Prevalence of Geriatric Syndromes and Satisfaction of Service in Older People Receiving Annual Health Screening at the Check-up Clinic, Siriraj Hospital
DOI:
https://doi.org/10.33192/smj.v77i1.271734Keywords:
geriatric syndromes, cognitive impairment, comprehensive geriatric assessment, patient satisfaction, health screeningAbstract
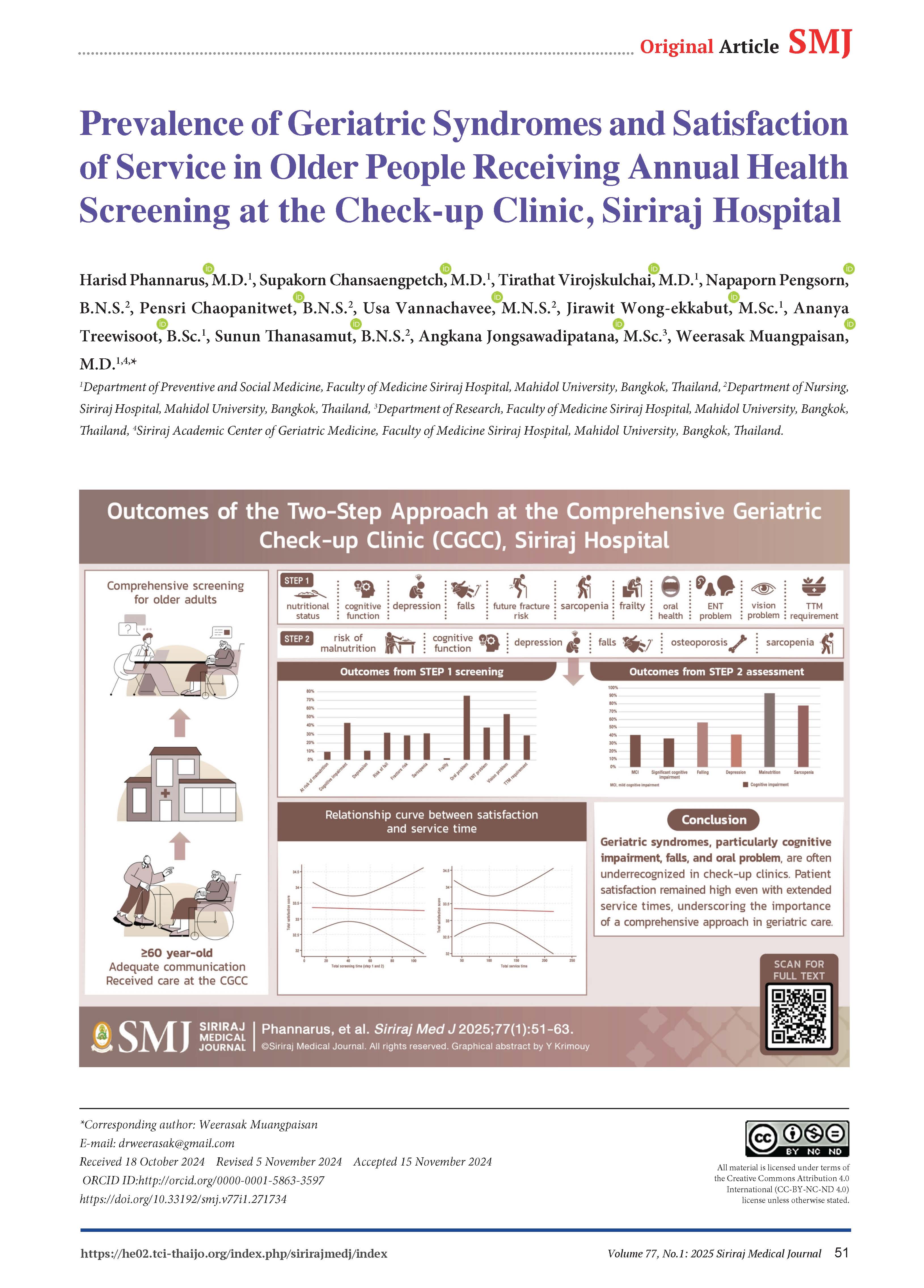
Objective: To assess the prevalence of geriatric syndromes (GSs) and evaluate service satisfaction among older patients attending a comprehensive geriatric check-up clinic (CGCC) at Siriraj Hospital.
Materials and Methods: A cross-sectional study was conducted at the CGCC from December 2021 to November 2022. Participants aged 60 years and older were screened using a two-step approach; short screening by a standard questionnaire followed by an in-depth assessment. GSs were identified through standardized tools, and patient satisfaction was assessed using a structured questionnaire.
Results: Of 159 participants, 67.9% were women, with a mean age of 66.6 ± 6 years. In step 1, 43.7% showed cognitive impairment, 29.1% had a risk of falls, and 76% reported oral health issues. Step 2 confirmed cognitive impairment in 40.6%, malnutrition risk in 93.3%, and sarcopenia in 78%. The mean satisfaction score was 33.3 ± 2.5 out of 35 points. Total service time averaged 104.2 ± 36.9 minutes.
Conclusion: In a health check-up clinic where GSs are often under-recognized, GSs, particularly cognitive impairment, fall risk, and oral health issues, are prevalent. Despite extended service times, patient satisfaction remained high, highlighting the importance of comprehensive screening in geriatric care.
References
Carlson C, Merel SE, Yukawa M. Geriatric syndromes and geriatric assessment for the generalist. Med Clin North Am. 2015;99(2):263-79.
Praditsuwan R. Current Knowledge in Geriatric Syndromes. Siriraj Med J. 2007;59(2):79-81.
Möller J, Rausch C, Laflamme L, Liang Y. Geriatric syndromes and subsequent health-care utilization among older community dwellers in Stockholm. Eur J Ageing. 2022;19(1):19-25.
Rausch C, van Zon SKR, Liang Y, Laflamme L, Möller J, de Rooij SE, et al. Geriatric Syndromes and Incident Chronic Health Conditions Among 9094 Older Community-Dwellers: Findings from the Lifelines Cohort Study. J Am Med Dir Assoc. 2022;23(1):54-9.e2.
Cheung JTK, Yu R, Wu Z, Wong SYS, Woo J. Geriatric syndromes, multimorbidity, and disability overlap and increase healthcare use among older Chinese. BMC Geriatr. 2018;18(1):147.
Limpawattana P, Phimson K, Sookprasert A, Sirithanaphol W, Chindaprasirt J. Prevalence of Geriatric Syndromes in Elderly Cancer Patients Receiving Chemotherapy. Curr Gerontol Geriatr Res. 2020;2020:9347804.
Aging and the Labor Market in Thailand [Internet]. 2021 [cited 2024 September 21]. Available from: https://www.worldbank.org/en/country/thailand/publication/aging-and-the-labor-market-in-thailand.
Demographics of Thailand [Internet]. Statista. 2024 [cited 2024 September 21]. Available from: https://www.statista.com/statistics/713667/thailand-forecast-aging-population/.
Somnuke P, Pongraweewan O, Siriussawakul A. Optimizing Perioperative Care for Elderly Surgical Patients: A Review of Strategies and Evidence-Based Practices. Siriraj Med J. 2024;76(7):465-72
Screening guideline for general population. In: Department of Medical Services, editor.: Institute of Medical Research & Technology Assessment (IMRTA); 2022.
Heinisch O. Cochran, W. G. Sampling Techniques, 2. Aufl. John Wiley and Sons, New York, London 1963. Preis s. Biom Z. 1965;7(3):203.
Pramyothin P, Keawtanom S, Dawilai S, Sarasak R, Sukaruttanawong C, Triyen W, et al. Performance of a new national nutrition screening tool (spent nutrition screening tool) in hospitalized non-critically ill adults at an academic medical center. Clin Nutr. 2018;37:S236-S7.
Rubenstein LZ, Harker JO, Salvà A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci. 2001;56(6):M366-72.
Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T, et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13(9):782-8.
World Health Organization. Integrated care for older people (ICOPE): guidance for person-centred assessment and pathways in primary care. 2019.
Train the Brain Forum Committee. Thai Mental State Examination (TMSE). Siriraj Hosp Gaz. 1993;45:359-74.
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695-9.
Arunpongpaisal S, Kongsuk T, Maneethorn N, Maneethorn B, Wannasawek K, Leejongpermpoon J, et al. Development and validity of two-question screening test for depressive disorders in Northeastern Thai community. Asian J Psychiatr. 2009;2(4):149-52.
Costantini L, Pasquarella C, Odone A, Colucci ME, Costanza A, Serafini G, et al. Screening for depression in primary care with Patient Health Questionnaire-9 (PHQ-9): A systematic review. J Affect Disord. 2021;279:473-83.
Visanuyothin S, Ittivisawakul N. The treatment of people with depression guideline The Journal of Boromrajonani College of Nursing, Nakhonratchasima. 2010;16(1).
Centers for Disease Control and Prevention (CDC), Stopping Elderly Accidents Deaths & Injuries (STEADI). Algorithm for Fall Risk Screening, Assessment, and Intervention. 2019.
Bischoff HA, Stähelin HB, Monsch AU, Iversen MD, Weyh A, von Dechend M, et al. Identifying a cut-off point for normal mobility: a comparison of the timed 'up and go' test in community-dwelling and institutionalised elderly women. Age Ageing. 2003;32(3):315-20.
Lord SR, Murray SM, Chapman K, Munro B, Tiedemann A. Sit-to-stand performance depends on sensation, speed, balance, and psychological status in addition to strength in older people. J Gerontol A Biol Sci Med Sci. 2002;57(8):M539-43.
Watts NB. The Fracture Risk Assessment Tool (FRAX®): applications in clinical practice. J Womens Health (Larchmt). 2011;20(4):525-31.
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, et al. Clinician's Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int. 2014;25(10):2359-81.
Akarapornkrailert P, Muangpaisan W, Boonpeng A, Daengdee D. Validation of the Thai version of SARC-F, MSRA-7, and MSRA-5 questionnaires compared to AWGS 2019 and sarcopenia risks in older patients at a medical outpatient clinic. Osteoporos Sarcopenia. 2020;6(4):205-11.
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J Am Med Dir Assoc. 2020;21(3):300-7.e2.
Sriwong W, Mahavisessin W, Srinonprasert V, Siriussawakul A, Aekplakorn W, Limpawattana P, et al. Validity and reliability of the Thai version of the simple frailty questionnaire (T-FRAIL) with modifications to improve its diagnostic properties in the preoperative setting. BMC Geriatr. 2022;22(1):161.
Lin CC, Meardon S, O'Brien K. The Predictive Validity and Clinical Application of Stopping Elderly Accidents, Deaths & Injuries (STEADI) for Fall Risk Screening. Adv Geriatr Med Res. 2022;4(3).
Loonlawong S, Limroongreungrat W, Rattananupong T, Kittipimpanon K, Saisanan Na Ayudhaya W, Jiamjarasrangsi W. Predictive validity of the Stopping Elderly Accidents, Deaths & Injuries (STEADI) program fall risk screening algorithms among community-dwelling Thai elderly. BMC Med. 2022;20(1):78.
Trevethan R. Sensitivity, Specificity, and Predictive Values: Foundations, Pliabilities, and Pitfalls in Research and Practice. Front Public Health. 2017;5:307.
Besora-Moreno M, Llauradó E, Tarro L, Solà R. Social and Economic Factors and Malnutrition or the Risk of Malnutrition in the Elderly: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients. 2020;12(3).
Chuansangeam M, Wuthikraikun C, Supapueng O, Muangpaisan W. Prevalence and risk for malnutrition in older Thai people: A systematic review and meta-analysis. Asia Pac J Clin Nutr. 2022;31(1):128-41.
Coll PP, Lindsay A, Meng J, Gopalakrishna A, Raghavendra S, Bysani P, et al. The Prevention of Infections in Older Adults: Oral Health. J Am Geriatr Soc. 2020;68(2):411-6.
Bourne RRA, Flaxman SR, Braithwaite T, Cicinelli MV, Das A, Jonas JB, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(9):e888-e97.
Guthrie DM, Davidson JGS, Williams N, Campos J, Hunter K, Mick P, et al. Combined impairments in vision, hearing and cognition are associated with greater levels of functional and communication difficulties than cognitive impairment alone: Analysis of interRAI data for home care and long-term care recipients in Ontario. PLoS One. 2018;13(2):e0192971.
Hsu AK, Bassett SM, O'Dwyer LC, McHugh M, Heinemann AW, Jordan N, et al. Cost-Effectiveness of Hearing Screening in Older Adults: A Scoping Review. Res Aging. 2022;44(2):186-204.
Lee Y, Kasper JD. Assessment of medical care by elderly people: general satisfaction and physician quality. Health Serv Res. 1998;32(6):741-58.
Kuo RJ, Wu YH, Hsu TS, Chen LK. Improving outpatient services for elderly patients in Taiwan: a qualitative study. Arch Gerontol Geriatr. 2011;53(2):e209-17.
Daure A, Chicoulaa B, Lagourdette C, Escourrou E, Secher M, Oustric S, et al. [General practitioners' satisfaction after a geriatric assessment into primary care: data from FAP study]. Geriatr Psychol Neuropsychiatr Vieil. 2019;17(1):31-7.
Batalden PB, Davidoff F. What is "quality improvement" and how can it transform healthcare? Qual Saf Health Care. 2007;16(1):2-3.
Bispo Júnior JP. Social desirability bias in qualitative health research. Rev Saude Publica. 2022;56:101.
Kroneman M, Verheij R, Tacken M, van der Zee J. Urban-rural health differences: primary care data and self reported data render different results. Health Place. 2010;16(5):893-902.
Sanford AM, Morley JE, Berg-Weger M, Lundy J, Little MO, Leonard K, et al. High prevalence of geriatric syndromes in older adults. PLoS One. 2020;15(6):e0233857.
Rafters SL, Schleper J, Lean N, Hwang M, Rohra A, Lillington L. Geriatric Syndrome Screening: Implementing an Evidence-Based Process in Hospitalized Older Adults With Cancer. Clin J Oncol Nurs. 2021;25(3):297-304.
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














