Validation of Self-application-based Malnutrition and Limited Mobility Screening Tools Compared with Standard Diagnostic Tools in Older Adults
DOI:
https://doi.org/10.33192/smj.v77i1.271719Keywords:
Screening, Application, Older adults, Malnutrition, Locomotor capacity, Intrinsic capacity, Limited mobility, WHO-ICOPEAbstract
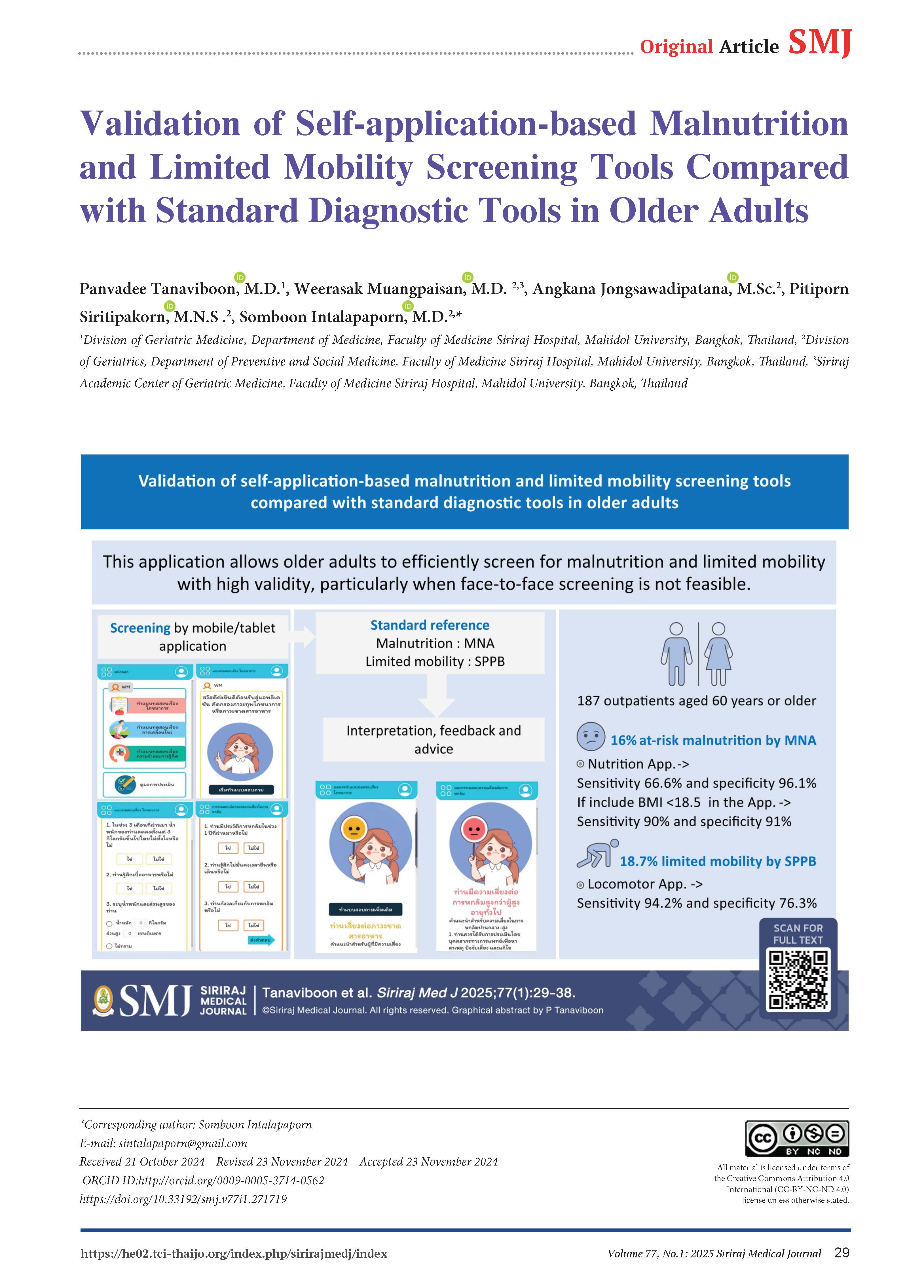
Objective: To validate application screening tools against face-to-face standard tools (the Mini Nutritional Assessment (MNA) and Short Physical Performance Battery test (SPPB)) in older adults.
Materials and Methods: A mobile or tablet application was developed based on user interfaces and experiences. Outpatients aged 60 years and over were tested with this tool. We used 2 questions from the WHO-ICOPE algorithm and 3 questions from the STEADI algorithm to screen for at-risk malnutrition and limited mobility, respectively. The MNA and SPPB were used to detect malnutrition and limited mobility, respectively, to test their validity.
Results: The study involved 187 participants, 16% of whom were diagnosed with at-risk malnutrition by the MNA and 18.7% of whom had limited mobility according to the SPPB. The sensitivity and specificity of the malnutrition application tool were 66.6% and 96.1%, respectively. When BMI < 18.5 was combined in the application, the sensitivity and specificity were 90% and 91%, respectively. For limited mobility, the sensitivity and specificity of the application were 94.2% and 76.3%, respectively. The majority of participants rated the application for easy understanding as «excellent» (65%) and rated their confidence in their ability to use the application by themselves as “excellent” (70%).
Conclusion: The application is an age-friendly, time-saving tool that can be used when face-to-face screening is vdifficult with good validity.
References
Cesari M, Keeffe J, Dent E, Kondo N, Laiteerapong A, Izquierdo M, et al. Integrated care for older people ( ICOPE):: Handbook: guidance for person-centred assessment and pathways in primary care. 2019.(Cesari, Keeffe et al. 2019)
Malnutrition among Older People in the Community [Internet]. bapen.org.uk. Available from: https://www.bapen.org.uk/pdfs/malnut_in_the_community.pdf
Chalermsri C, Assantachai P, Pramyothin P, Pengsorn N, Muangpaisan W. Prevalence of and factors associated with undernutrition in a geriatric outpatient setting: Results from a multidimensional nutritional assessment. Siriraj Med J. 2018;70(5):413-8.
Serón-Arbeloa C, Labarta-Monzón L, Puzo-Foncillas J, Mallor-Bonet T, Lafita-López A, Bueno-Vidales N, et al. Malnutrition screening and assessment. Nutrients. 2022;14(12):2392.
Reber E, Gomes F, Vasiloglou MF, Schuetz P, Stanga Z. Nutritional risk screening and assessment. J Clin Med. 2019;8(7):1065.
Power L, Mullally D, Gibney ER, Clarke M, Visser M, Volkert D, et al. A review of the validity of malnutrition screening tools used in older adults in community and healthcare settings - A MaNuEL study. Clin Nutr ESPEN. 2018;24:1-13.
Ackermans LLGC, Rabou J, Basrai M, Schweinlin A, Bischoff SC, Cussenot O, et al. Screening, diagnosis and monitoring of sarcopenia: When to use which tool? Clin Nutr ESPEN. 2022;48:36-44.
Isautier JM, Bosnić M, Yeung SS, Trappenburg MC, Meskers CG, Whittaker AC, et al. Validity of nutritional screening tools for community-dwelling older adults: a systematic review and meta-analysis. J Am Med Dir Assoc. 2019;20(10):1351.e13-1351.e25.
Cederholm T, Jensen G, Correia M, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition–a consensus report from the global clinical nutrition community. J Cachexia Sarcopenia Muscle. 2019;10(1):207-17.
Guigoz Y, Vellas B. Nutritional assessment in older adults: MNA® 25 years of a screening tool & a reference standard for care and research; what next? J Nutr Health Aging. 2021;25(4):528-83.
Soubra R, Chkeir A, Novella J-L. A systematic review of thirty‐one assessment tests to evaluate mobility in older adults. Biomed Res Int. 2019;2019:1354362.
Webber SC, Porter MM, Menec VH. Mobility in older adults: a comprehensive framework. Gerontologist. 2010;50(4):443-50.
Kaewkan K. Assessment of Physical Performance in elderly with Short Physical Performance Battery Test. J Med Health Sci. 2019;26(2):96-111.
Lamb SE, Keene DJ. Measuring physical capacity and performance in older people. Best Pract Res Clin Rheumatol. 2017;31(2):243-54.
Volkert D, Beck AM, Cederholm T, Cruz-Jentoft A, Hooper L, Kiesswetter E, et al. ESPEN practical guideline: Clinical nutrition and hydration in geriatrics. Clin Nutr. 2022;41(4):958-89.
Lindner-Rabl S, Wagner V, Matijevic A, Herzog C, Lampl C, Traub J, et al. Clinical interventions to improve nutritional care in older adults and patients in primary healthcare–a scoping review of current practices of health care practitioners. Clin Interv Aging. 2022;17:1-13.
Phu S, Kirk B, Bani Hassan E, Vogrin S, Zanker J, Bernardo S, et al. The diagnostic value of the Short Physical Performance Battery for sarcopenia. BMC Geriatr. 2020;20(1):242.
Beaudart C, Rolland Y, Cruz-Jentoft AJ, Bauer JM, Sieber C, Cooper C, et al. Assessment of muscle function and physical performance in daily clinical practice: a position paper endorsed by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Calcif Tissue Int. 2019;105(1):1-14.
What is the MNA®? [Internet]. Mna-elderly.com. Available from: http://www.mna-elderly.com
Short physical performance battery (sppb) guide [Internet]. sppbguide.com. Available from: https://sppbguide.com
Timed Up & go(TUG) [Internet]. Cdc.gov. Available from: https://www.cdc.gov/steadi/media/pdfs/STEADI-Assessment-TUG-508.pdf
Miranda-Cantellops N, Tiu TK. Berg Balance Testing. Stat Pearls Publishing; 2023.
Totland TH, Krogh HW, Smedshaug GB, Tornes RA, Bye A, Paur I. Harmonization and standardization of malnutrition screening for all adults–A systematic review initiated by the Norwegian Directorate of Health. Clin Nutr ESPEN. 2022;52:32-49.
Chuansangeam M, Wuthikraikun C, Supapueng O, Muangpaisan W. Prevalence and risk for malnutrition in older Thai people: A systematic review and meta-analysis. Asia Pac J Clin Nutr. 2022;31(1):128-41.
Leung AY, Su JJ, Lee ES, Fung JT, Molassiotis A. Intrinsic capacity of older people in the community using WHO Integrated Care for Older People (ICOPE) framework: a cross-sectional study. BMC Geriatr. 2022;22(1):304.
Zhong B-X, Zhong H-L, Zhou G-Q, Xu W-Q, Lu Y, Zhao Q. Physical performance and risk of hip fracture in community-dwelling elderly people in China: a 4-year longitudinal cohort study. Maturitas. 2021;146:26-33.
Lu F, Li J, Liu X, Liu S, Sun X, Wang X. Diagnostic performance analysis of the Integrated Care for Older People (ICOPE) screening tool for identifying decline in intrinsic capacity. BMC Geriatr. 2023;23(1):509.
Power L, Mullally D, Gibney ER, Clarke M, Visser M, Volkert D, et al. A review of the validity of malnutrition screening tools used in older adults in community and healthcare settings - A MaNuEL study. Clin Nutr ESPEN. 2018;24:1-13.
Serón-Arbeloa C, Labarta-Monzón L, Puzo-Foncillas J, Mallor-Bonet T, Lafita-López A, Bueno-Vidales N, et al. Malnutrition Screening and Assessment. Nutrients. 2022;14(12): 2392.
Guigoz Y, Vellas B. Nutritional assessment in older adults: MNA® 25 years of a screening tool & a reference standard for care and research; what next? J Nutr Health Aging. 2021;25(4):528-83.
Reber E, Gomes F, Vasiloglou MF, Schuetz P, Stanga Z. Nutritional risk screening and assessment. J Clin Med. 2019;8(7):1065.
Isautier JM, Bosnić M, Yeung SS, Trappenburg MC, Meskers CG, Whittaker AC, et al. Validity of nutritional screening tools for community-dwelling older adults: a systematic review and meta-analysis. J Am Med Dir Assoc. 2019;20(10):1351.e13-1351.e25.
Vellas B, Guigoz Y, Garry PJ, Nourhashemi F, Bennahum D, Lauque S, et al. The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition. 1999;15(2):116-22.
Kooij L, Vos PJ, Dijkstra A, van Harten WH. Effectiveness of a mobile health and self-management app for high-risk patients with chronic obstructive pulmonary disease in daily clinical practice: mixed methods evaluation study. JMIR Mhealth Uhealth. 2021;9(2):e21977.
Ritchey K, Olney A, Chen S, Phelan EA. STEADI self-report measures independently predict fall risk. Gerontol Geriatr Med. 2022;8:23337214221079222.
Merchant RA, Tsoi C, Tan W, Lau W, Sandrasageran S, Arai H. Community-based peer-led intervention for healthy ageing and evaluation of the ‘HAPPY’program. J Nutr Health Aging. 2021;25(4):520-7.
Taheri-Kharameh Z, Malmgren Fänge A, Ekvall Hansson E, Bashirian S, Heidarimoghadam R, Poorolajal J, et al. Development of a mobile application to screen and manage fall risks in older people. Disabil Rehabil Assist Technol. 2022;17(3):362-7.
Deapartment of Older Persons. Elderly statistics [Internet]. 2022. cited 2024 September 13. Available from: https://www.dop.go.th/th/know/side/1/1/2449
Ko-amornsup W, Siriussawakul A, Aosangdeeku K, Preedachitkul R, Srinonprasert V, Somnuke P, et al. Health survey of monks residing in urban areas: The Bangkok Noi model. Siriraj Med J. 2024;76(11):746-57.
Coordinated Care Plan to Prevent Older Adult Falls [Internet]. cdc.gov/steadi. Available from: https://www.cdc.gov/steadi/pdf/Steadi-Coordinated-Care-Plan.pdf
Casey CM, Parker EM, Winkler G, Liu X, Lambert GH, Eckstrom E. Lessons Learned From Implementing CDC’s STEADI Falls Prevention Algorithm in Primary Care. Gerontologist. 2017;57(4):787-96.
Loonlawong S, Limroongreungrat W, Rattananupong T, Kittipimpanon K, Saisanan Na Ayudhaya W, Jiamjarasrangsi W. Predictive validity of the Stopping Elderly Accidents, Deaths & Injuries (STEADI) program fall risk screening algorithms among community-dwelling Thai elderly. BMC Med. 2022;20(1):78.
Lin C-C, Meardon S, O’Brien K. The Predictive Validity and Clinical Application of Stopping Elderly Accidents, Deaths & Injuries (STEADI) for Fall Risk Screening. Adv Geriatr Med Res. 2022;4(3):e220008.
Lohman MC, Crow RS, DiMilia PR, Nicklett EJ, Bruce ML, Batsis JA. Operationalisation and validation of the Stopping Elderly Accidents, Deaths, and Injuries (STEADI) fall risk algorithm in a nationally representative sample. J Epidemiol Community Health. 2017;71(12):1191-7.
Nithman RW, Vincenzo JL. How steady is the STEADI? Inferential analysis of the CDC fall risk toolkit. Arch Gerontol Geriatr. 2019;83:185-94.
Burns ER, Lee R, Hodge SE, Pineau VJ, Welch B, Zhu M. Validation and comparison of fall screening tools for predicting future falls among older adults. Arch Gerontol Geriatr. 2022;101:104713.
Donini LM, Marrocco W, Marocco C, Lenzi A. Validity of the Self- Mini Nutritional Assessment (Self- MNA) for the Evaluation of Nutritional Risk. A Cross- Sectional Study Conducted in General Practice. J Nutr Health Aging. 2018;22(1):44-52.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














