care Facilities: A Systematic Review and Meta-Analysis. Curr Clin Pharmacol. 2015;10(3):194-203.
Corbett A, Husebo BS, Achterberg WP, Aarsland D, Erdal A, Flo E. The importance of pain management in older people with dementia. British Medical Bulletin. 2014;111(1):139-48.
Miu DKY, Chan KC. Under-detection of pain in elderly nursing home residents with moderate to severe dementia. Journal of Clinical Gerontology and Geriatrics. 2014;5(1):23-7.
American Geriatric Society Panel on the Pharmacological Management of Persistent Pain in Older Persons. The management of persistent pain in older persons. J Am Geriatr Soc. 2002;50(6 Suppl):S205-24.
Schofield P. The Assessment of Pain in Older People: UK National Guidelines. Age Ageing. 2018;47(suppl_1):i1-i22.
Collett B, O'Mahoney S, Schofield P, Closs SJ, Potter J, Guideline Development G. The assessment of pain in older people. Clin Med (Lond). 2007;7(5):496-500.
van Dalen-Kok AH, Pieper MJ, de Waal MW, Lukas A, Husebo BS, Achterberg WP. Association between pain, neuropsychiatric symptoms, and physical function in dementia: a systematic review and meta-analysis. BMC Geriatr. 2015;15:49.
Sampson EL, White N, Lord K, Leurent B, Vickerstaff V, Scott S, et al. Pain, agitation, and behavioural problems in people with dementia admitted to general hospital wards: a longitudinal cohort study. Pain. 2015;156(4):675-83.
Warden V, Hurley AC, Volicer L. Development and psychometric evaluation of the Pain Assessment in Advanced Dementia (PAINAD) scale. J Am Med Dir Assoc. 2003;4(1):9-15.
DeWaters T, Faut-Callahan M, McCann JJ, Paice JA, Fogg L, Hollinger-Smith L, et al. Comparison of self-reported pain and the PAINAD scale in hospitalized cognitively impaired and intact older adults after hip fracture surgery. Orthop Nurs. 2008;27(1):21-8.
Jordan A, Hughes J, Pakresi M, Hepburn S, O'Brien JT. The utility of PAINAD in assessing pain in a UK population with severe dementia. Int J Geriatr Psychiatry. 2011;26(2):118-26.
Costardi D, Rozzini L, Costanzi C, Ghianda D, Franzoni S, Padovani A, et al. The Italian version of the pain assessment in advanced dementia (PAINAD) scale. Arch Gerontol Geriatr. 2007;44(2):175-80.
Lukas A, Hagg-Grun U, Mayer B, Fischer T, Schuler M. Pain assessment in advanced dementia. Validity of the German PAINAD-a prospective double-blind randomised placebo-controlled trial. Pain. 2019;160(3):742-53.
Buyukturan O, Naharci MI, Buyukturan B, Kirdi N, Yetis A. The Turkish Version of Pain Assessment in Advanced Dementia (PAINAD) Scale. Noro Psikiyatr Ars. 2018;55(3):271-5.
Pinto MC, Minson FP, Lopes AC, Laselva CR. Cultural adaptation and reproducibility validation of the Brazilian Portuguese version of the Pain Assessment in Advanced Dementia (PAINAD-Brazil) scale in non-verbal adult patients. Einstein (Sao Paulo). 2015;13(1):14-9.
Lin PC, Lin LC, Shyu YI, Hua MS. Chinese version of the Pain Assessment in Advanced Dementia Scale: initial psychometric evaluation. J Adv Nurs. 2010;66(10):2360-8.
Zwakhalen SM, Hamers JP, Berger MP. The psychometric quality and clinical usefulness of three pain assessment tools for elderly people with dementia. Pain. 2006;126(1-3):210-20.
Kwon SH, Cho YS, Kim H. Reliability and Feasibility of the Pain Assessment in Advanced Dementia Scale-Korean Version (PAINAD-K). Pain Manag Nurs. 2021;22(5):660-7.
Department of Older Persons. Situation of The Thai Older Persons 2022. Bangkok, Thailand: Amarin Corporations Public Company Limited; 2023. Available from: https://thaitgri.org/?p=40218.
Iamaroon A, Wongviriyawong T, Sura-Arunsumrit P, Wiwatnodom N, Rewuri N, Chaiwat O. Incidence of and risk factors for postoperative delirium in older adult patients undergoing noncardiac surgery: a prospective study. BMC Geriatr. 2020;20(1):40.
Srinonprasert V, Pakdeewongse S, Assanasen J, Eiamjinnasuwat W, Sirisuwat A, Limmathuroskul D, et al. Risk factors for developing delirium in older patients admitted to general medical wards. J Med Assoc Thai. 2011;94 Suppl 1:S99-104.
Srinil T, Lao-amornphunkul S, Narksut A, Thikom N, Pansangar C, Thanakiattiwibun C, et al. Incidences, Characteristics, Management and Outcomes of Different Subtypes of Postoperative Delirium in Elderly Patients Admitted to the Surgical Intensive Care Unit: A Secondary Analysis of a Prospective Cohort Study. Siriraj Medical Journal. 2024;76(7):406-14.
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000;25(24):3186-91.
Tsang S, Royse CF, Terkawi AS. Guidelines for developing, translating, and validating a questionnaire in perioperative and pain medicine. Saudi J Anaesth. 2017;11(Suppl 1):S80-S9.
Yusoff MSB. ABC of content validation and content validity index calculation. Education in Medicine Journal. 2019;11(2):49-54.
Senanarong V, Poungvarin N, Sukhatunga K, Prayoonwiwat N, Chaisewikul R, Petchurai R, et al. Cognitive status in the community dwelling Thai elderly. J Med Assoc Thai. 2001;84(3):408-16.
Siri S, Okanurak K, Chansirikanjana S, Kitayaporn D, Jorm AF. Modified Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) as a screening test for dementia for Thai elderly. Southeast Asian J Trop Med Public Health. 2006;37(3):587-94.
Muangpaisan W, Assantachai P, Sitthichai K, Richardson K, Brayne C. The Distribution of Thai Mental State Examination Scores among Non-Demented Elderly in Suburban Bangkok Metropolitan and Associated Factors. J Med Assoc Thai. 2015;98(9):916-24.
Tangwongchai S, Phanasathit M, Charernboon T, Akkayagorn L, Hemrungrojn S, Phanthumchinda K, et al. The validity of thai version of the montreal cognitive assessment (MoCA-T). Dement Neuropsychol. 2009;3(2):172.
Sclan SG, Reisberg B. Functional assessment staging (FAST) in Alzheimer's disease: reliability, validity, and ordinality. International psychogeriatrics. 1992;4(3):55-69.
Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369(9):840-51.
Mahoney FI, Barthel DW. Functional Evaluation: The Barthel Index. Md State Med J. 1965;14:61-5.
Scherder EJ, Bouma A. Visual analogue scales for pain assessment in Alzheimer's disease. Gerontology. 2000;46(1):47-53.
Schober P, Boer C, Schwarte LA. Correlation Coefficients: Appropriate Use and Interpretation. Anesth Analg. 2018;126(5):1763-8.
Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med. 2016;15(2):155-63.
Bobak CA, Barr PJ, O'Malley AJ. Estimation of an inter-rater intra-class correlation coefficient that overcomes common assumption violations in the assessment of health measurement scales. BMC Med Res Methodol. 2018;18(1):93.
Manz BD, Mosier R, Nusser-Gerlach MA, Bergstrom N, Agrawal S. Pain assessment in the cognitively impaired and unimpaired elderly. Pain Manag Nurs. 2000;1(4):106-15.
Pautex S, Michon A, Guedira M, Emond H, Le Lous P, Samaras D, et al. Pain in severe dementia: self-assessment or observational scales? J Am Geriatr Soc. 2006;54(7):1040-5.
Achterberg W, Lautenbacher S, Husebo B, Erdal A, Herr K. Pain in dementia. Pain Rep. 2020;5(1):e803.
Wrzesien A, Andrzejewski K, Jampolska M, Kaczynska K. Respiratory Dysfunction in Alzheimer's Disease-Consequence or Underlying Cause? Applying Animal Models to the Study of Respiratory Malfunctions. Int J Mol Sci. 2024;25(4).
Hibi S, Yamaguchi Y, Umeda-Kameyama Y, Iijima K, Takahashi M, Momose T, et al. Respiratory dysrhythmia in dementia with Lewy bodies: a cross-sectional study. BMJ Open. 2013;3(9):e002870.
Cherniack NS, Longobardo G, Evangelista CJ. Causes of cheyne-stokes respiration. Neurocritical Care. 2005;3(3):271-9.
White N, Bazo-Alvarez JC, Koopmans M, West E, Sampson EL. Understanding the association between pain and delirium in older hospital inpatients: systematic review and meta-analysis. Age Ageing. 2024;53(4).
Cerejeira J, Lagarto L, Mukaetova-Ladinska EB. Behavioral and psychological symptoms of dementia. Front Neurol. 2012;3:73.
Phannarus H, Muangpaisan W, Siritipakorn P, Pianchob S, Supapueng O. Development of a Thai tool for assessing behavioral and psychological symptoms of dementia: A confirmatory factor analysis. Brain Behav. 2020;10(11):e01816.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














