Wearable Device versus Polysomnography for the Assessment of Sleep Characteristics in Patients with Sleep Disorders
DOI:
https://doi.org/10.33192/smj.v77i4.272562Keywords:
Wearable device, Fitbit Alta HR®, sleep disorder, ThaiAbstract
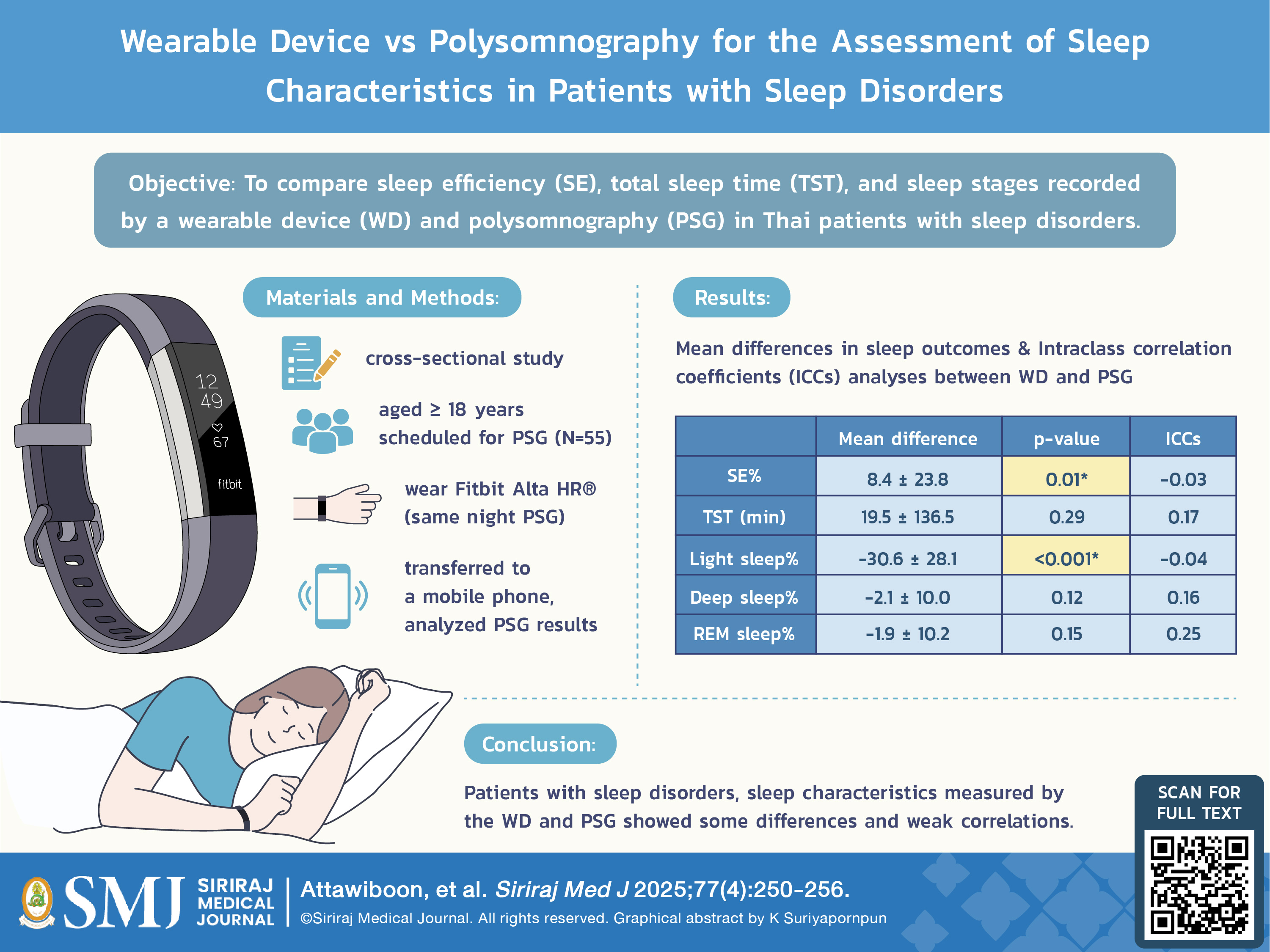
Objective: To compare sleep efficiency (SE), total sleep time (TST), and sleep stages recorded by a wearable device (WD) and polysomnography (PSG) in Thai patients with sleep disorders.
Materials and Methods: Patients aged ≥18 years scheduled for PSG were included in this cross-sectional study. All research subjects completed questionnaires and wore a WD (Fitbit Alta HR®) on the same night they underwent PSG study. The data from the WD were transferred to a mobile phone and analyzed independently of PSG results, which were scored by sleep technicians. Bland-Altman plots and intraclass correlation coefficients (ICCs) were used for the analyses.
Results: Data from 55 patients (33 males, 22 females) were analyzed, with four patients excluded due to data errors. The mean differences between WD and PSG for SE (%) and light sleep were 8.4±23.8 and 43.6±26.4, respectively, both statistically significantly (p<0.05). The ICCs for SE and light sleep were -0.03 and -0.04, indicating poor reliability. However, the mean differences for TST, deep sleep, and REM sleep between the two methods were not statistically significant (p>0.05), with ICC values of 0.17, 0.16, and 0.25, respectively, all considered poor correlations.
Conclusion: In patients with sleep disorders, sleep characteristics measured by the WD and PSG showed some differences and weak correlations. As technology advances, the accuracy of wearable devices may improve. Further studies are needed to evaluate different devices and populations.
References
Practice parameters for the use of portable recording in the assessment of obstructive sleep apnea. Standards of Practice Committee of the American Sleep Disorders Association. Sleep. 1994;17:372-7.
Lee SA, Paek JH, Han SH. Sleep hygiene and its association with daytime sleepiness, depressive symptoms, and quality of life in patients with mild obstructive sleep apnea. J Neurol Sci. 2015;359:445-9.
Mehra R, Moul DE, Strohl KP. In: Kryger M, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 6th ed. Elsevier, Philadelphia; 2017.p.167-73.
Marino M, Li Y, Rueschman MN, Winkelman JW, Ellenbogen JM, Solet JM, et al. Measuring Sleep: Accuracy, Sensitivity, and Specificity of Wrist Actigraphy Compared to Polysomnography. Sleep. 2013;36:1747-55.
Martin JL, Hakim AD. Wrist actigraphy. Chest. 2011;139:1514-27.
Morgenthaler T, Alessi C, Friedman L, Owens J, Kapur V, Boehlecke B, et al. Standards of Practice Committee; American Academy of Sleep Medicine. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: an update for 2007. Sleep. 2007;30:519-29.
Evenson KR, Goto MM, Furberg RD. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int J Behav Nutr Phys Act. 2015;12:159.
de Zambotti M, Baker FC, Colrain IM. Validation of Sleep-Tracking Technology Compared with Polysomnography in Adolescents. Sleep. 2015;38:1461-8.
Cook JD, Eftekari SC, Dallmann E, Sippy M, Plante DT. Ability of the Fitbit Alta HR to quantify and classify sleep in patients with suspected central disorders of hypersomnolence: A comparison against polysomnography. J Sleep Res. 2018;28(4):e12789.
de Zambotti M, Claudatos S, Inkelis S, Colrain IM, Baker FC. Evaluation of a consumer fitness-tracking device to assess sleep in adults. Chronobiol Int. 2015;32:1024-8.
Cook JD, Prairie ML, Plante DT. Ability of the Multisensory Jawbone UP3 to Quantify and Classify Sleep in Patients With Suspected Central Disorders of Hypersomnolence: A Comparison Against Polysomnography and Actigraphy. J Clin Sleep Med. 2018;14:841-8.
Lee HA, Lee HJ, Moon JH, Lee T, Kim MG, In H, et al. Comparison of Wearable Activity Tracker with Actigraphy for Sleep Evaluation and Circadian Rest-Activity Rhythm Measurement in Healthy Young Adults. Psychiatry Investig. 2017;14:179-85.
Osterbauer B, Koempel AJ, Davidson Ward SL, Fisher LM, Don DM, Ver Halen J. A Comparison Study of The Fitbit Activity Monitor And PSG For Assessing Sleep Patterns And Movement In Children. J Otolaryngol Adv. 2016;1:24-35.
Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med. 2017;16:346.
de Zambotti M, Cellini N, Goldstone A, Colrain IM, Baker FC. Wearable sleep technology in clinical and research settings. Med Sci Sports Exerc [Internet]. 2019;51(7):1538-57.
Banhiran W. Characteristics and clinical presentations of patients at the Siriraj snoring clinic. Siriraj Med J [Internet]. 2020 [cited 2025 Jan 22];72(3):202-8.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2025 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














