Effectiveness of a Brain Training Program on the Cognitive Function of Sepsis Survivors: A Randomized Controlled Trial Study
DOI:
https://doi.org/10.33192/smj.v77i3.272129Keywords:
Sepsis survivors, brain training program, cognitive functionsAbstract
Objective: This study aimed to evaluate the effectiveness of a brain training program designed to enhance the cognitive function of sepsis survivors.
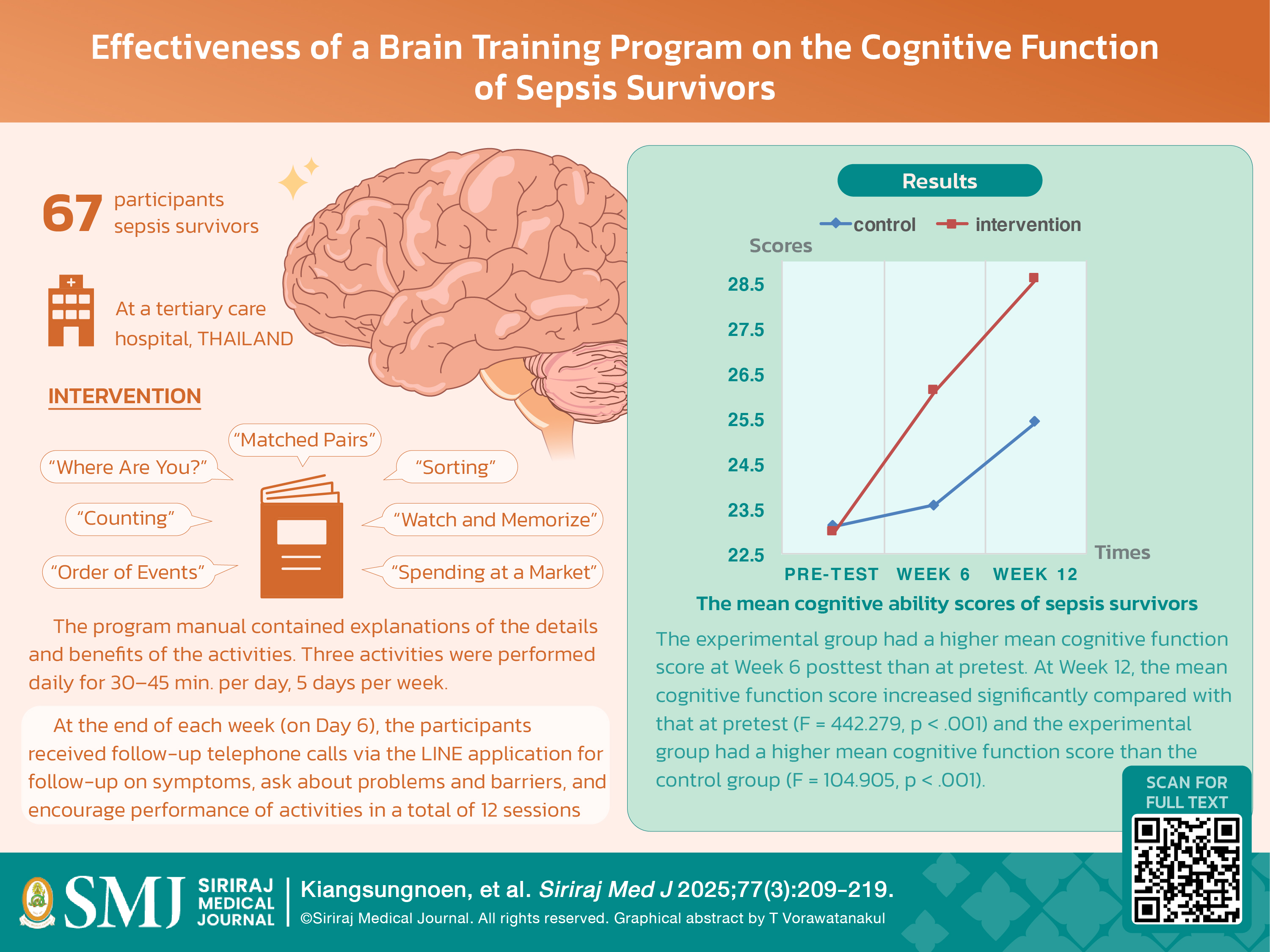
Materials and Methods: We conducted a single-blind randomized controlled trial at a tertiary care hospital involving 67 participants aged over 18 years with participants randomly assigned to two groups, an experimental group (n=33) receiving the brain training program, and a control group (n=34) receiving standard care only. We measured cognitive function at three different time points: Baseline, Week 6, and Week 12, using the Thai Mental State Examination for testing and repeated measure ANOVA for statistical analysis.
Results: The experimental group had a higher mean cognitive function score at Week 6 posttest than at pretest. At Week 12, the mean cognitive function score increased significantly compared with that at pretest (F = 442.279, p < .001) and the experimental group had a higher mean cognitive function score than the control group (F = 104.905, p < .001).
Conclusion: The brain training program significantly increased the cognitive function levels of sepsis survivors in 6–12 weeks. The result of this study shows the benefits of a brain training program in increasing cognitive functions. Therefore, such a brain training program should be implemented among sepsis survivors to improve their cognitive functions.
References
Rudd KE, Johnson SC, Agesa Km, Shackelford KA, Tsoi D, Kievlan DR, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395:200-11.
Fleischmann-Struzek C, Mellhammar L, Rose N, Cassini A, Rudd KE, Schlattmann P, et al. Incidence and mortality of hospital- and ICU-treated sepsis: results from an updated and expanded systematic review and meta-analysis. Intensive Care Med. 2020;46(8):1552-62.
Cheung AM, Tansey CM, Tomlinson G, Diaz-Granados N, Matté A, Barr A, et al. Two-year outcomes, health care use, and costs of survivors of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2016;174:538-44.
Steele AM, Starr ME, Saito H. Late Therapeutic Intervention with Antibiotics and Fluid Resuscitation Allows for a Prolonged Disease Course with High Survival in a Severe Murine Model of Sepsis. Shock. 2017;6:726-34.
Rhee C, Klompas M. Sepsis trends: increasing incidence and decreasing mortality, or changing denominator? J Thorac Dis. 2020;12(Suppl 1):S89-S100.
Prescott HC, Angus DC. Enhancing recovery from sepsis: a review. JAMA. 2018;319(1):62-75.
Thompson K, Taylo RC, Jan S, Li Q, Hammond N, Myburgh J, et al. Health-related outcomes of critically ill patients with and without sepsis. Intensive Care Med. 2018;44(8):1249-57.
Montel Z, Perl A, Marck M, Mehdi SF, Lowell B, Bathija S, et al. Post-sepsis syndrome-an evolving entity that afflicts survivors of sepsis. Mol Med. 2020;26(1):6.
Diamond A. Executive functions. Annu Rev Psychol. 2013;64:135-68.
Martínez L, Prada E, Satler C, C H Tavares M, Tomaz C. Executive dysfunctions: The role in attention deficit hyperactivity and post-traumatic stress neuropsychiatric disorders. Front Psychol. 2016;7:1230.
Jiang Y, Ji M, Yang J. Current understanding of long-term cognitive impairment after sepsis. Front Immunol. 2022;13:1855006.
Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787-94.
Annane D, Sharshar T. Cognitive decline after sepsis. Lancet Respir Med. 2015;3(1):61-9.
Sepsis Alliance. Sepsis survivors. 2022. Available from: https://www.sepsis.org/sepsis-survivor-week. Accessed 27 Sept 2022.
Gyawali B, Ramakrishna K, Dhamoon AS. Sepsis: The evolution in definition, pathophysiology, and management. SAGE Open Med. 2019;7:2050312119835043.
Hebb DO, Hebb DO. The organization of behavior. New York: Wiley. 1949.
Wang S, Hammes J, Khan S, Gao S, Harrawood A, Martinez S, et al. Improving recovery and outcomes every day after the ICU (IMPROVE): study protocol for a randomized controlled trial. Trials. 2018;19(1):196.
Patel MB, Morandi A, Pandharipande PP. What's new in post-ICU cognitive impairment? Intensive Care Med. 2015;41(4):708-11.
Shao C, Gu L, Mei Y, Li M. Analysis of the risk factors for cognitive impairment in post intensive care syndrome patient. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2017;29(8):716-20.
Wang LL. The clinical study of cognitive function in survivors of sepsis. Tianjin, China: Tianjin Medical Uni Varsity, 2018; p. 52.
Li BB. The present status and influence factors of post-intensive care syndrome in adult after cardiac surgery [PhD dissertation]. Shandong, China: Shandong University; 2018. p. 90.
Yan XX, Han R, Yue Y, Song K. Clinical study on influencing factors of early cognitive impairment in critically ill patients after ICU. Chi J Gen Practice. 2020;18(5):746-48.
Hartley P, Gibbins N, Saunders A, Alexander K, Conroy E, Dixon R, et al. The association between cognitive impairment and functional outcome in hospitalized older patients: a systematic review and meta-analysis. Age Ageing. 2017;46(4):559-67.
Brück E, Schandl A, Bottai M, Sackey P. The impact of sepsis, delirium, and psychological distress on self-rated cognitive
function in ICU survivors-a prospective cohort study. J Intensive Care. 2018;6:2.
Zhao J, Yao L, Wang C, Sun Y, Sun Z. The effects of cognitive intervention on cognitive impairments after intensive care unit admission. Neuropsychol Rehabil. 2017;27(3):301-17.
Brummel NE, Girard TD, Ely EW, Pandharipande PP, Morandi A, Hughes CG, et al. Feasibility and safety of early combined cognitive and physical therapy for critically ill medical and surgical patients: the Activity and Cognitive Therapy in ICU (ACT-ICU) trial. Intensive Care Med. 2014;40(3):370-9.
Jackson JC, Ely EW, Morey MC, Anderson VM, Denne LB, Clune J, et al. Cognitive and physical rehabilitation of intensive care unit survivors: results of the RETURN randomized controlled pilot investigation. Crit Care Med. 2012;40(4):1088-97.
Mehlhorn J, Freytag A, Schmidt K, Brunkhorst FM, Graf J, Troitzsch U, et al. Rehabilitation interventions for post intensive care syndrome: a systematic review. Crit Care Med. 2014;42(5):1263-71.
Li HX, Bai CM, Wang RX, Zheng T, Sun HB. Correlation between negative emotions and cognitive impairment in patients with anxiety disorder. J Int Psychol. 2017;44:68-71.
Zhu RR, Gan YQ, Li Y, Xian Z. Mediating effect of positive emotion on relationship between cognition reappraisal and meaning of life in freshmen. Chin. Ment. Health J. 2017;12:490-4.
Lampit A, Hallock H, Valenzuela M. Computerized cognitive training in cognitively healthy older adults: a systematic review and meta-analysis of effect modifiers. PLoS Med. 2014;11(11):e1001756.
Qionglan D, Yuxin Y, Qibing T, Mei Y, An L, Hongjun X, et al. Effects of early cognitive rehabilitation training on cognitive function and quality of life in critically ill patients with cognitive impairment: A randomized controlled trial. Aust Crit Care. 2023;36(5):708-15.
Muangpaisan W, Assantachai P, Sitthichai K, Richardson K, Brayne C. The distribution of Thai Mental State Examination scores among non-demented elderly in suburban Bangkok metropolitan and associated factors. J Med Assoc Thai. 2015; 98(9):916-24.
Published
How to Cite
License
Copyright (c) 2025 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














