Referral Patterns, Co-occurring Conditions and Survival Outcomes of Biliary Atresia in Thailand: A Data Mining Study from the National Health Security Office Registry
DOI:
https://doi.org/10.33192/smj.v77i5.272428Keywords:
Biliary atresia, children, infants, survival, ThailandAbstract
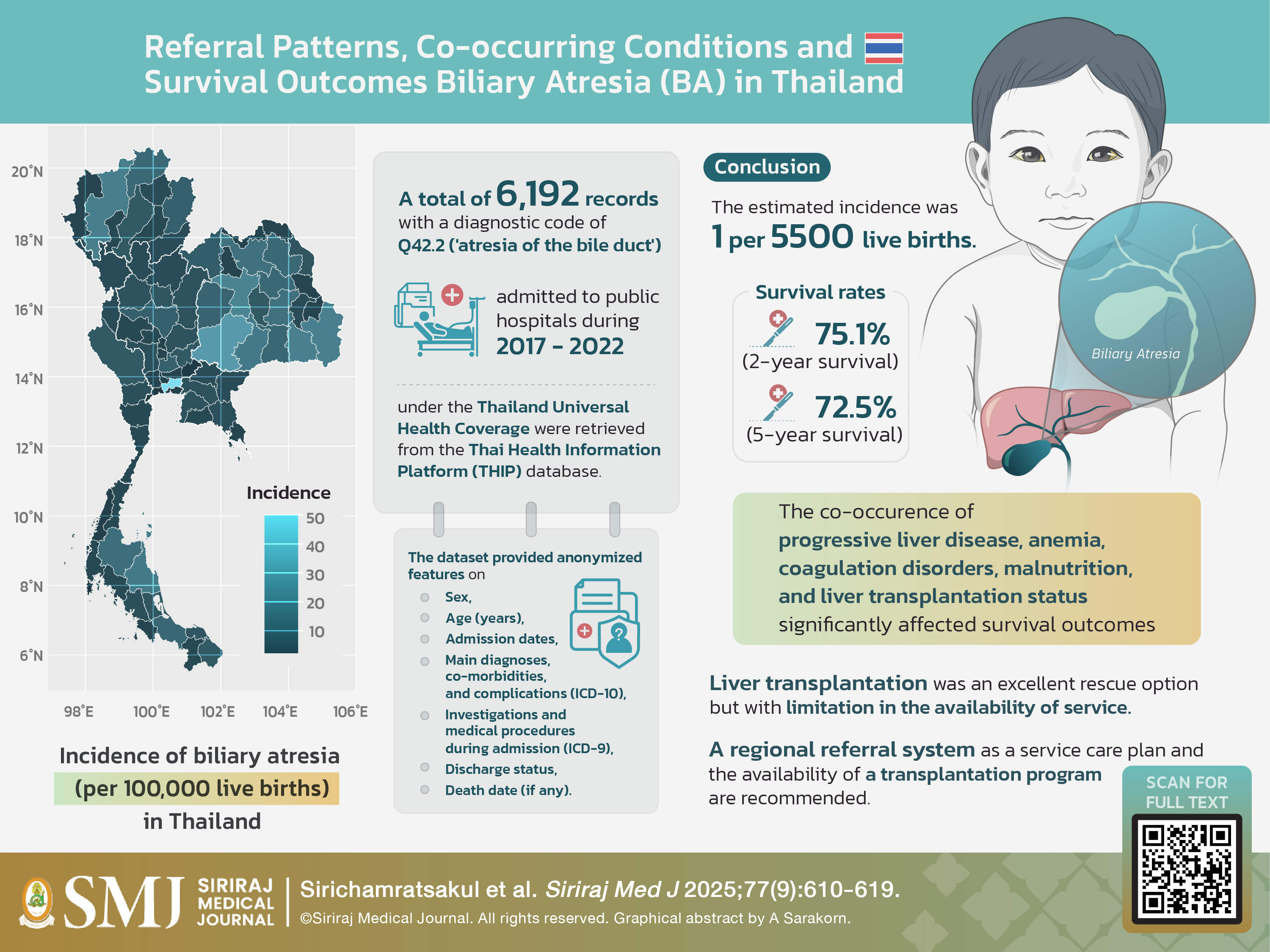
Objective: This study aimed to identify comorbidities and referral patterns in biliary atresia (BA) patients and analyze their influence on survival outcomes using a large national reimbursement cohort.
Materials and Methods: Data were extracted from the National Health Security Office (NHSO) registry via the Thai Health Information Portal (THIP). Patients under six years with a diagnosis of BA between 2017 and 2022 were included. Comorbidities, referral patterns, and survival were analyzed; association rule analysis was performed using the mlxtend package in Python 3.9, whereas survival analysis was conducted using the Kaplan Meier survival curve.
Results: In total, 957 BA cases among 4,168 admissions were included. The estimated annual incidence was 108.7 cases (1.8 per 10,000 live births). The 2- and 5-year survival rates were 75.1% and 72.5%, respectively. Association rules analysis revealed that metabolic disorders, liver cirrhosis, and portal hypertension had a high confidence of co-occurrence with BA. Anemia, coagulation disorders, malnutrition, liver cirrhosis, hepatic failure, ascites, and hypoalbuminemia were significantly associated with poorer survival outcomes. Cases with more than one referral before a definitive surgery significantly had poorer survival outcomes.
Conclusion: Overall, BA patients in Thailand had fair survival rates. Co-occurring progressive liver diseases, anemia, coagulation disorders, malnutrition, and prolonged referrals significantly contribute to poorer survival. Managing these peri-operative factors might improve the outcome of this devastating disease.
References
Davenport M. Biliary atresia: clinical aspects. Semin Pediatr Surg. 2012;21(3):175-84.
Schreiber RA, Harpavat S, Hulscher JBF, Wildhaber BE. Biliary Atresia in 2021: Epidemiology, Screening and Public Policy. J Clin Med. 2022;11(4).
Cavallo L, Kovar EM, Aqul A, McLoughlin L, Mittal NK, Rodriguez-Baez N, et al. The Epidemiology of Biliary Atresia: Exploring the Role of Developmental Factors on Birth Prevalence. J Pediatr. 2022;246:89-94 e2.
Hopkins PC, Yazigi N, Nylund CM. Incidence of Biliary Atresia and Timing of Hepatoportoenterostomy in the United States. J Pediatr. 2017;187:253-7.
Nakayama DK. Morio Kasai Corrects the Uncorrectable: Hepatic Portoenterostomy for Biliary Atresia. J Pediatr Surg. 2024:161765.
Nio M, Ohi R, Miyano T, Saeki M, Shiraki K, Tanaka K, et al. Five- and 10-year survival rates after surgery for biliary atresia: a report from the Japanese Biliary Atresia Registry. J Pediatr Surg. 2003;38(7):997-1000.
Sangkhathat S, Patrapinyokul S, Tadtayathikom K, Osatakul S. Peri-operative factors predicting the outcome of hepatic porto-enterostomy in infants with biliary atresia. J Med Assoc Thai. 2003;86(3):224-31.
Davenport M, Ong E, Sharif K, Alizai N, McClean P, Hadzic N, et al. Biliary atresia in England and Wales: results of centralization and new benchmark. J Pediatr Surg. 2011;46(9):1689-94.
Tomita H, Shimojima N, Sasaki H, Shimotakahara A, Yamada Y, Kuroda T, et al. Predicting Cirrhosis and Poor Outcomes of Bile Drainage Surgery for Biliary Atresia: A Multicentric Observational Study in Japan. Ann Surg. 2024;279(4):692-8.
Sirichamratsakul K, Laochareonsuk W, Surachat K, Sangkhathat S. Population-based prevalence study of common congenital malformations of the alimentary tract and abdominal wall in Thailand: a study using data from the National Health Security Office. World J Pediatr Surg. 2023;6(3):e000540.
Wu WT, Li YJ, Feng AZ, Li L, Huang T, Xu AD, et al. Data mining in clinical big data: the frequently used databases, steps, and methodological models. Mil Med Res. 2021;8(1):44.
Ma H, Ding J, Liu M, Liu Y. Connections between Various Disorders: Combination Pattern Mining Using Apriori Algorithm Based on Diagnosis Information from Electronic Medical Records. Biomed Res Int. 2022;2022:2199317.
Arpornsujaritkun N, Leelaudomlipi S, Sobhonslidsuk A, Mingphruedhi S, Jongjirasiri S, Intraprasong P, et al. Outcome of Living Donor Hepatectomy for Pediatric Liver Transplantation: Report of 100 Cases at Ramathibodi Hospital. Rama Med J. 2016;39:217-24.
Chieochalakom E, Chiengkriwate P. The Diagnostic Accuracy of Hepatobiliary Scintigraphy and Ultrasonography in Cholestatic Jaundice Infants. Songkla Med J. 2014;32(3):129-37.
Laohapensang M, Srikuancharoen P. The Relationship between Clinical Outcomes After Kasai Operation and Related Factors in Infants with Biliary Atresia. J Med Assoc Thai. 2017;100(Suppl. 4):S99-104.
Wirifai T, Laohawilai S. Outcomes of Kasai Operation for Treatment of Patients with Biliary Atresia at a Tertiary Care Hospital. J Dep Med Serv. 2020;45(4):32-6.
Sangkhathat S, Laochareonsuk W, Maneechay W, Kayasut K, Chiengkriwate P. Variants Associated with Infantile Cholestatic Syndromes Detected in Extrahepatic Biliary Atresia by Whole Exome Studies: A 20-Case Series from Thailand. J Pediatr Genet. 2018;7(2):67-73.
Nio M, Sasaki H, Wada M, Kazama T, Nishi K, Tanaka H. Impact of age at Kasai operation on short- and long-term outcomes of type III biliary atresia at a single institution. J Pediatr Surg. 2010;45(12):2361-3.
Fanna M, Masson G, Capito C, Girard M, Guerin F, Hermeziu B, et al. Management of Biliary Atresia in France 1986 to 2015: Long-term Results. J Pediatr Gastroenterol Nutr. 2019;69(4):416-24.
Tessier MEM, Shneider BL. 60 Days in Biliary Atresia: A Historical Dogma Challenged. Clin Liver Dis (Hoboken). 2020;15(Suppl 1):S3-S7.
Hukkinen M, Ruuska S, Pihlajoki M, Kyronlahti A, Pakarinen MP. Long-term outcomes of biliary atresia patients surviving with their native livers. Best Pract Res Clin Gastroenterol. 2022;56-57:101764.
Choungboonsri C. Does Kasai operation prior to liver transplantation affect peri-operative outcomes in children with biliary atresia? Chulalongkorn Med J. 2021;65(1):45-9.
Sihaklang B, Getsuwan S, Pattanaprateep O, Butsriphum N, Lertudomphonwanit C, Tanpowpong P, et al. Cost-effectiveness analysis of liver transplantation in biliary atresia according to the severity of end-stage liver disease. BMC Pediatr. 2023;23(1):439.
Gesprasert G, Chongsrisawat V, Tantemsapya N, Thirapattaraphan C, Nonthasoot B, Tovikkai C, et al. The first report of pediatric liver transplantation in Thailand from the Thai liver transplant registry. Transplantation. 2020;104(S3):S536.
Anouti A, Patel MS, VanWagner LB, Lee WM, Fung JJ, Cholankeril G, et al. Biliary atresia and liver transplantation in the United States: A contemporary analysis. Liver Int. 2023;43(10):2198-209.
Umeshita K, Eguchi S, Egawa H, Haga H, Kasahara M, Kokudo N, et al. Liver transplantation in Japan: Registry by the Japanese Liver Transplantation Society. Hepatol Res. 2019;49(9):964-80.
Ginstrom DA, Hukkinen M, Kivisaari R, Pakarinen MP. Biliary Atresia-associated Cholangitis: The Central Role and Effective Management of Bile Lakes. J Pediatr Gastroenterol Nutr. 2019;68(4):488-94.
Burns J, Davenport M. Adjuvant treatments for biliary atresia. Transl Pediatr. 2020;9(3):253-65.
Lykavieris P, Chardot C, Sokhn M, Gauthier F, Valayer J, Bernard O. Outcome in adulthood of biliary atresia: a study of 63 patients who survived for over 20 years with their native liver. Hepatology. 2005;41(2):366-71.
Jung E, Park WH, Choi SO. Late complications and current status of long-term survivals over 10 years after Kasai portoenterostomy. J Korean Surg Soc. 2011;81(4):271-5.
de Vries W, Homan-Van der Veen J, Hulscher JB, Hoekstra-Weebers JE, Houwen RH, Verkade HJ, et al. Twenty-year transplant-free survival rate among patients with biliary atresia. Clin Gastroenterol Hepatol. 2011;9(12):1086-91.
Qisthi SA, Saragih DSP, Sutowo DW, Sirait DN, Imelda P, Kencana SMS, et al. Prognostic Factors for Survival of Patients with Biliary Atresia Following Kasai Surgery. Kobe J Med Sci. 2020;66(2):E56-E60.
Laohapensang M, Srikuancharoen P, Tantemsapya N. Factors Related to the Clinical Outcomes of the Kasai Procedure in Infants with Biliary Atresia. Siriraj Med J. 2020;72(3):226-37.
Analysis of sequential secondary cytogenetic changes in Ewing's sarcoma: A xenotransplantation model. Virchows Arch. 2005;447(2):227–552.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2025 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














