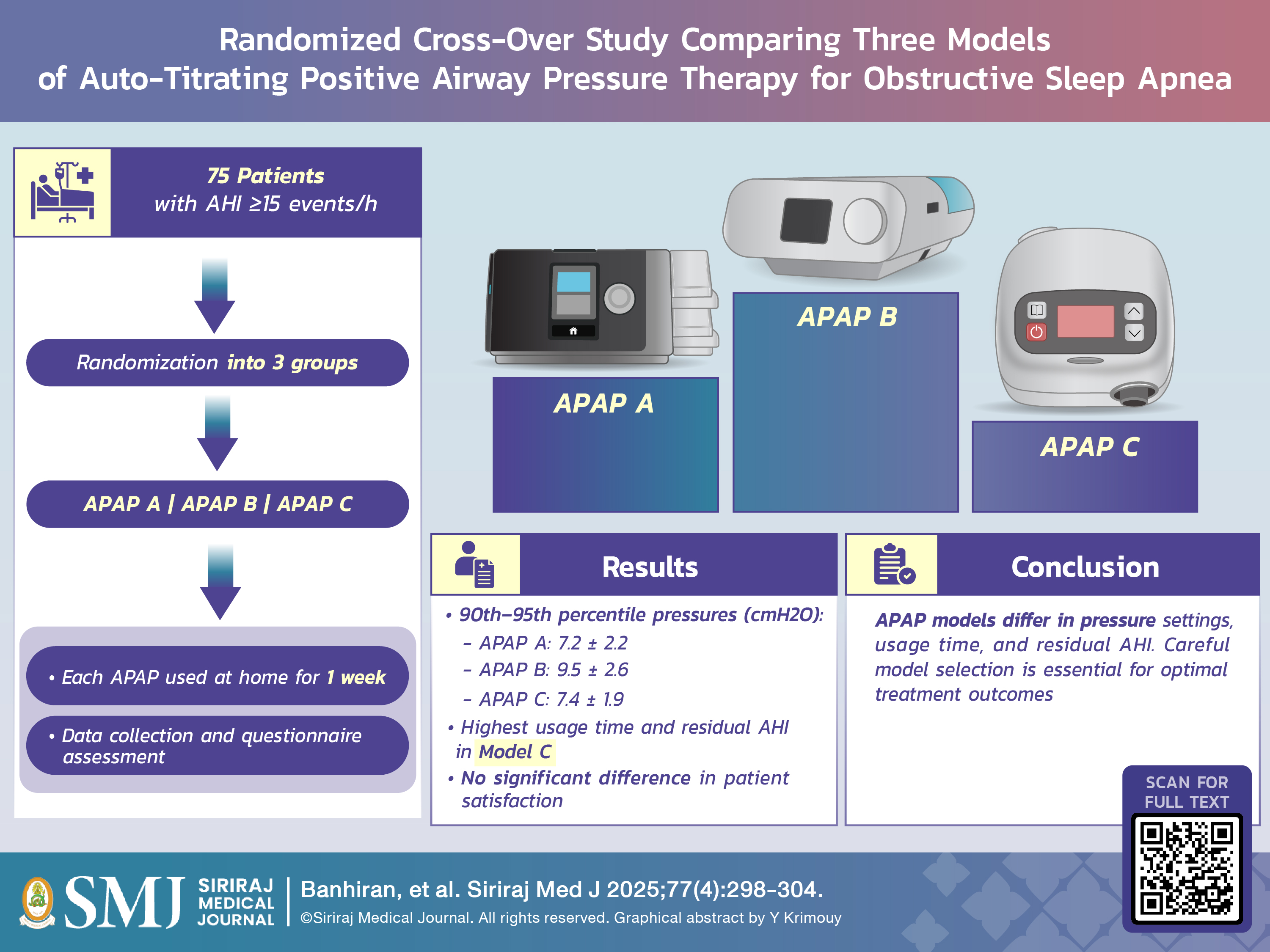
Randomized Cross-Over Study Comparing Three Models of Auto-Titrating Positive Airway Pressure Therapy for Obstructive Sleep Apnea
DOI:
https://doi.org/10.33192/smj.v77i4.272529Keywords:
Auto-titrating positive airway pressure, APAP, obstructive sleep apnea, pressure titration, continuous positive airway pressure, CPAPAbstract
Objective: To compare pressure, average usage time, residual apnea-hypopnea index (AHI), and patient satisfaction across three models of auto-titrating positive airway pressure (APAP) (A, B, and C refers to APAP devices — APEX, Philips, and Hoffrichter, respectively).
Materials and Methods: Seventy-five adult patients with an AHI of ≥15 events/h who were willing to use APAP were included and randomly assigned to three groups with different APAP sequences generated by computer randomization. After using each model at home for a week, patients returned to the clinic for data collection and switched to the next model. They completed questionnaires regarding their symptoms before and after the therapeutic session.
Results: Data from 62 patients (43 males, 19 females) who completed the research protocol were analyzed. The average 90th–95th percentile pressures for APAP models A, B and C were 7.2 ± 2.2, 9.5 ± 2.6 and 7.4 ± 1.9 cmH2O, respectively (p < 0.001), with an intra-class correlation coefficient (ICC) of 0.52 (95% CI 0.22-0.70). In addition, average usage time and residual AHI differed significantly, with the highest values in model C. However, no significant differences were found in mean pressure or patient satisfaction across the three APAP models.
Conclusion: The 90th–95th percentile pressures, average time usage, and residual AHI varied among APAP models, showing only moderate consistency. These findings suggest that careful consideration is required when selecting an APAP model for home use, as it may affect pressure determination and treatment outcomes.
References
Mehra R, Moul DE, Strohl KP. Sleep Breathing Disorder: Clinical Overview. In: Kryger M, Roth T, editors. Principles and Practice of Sleep Medicine. 6th ed. Philadelphia, PA: Elsevier; 2017. p. 167-73.
Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP. Pathophysiology of sleep apnea. Physiol Rev. 2010;90(1):47-112.
Rungmanee S, Banhiran W, Keskool P, Assanasen P, Chotinaiwattarakul W, Nujchanart N. Characteristics and clinical presentations of patients at the Siriraj snoring clinic. Siriraj Med J. 2020;72(3):202-8.
Franklin KA, Lindberg E. Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea. J Thorac Dis. 2015;7(8):1311-22.
Sompradeekul S, Maranetra N, Naruman C, Nana A. The Prevalence of Obstructive Sleep Apnea Among Professional Hospital Drivers. Siriraj Med J. 2002;54(10):625-33.
Ungkanont K, Suraseranivongse S, Laohaprasitiporn D,
Vichyanond P. Pediatric Obstructive Sleep Apnea. Siriraj Med J. 2001;53(10):750-3.
Soonthornkes N, Sakornwattananon O, Jirapitakkul J, Nuallaong W. Burnout and Associated Factors among Thai Anesthesiology Residents. Siriraj Med J. 2023;75(10):736-43.
Nantsupawat N, Khamchet S, Buawongpong N, Pinyopornpanish K, Nantsupawat T, Angkurawaranon C, et al. Sleep Quality and Associated Factors in Elderly Patients with Type-2 Diabetes Mellitus. Siriraj Med J. 2023;75(5):392-8.
Dong JY, Zhang YH, Qin LQ. Obstructive sleep apnea and cardiovascular risk: meta-analysis of prospective cohort studies. Atherosclerosis. 2013;229(2):489-95.
Banhiran W, Assanasen P, Metheetrairut C, Nopmaneejumruslers C, Chotinaiwattarakul W, Kerdnoppakhun J. Functional outcomes of sleep in Thai patients with obstructive sleepdisordered breathing. Sleep Breath. 2012;16(3):663-75.
Banhiran W, Assanasen P, Metheetrairut C, Chotinaiwattarakul W. Health-related quality of life in Thai patients with obstructive sleep disordered breathing. J Med Assoc Thai. 2013;96(2):209-16.
Tregear S, Reston J, Schoelles K, Phillips B. Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clin Sleep Med. 2009;5(6):573-81.
Rodenstein D. Sleep apnea: traffic and occupational accidents--individual risks, socioeconomic and legal implications. Respiration. 2009;78(3):241-8.
Epstein LJ, Kristo D, Strollo PJ, Jr., Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263-76.
Lee SA, Paek JH, Han SH. Sleep hygiene and its association with daytime sleepiness, depressive symptoms, and quality of life in patients with mild obstructive sleep apnea. J Neurol Sci. 2015;359(1-2):445-9.
Tuomilehto H, Seppa J, Uusitupa M. Obesity and obstructive sleep apnea--clinical significance of weight loss. Sleep Med Rev. 2013;17(5):321-9.
Aloia MS, Stanchina M, Arnedt JT, Malhotra A, Millman RP. Treatment adherence and outcomes in flexible vs standard continuous positive airway pressure therapy. Chest. 2005;127(6):2085-93.
Juhasz J, Becker H, Cassel W, Rostig S, Peter JH. Proportional positive airway pressure: a new concept to treat obstructive sleep apnoea. Eur Respir J. 2001;17(3):467-73.
Berry RB, Sriram P. Auto-adjusting positive airway pressure treatment for sleep apnea diagnosed by home sleep testing. J Clin Sleep Med. 2014;10(12):1269-75.
Wongsritrang K, Fueangkamloon S. Comparison of the clinical manual titration in obstructive sleep apnea patients. J Med Assoc Thai. 2013;96(9):1159-63.
Kim Y, Koo YS, Lee HY, Lee SY. Can Continuous Positive Airway Pressure Reduce the Risk of Stroke in Obstructive Sleep Apnea Patients? A Systematic Review and Meta-Analysis. PLoS One. 2016;11(1):e0146317.
Kushida CA, Littner MR, Hirshkowitz M, Morgenthaler TI, Alessi CA, Bailey D, et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep. 2006;29(3):375-80.
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, et al. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017;13(3):479-504.
Hui DS, Ng SS, To KW, Ko FW, Ngai J, Chan KK, et al. A randomized controlled trial of an ambulatory approach versus the hospital-based approach in managing suspected obstructive sleep apnea syndrome. Sci Rep. 2017;8:45901.
Guerrero A, Embid C, Isetta V, Farre R, Duran-Cantolla J, Parra O, et al. Management of sleep apnea without high pretest probability or with comorbidities by three nights of portable sleep monitoring. Sleep. 2014;37(8):1363-73.
Nolan GM, Ryan S, O’Connor T M, McNicholas WT. Comparison of three auto-adjusting positive pressure devices in patients with sleep apnoea. Eur Respir J. 2006;28(1):159-64.
Gagnadoux F, Pevernagie D, Jennum P, Lon N, Loiodice C, Tamisier R, et al. Validation of the System One RemStar Auto A-Flex for Obstructive Sleep Apnea Treatment and Detection of Residual Apnea-Hypopnea Index: A European Randomized Trial. J Clin Sleep Med. 2017;13(2):283-90.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2025 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














