From Cadaveric Dissection to Artificial Intelligence: A Chronological Review of Advances in Anatomy Education
DOI:
https://doi.org/10.33192/smj.v77i12.275193Keywords:
Anatomy education, Cadaveric dissection, Clinical anatomy, Medical curriculum reform, Problem-based learning (PBL), Artificial intelligence, ChatGPTAbstract
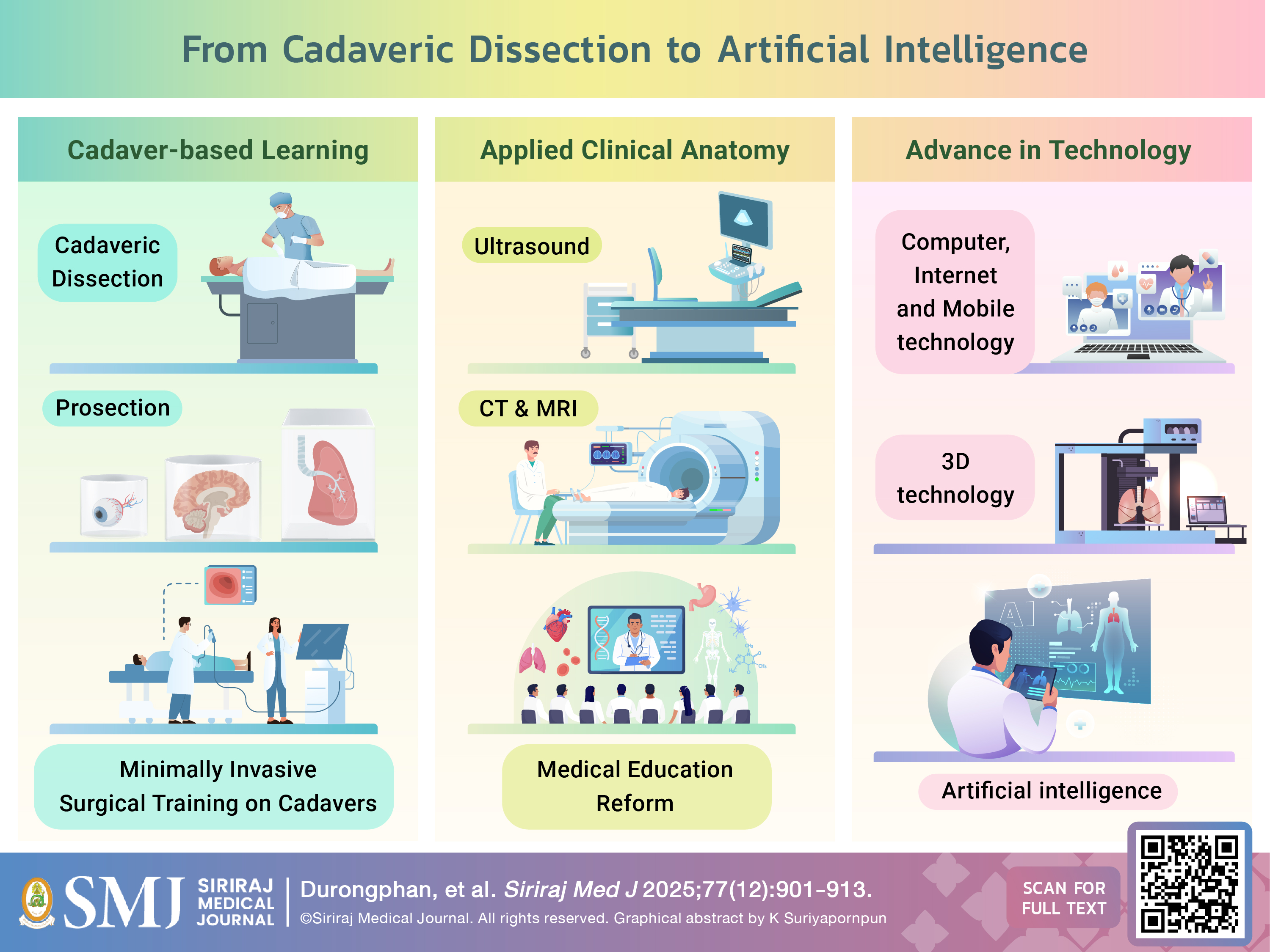
Cadaveric dissection has traditionally been the cornerstone of anatomy education. However, in recent decades, its role has come under increasing scrutiny. Comprehensive historical analyses explaining this shift remain limited. This chronologically structured review traces the evolution of anatomy teaching from its origins with Herophilus in the 3rd century BC to the advent of contemporary digital and artificial intelligence (AI)-enhanced approaches. Key milestones include the 1910 Flexner Report, which emphasized integrated biomedical sciences, widespread curricular reforms, increased reliance on prosection, the rise of minimally invasive surgery, and the incorporation of cadaveric simulation in postgraduate training. Advances in imaging technologies such as computed tomography (CT) and magnetic resonance imaging (MRI), alongside innovations in three-dimensional (3D) printing, digital dissection platforms, and virtual or augmented reality (VR/AR), have significantly reshaped anatomy instruction. Internet-based learning and mobile technologies have further transformed self-directed study through accessible, interactive resources. Most recently, AI has introduced capabilities such as personalized tutoring, performance prediction, automated assessment, and intraoperative anatomical guidance. This review highlights the value of a blended approach that integrates cadaveric experience with technological innovations. Future curricula should prioritize optimizing the sequence and combination of these modalities while ensuring equitable access and preparing students for real-world clinical challenges.
References
Garrison FH. An introduction to the history of medicine : with medical chronology, suggestions for study and bibliographic data. 4th ed. Philadelphia: W.B. Saunders; 1929. 996 p. p.
Elizondo-Omana RE, Guzman-Lopez S, Garcia-Rodriguez Mde L. Dissection as a teaching tool: past, present, and future. Anat Rec B New Anat. 2005;285(1):11-5. doi: 10.1002/ar.b.20070
Bay NS, Bay BH. Greek anatomist herophilus: the father of anatomy. Anat Cell Biol. 2010;43(4):280-3. doi: 10.5115/acb.2010.43.4.280
Standring S. A brief history of topographical anatomy. J Anat. 2016;229(1):32-62. doi: 10.1111/joa.12473
Toledo-Pereyra LH. De Humani Corporis Fabrica surgical revolution. J Invest Surg. 2008;21(5):232-6. doi: 10.1080/08941930802330830
Ghosh SK. Cadaveric dissection as an educational tool for anatomical sciences in the 21st century. Anat Sci Educ. 2017;10(3):286-99. doi: 10.1002/ase.1649
Baethge C, Goldbeck-Wood S, Mertens S. SANRA-a scale for the quality assessment of narrative review articles. Res Integr Peer Rev. 2019;4:5. doi: 10.1186/s41073-019-0064-8
Gregory AT, Denniss AR. An Introduction to Writing Narrative and Systematic Reviews - Tasks, Tips and Traps for Aspiring Authors. Heart Lung Circ. 2018;27(7):893-8. doi: 10.1016/j.hlc.2018.03.027
Toledo-Pereyra LH. Medical Renaissance. J Invest Surg. 2015;28(3):127-30. doi: 10.3109/08941939.2015.1054747
Bonnel F, Lavabre-Bertrand T, Bonnel C. The teaching of anatomy in Montpellier University during VIII centuries (1220-2020). Surg Radiol Anat. 2019;41(10):1119-28. doi: 10.1007/s00276-019-02289-6
Gelfand T. The "Paris manner" of dissection: student anatomical dissection in early eighteenth-century Paris. Bull Hist Med. 1972;46(2):99-130.
Flexner A. Medical education in the United States and Canada. From the Carnegie Foundation for the Advancement of Teaching, Bulletin Number Four, 1910. Bull World Health Organ. 2002;80(7):594-602.
Ratanayotha A, Oo EM. Chronicle of Anatomical Education in Thailand: Experiences at Siriraj Medical School. Siriraj Med J. 2022;74(7):463-71. doi: 10.33192/Smj.2022.55
Sinha SR, Entezampour M, Davis K, Vyas RM. Clinically Applied Anatomy: An Impactful Initiative in the Evolution of Medical Education. Ann Plast Surg. 2020;84(5):476-80. doi: 10.1097/SAP.0000000000002216
Kim IB, Joo KM, Song CH, Rhyu IJ. A Brief Review of Anatomy Education in Korea, Encompassing Its Past, Present, and Future Direction. J Korean Med Sci. 2024;39(20):e159. doi: 10.3346/jkms.2024.39.e159
Gabriel AG, Chia SL. High Price of Perfection that Is Anatomy: Why Studying and Teaching the Human Body Is a Financial Muscle. Journal of Innovations in Medical Research. 2025;4(2):84-8. doi: 10.63593/JIMR.2788-7022.2025.04.010
Jayakumar N, Athar S, Ashwood N. Where do these cadavers come from? Clin Anat. 2020;33(6):872-5. doi: 10.1002/ca.23570
Anatomists IFoAo. Recommendations of good practice for the donation and study of human bodies and tissues for anatomical examination 2012 [cited 2025 July 1]. Available from: https://ifaa.net/wp-content/uploads/2017/09/IFAA-guidelines-220811.pdf.
Chen D, Zhang Q, Deng J, Cai Y, Huang J, Li F, et al. A shortage of cadavers: The predicament of regional anatomy education in mainland China. Anat Sci Educ. 2018;11(4):397-402. doi: 10.1002/ase.1788
Zdilla MJ, Balta JY. Human body donation and surgical training: a narrative review with global perspectives. Anat Sci Int. 2023;98(1):1-11. doi: 10.1007/s12565-022-00689-0
Durongphan A, Amornmettajit N, Rungruang J, Nitimanee E, Panichareon B. One academic year laboratory and student breathing zone formaldehyde level, measured by gas-piston hand pump at gross anatomy laboratory, Siriraj Hospital, Thailand. Environ Sci Pollut Res Int. 2020;27(14):16521-7. doi: 10.1007/s11356-020-08199-0
Durongphan A, Chongkolwatana W, Ngamskulrungroj P, Pochnasomboon T, Pinkaew J, Pamornpol B, et al. A Pilot Comparative Study of Submerge vs. Non-Submerg Saturated Salt Solution Human Cadavers Embalming Method by Gross, Histological, and Microbiological Evaluation. Siriraj Med J. 2022;74(7):431-9. doi: 10.33192/Smj.2022.52
Smith CF, Freeman SK, Heylings D, Finn GM, Davies DC. Anatomy education for medical students in the United Kingdom and Republic of Ireland in 2019: A 20-year follow-up. Anat Sci Educ. 2022;15(6):993-1006. doi: 10.1002/ase.2126
Peter SDS, Holcomb III GW. History of minimally invasive surgery: Philadelphia: Elsevier Health Sciences; 2008.
Jani K, Rajan PS, Sendhilkumar K, Palanivelu C. Twenty years after Erich Muhe: Persisting controversies with the gold standard of laparoscopic cholecystectomy. J Minim Access Surg. 2006;2(2):49-58. doi: 10.4103/0972-9941.26646
Memon I. Cadaver Dissection Is Obsolete in Medical Training! A Misinterpreted Notion. Med Princ Pract. 2018;27(3):201-10. doi: 10.1159/000488320
Anastakis DJ, Regehr G, Reznick RK, Cusimano M, Murnaghan J, Brown M, et al. Assessment of technical skills transfer from the bench training model to the human model. Am J Surg. 1999;177(2):167-70. doi: 10.1016/s0002-9610(98)00327-4
Lewis CE, Peacock WJ, Tillou A, Hines OJ, Hiatt JR. A novel cadaver-based educational program in general surgery training. J Surg Educ. 2012;69(6):693-8. doi: 10.1016/j.jsurg.2012.06.013
Gasco J, Holbrook TJ, Patel A, Smith A, Paulson D, Muns A, et al. Neurosurgery simulation in residency training: feasibility, cost, and educational benefit. Neurosurgery. 2013;73 Suppl 1:39-45. doi: 10.1227/NEU.0000000000000102
Kim SC, Fisher JG, Delman KA, Hinman JM, Srinivasan JK. Cadaver-Based Simulation Increases Resident Confidence, Initial Exposure to Fundamental Techniques, and May Augment Operative Autonomy. J Surg Educ. 2016;73(6):e33-e41. doi: 10.1016/j.jsurg.2016.06.014
Camp CL, Krych AJ, Stuart MJ, Regnier TD, Mills KM, Turner NS. Improving Resident Performance in Knee Arthroscopy: A Prospective Value Assessment of Simulators and Cadaveric Skills Laboratories. J Bone Joint Surg Am. 2016;98(3):220-5. doi: 10.2106/JBJS.O.00440
Farah GJ, Rogers JL, Lopez AM, Brown NJ, Pennington Z, Kuo C, et al. Resident Training in Spine Surgery: A Systematic Review of Simulation-Based Educational Models. World Neurosurg. 2023;174:81-115. doi: 10.1016/j.wneu.2023.03.032
London IC. London School of Surgery Training Programme 2023 [cited 2025 Jun. 23]. Available from: https://www.imperial.ac.uk/medicine/research-and-impact/facilities/london-school-of-surgery-training-programme/training-and-assessment/ear-nose--throat-surgical-training/.
University HMS. Didactic Curriculum in Otolaryngology–Head and Neck Surgery 2023 [cited 2025 Jun. 23]. Available from: https://oto.hms.harvard.edu/didactic-curriculum-otolaryngology.
University GSM. Curriculum 2023 [cited 2025 Jun. 23]. Available from: https://graduate.mahidol.ac.th/inter/prospective-students/?p=curriculum&id=2035N03G.
Estai M, Bunt S. Best teaching practices in anatomy education: A critical review. Ann Anat. 2016;208:151-7. doi: 10.1016/j.aanat.2016.02.010
Mitchell PD, Boston C, Chamberlain AT, Chaplin S, Chauhan V, Evans J, et al. The study of anatomy in England from 1700 to the early 20th century. J Anat. 2011;219(2):91-9. doi: 10.1111/j.1469-7580.2011.01381.x
Roth H, Smith RA, Mackay S. Modern day relevance of William Hunter's approach to teaching "The organ of hearing". Clin Anat. 2013;26(5):551-5. doi: 10.1002/ca.22220
Sinclair DC. An Experiment in the Teaching of Anatomy. 1965 May. Report No.: 0022-2577 (Print) 0022-2577 (Linking).
Koh ZJ, Yeow M, Srinivasan DK, Ng YK, Ponnamperuma GG, Chong CS. A randomized trial comparing cadaveric dissection and examination of prosections as applied surgical anatomy teaching pedagogies. Anat Sci Educ. 2023;16(1):57-70. doi: 10.1002/ase.2166
Abdellatif H. Time Spent in Practicing Dissection Correlated with Improvement in Anatomical Knowledge of Students: Experimental Study in an Integrated Learning Program. Cureus. 2020;12(4):e7558. doi: 10.7759/cureus.7558
Wilson AB, Miller CH, Klein BA, Taylor MA, Goodwin M, Boyle EK, et al. A meta-analysis of anatomy laboratory pedagogies. Clin Anat. 2018;31(1):122-33. doi: 10.1002/ca.22934
Clayton M. Leonardo da Vinci as an anatomist 2001. Available from: https://media.rct.uk/sites/default/files/file-downloads/Leonardo%20da%20Vinci%20Anatomist.pdf?_ga=2.35543076.461267984.1751959990-560325555.1751959990.
Martin C, Philo R. Leonardo da Vinci : the mechanics of man. London
Los Angeles: Royal Collection Enterprises ; J. Paul Getty Museum; 2010. 160 p. p.
McLachlan JC, Patten D. Anatomy teaching: ghosts of the past, present and future. Med Educ. 2006;40(3):243-53. doi: 10.1111/j.1365-2929.2006.02401.x
Op Den Akker JW, Bohnen A, Oudegeest WJ, Hillen B. Giving color to a new curriculum: bodypaint as a tool in medical education. Clin Anat. 2002;15(5):356-62. doi: 10.1002/ca.10049
Bergman EM, Sieben JM, Smailbegovic I, de Bruin AB, Scherpbier AJ, van der Vleuten CP. Constructive, collaborative, contextual, and self-directed learning in surface anatomy education. Anat Sci Educ. 2013;6(2):114-24. doi: 10.1002/ase.1306
Teichgraber UK, Meyer JM, Poulsen Nautrup C, von Rautenfeld DB. Ultrasound anatomy: a practical teaching system in human gross anatomy. Med Educ. 1996;30(4):296-8. doi: 10.1111/j.1365-2923.1996.tb00832.x
Swamy M, Searle RF. Anatomy teaching with portable ultrasound to medical students. BMC Med Educ. 2012;12:99. doi: 10.1186/1472-6920-12-99
So S, Patel RM, Orebaugh SL. Ultrasound imaging in medical student education: Impact on learning anatomy and physical diagnosis. Anat Sci Educ. 2017;10(2):176-89. doi: 10.1002/ase.1630
Griksaitis MJ, Sawdon MA, Finn GM. Ultrasound and cadaveric prosections as methods for teaching cardiac anatomy: a comparative study. Anat Sci Educ. 2012;5(1):20-6. doi: 10.1002/ase.259
Wittich CM, Montgomery SC, Neben MA, Palmer BA, Callahan MJ, Seward JB, et al. Teaching cardiovascular anatomy to medical students by using a handheld ultrasound device. JAMA. 2002;288(9):1062-3. doi: 10.1001/jama.288.9.1062
Haidar DA, Kessler R, Khanna NK, Cover MT, Burkhardt JC, Theyyunni N, et al. Association of a longitudinal, preclinical ultrasound curriculum with medical student performance. BMC Med Educ. 2022;22(1):50. doi: 10.1186/s12909-022-03108-0
Johnson CD, Davison L, Graham EC, Sweeney EM. Ultrasound technology as a tool to teach basic concepts of physiology and anatomy in undergraduate and graduate courses: a systematic review. Adv Physiol Educ. 2025;49(1):11-26. doi: 10.1152/advan.00199.2023
Bradley WG. History of medical imaging. Proc Am Philos Soc. 2008;152(3):349-61.
Rontgen WC. On a New Kind of Rays. Science. 1896;3(59):227-31. doi: 10.1126/science.3.59.227
Mould RF. The discovery of radium in 1898 by Maria Sklodowska-Curie (1867-1934) and Pierre Curie (1859-1906) with commentary on their life and times. Br J Radiol. 1998;71(852):1229-54. doi: 10.1259/bjr.71.852.10318996
Schulz RA, Stein JA, Pelc NJ. How CT happened: the early development of medical computed tomography. J Med Imaging (Bellingham). 2021;8(5):052110. doi: 10.1117/1.JMI.8.5.052110
Geva T. Magnetic resonance imaging: historical perspective. J Cardiovasc Magn Reson. 2006;8(4):573-80. doi: 10.1080/10976640600755302
Hamilton JD. The McMaster curriculum: a critique. Br Med J. 1976;1(6019):1191-6. doi: 10.1136/bmj.1.6019.1191
Erkonen WE, Albanese MA, Smith WL, Pantazis NJ. Gross anatomy instruction with diagnostic images. Invest Radiol. 1990;25(3):292-4. doi: 10.1097/00004424-199003000-00018
Erkonen WE, Albanese MA, Smith WL, Pantazis NJ. Effectiveness of teaching radiologic image interpretation in gross anatomy. A long-term follow-up. Invest Radiol. 1992;27(3):264-6. doi: 10.1097/00004424-199203000-00016
Chew C, O’Dwyer P, Young D, Gracie J. Radiology teaching improves anatomy scores for medical students. The British Journal of Radiology. 2020;93(1114):20200463. doi: 10.1259/bjr.20200463
Larsen RJ, Engle DL. The impact of a radiological anatomy-based intervention in a gross anatomy course for undergraduate medical students. Education in the Health Professions. 2020;3(2):47-53. doi: 10.4103/EHP.EHP_19_20
Merseth KK. The Early History of Case-Based Instruction: Insights for Teacher Education Today. Journal of Teacher Education.42(4):4. doi: 10.1177/002248719104200402
School HL. The Case Study Teaching Method [cited 2025 Jun. 23]. Available from: https://casestudies.law.harvard.edu/the-case-study-teaching-method/#:~:text=The%20case%20method%20in%20legal,that%20furthered%20principles%20or%20doctrines.
Normand Y. THE HISTORY OF THE CASE STUDY AT HARVARD BUSINESS SCHOOL: Harvard Business School Online; [cited 2025 Jun. 23]. Available from: https://online.hbs.edu/blog/post/the-history-of-the-case-study-at-harvard-business-school.
School HB. CASE METHOD 100 YEARS: Harvard Business School; [cited 2025 Jun. 23]. Available from: https://www.hbs.edu/case-method-100.
W. B. CANNON AM. The Case Method of Teaching Systematic Medicine. Boston Medical and Surgical Journal. 1900(142):4. doi: 10.1056/nejm190001111420202
The Case System in Medical Teaching Boston Medical and Surgical Journal. 1906;155:2. doi: 10.1056/NEJM190607121550219
Neufeld VR, Barrows HS. The "McMaster Philosophy": an approach to medical education. J Med Educ. 1974;49(11):1040-50. doi:
Tosteson DC. New pathways in general medical education. N Engl J Med. 1990;322(4):234-8. doi: 10.1056/NEJM199001253220405
Gijbels D, Dochy F, Van den Bossche P, Segers M. Effects of problem-based learning: A meta-analysis from the angle of assessment. Review of educational research. 2005;75(1):27-61. doi: 10.3102/00346543075001027
Hartling L, Spooner C, Tjosvold L, Oswald A. Problem-based learning in pre-clinical medical education: 22 years of outcome research. Med Teach. 2010;32(1):28-35. doi: 10.3109/01421590903200789
Trullas JC, Blay C, Sarri E, Pujol R. Effectiveness of problem-based learning methodology in undergraduate medical education: a scoping review. BMC Med Educ. 2022;22(1):104. doi: 10.1186/s12909-022-03154-8
Hinduja K, Samuel R, Mitchell S. Problem-based learning: is anatomy a casualty? Surgeon. 2005;3(2):84-7. doi: 10.1016/s1479-666x(05)80067-8
Williams JM. Is Student Knowledge of Anatomy Affected by a Problem-Based Learning Approach? A Review. Journal of Education and Training Studies. 2014;2(4):108-12. doi: https://doi.org/10.11114/jets.v2i4.509
Louw G, Eizenberg N, Carmichael SW. The place of anatomy in medical education: AMEE Guide no 41. Med Teach. 2009;31(5):373-86. doi: 10.1080/01421590902825149
Parmelee D, Roman B, Overman I, Alizadeh M. The lecture-free curriculum: Setting the stage for life-long learning: AMEE Guide No. 135. Med Teach. 2020;42(9):962-9. doi: 10.1080/0142159X.2020.1789083
MacNeill H, Masters K, Nemethy K, Correia R. Online learning in Health Professions Education. Part 1: Teaching and learning in online environments: AMEE Guide No. 161. Med Teach. 2024;46(1):4-17. doi: 10.1080/0142159X.2023.2197135
JP B. Alan Turing: Founder of Computer Science. Engineering Trustworthy Software Systems. 2017. doi: 10.1007/978-3-319-56841-6_1
Copeland BJ. The modern history of computing: Stanford University; 2006 [Available from: https://plato.stanford.edu/entries/computing-history/#ACE
Turing AM. Computing machinery and intelligence. Mind. 1950; LIX( 236):433–60. doi: 10.1093/oso/9780198250791.003.0017
Carpenter BE, Doran R. AM Turing's ACE report of 1946 and other papers. Massachusetts Institute of Technology; 1986. Report No.: 0262031140.
Aspray W. The Intel 4004 microprocessor: What constituted invention? IEEE Annals of the History of Computing. 1997;19(3):4–15. doi: 10.1109/85.601727
Batson E. Apple IIe and IBM PC. Comparison of America's most popular personal computers. Postgrad Med. 1984;75(5):279-82. doi: 10.1080/00325481.1984.11698007
Ackerman MJ. The Visible Human Project. Inf Serv Use. 2022;42(1):129-36. doi: 10.3233/ISU-210145
Ackerman MJ. The Visible Human Project: a resource for education. Acad Med. 1999;74(6):667-70. doi: 10.1097/00001888-199906000-00012
Rowe PM. Visible Human Project pays back investment. Lancet. 1999;353(9146):46. doi: 10.1016/S0140-6736(05)74857-1
Adnan S, Benson AC, Xiao J. How virtual reality is being adopted in anatomy education in health sciences and allied health: A systematic review. Anat Sci Educ. 2025;18(5):496-525. doi: 10.1002/ase.70027
García‐Robles P, Cortés‐Pérez I, Nieto‐Escámez FA, García‐López H, Obrero‐Gaitán E, Osuna‐Pérez MC. Immersive virtual reality and augmented reality in anatomy education: a systematic review and Meta‐Analysis. Anatomical Sciences Education. 2024;17(3):514-28. doi: 10.1002/ase.2397
Bolek KA, De Jong G, Henssen D. The effectiveness of the use of augmented reality in anatomy education: a systematic review and meta-analysis. Sci Rep. 2021;11(1):15292. doi: 10.1038/s41598-021-94721-4
Bank W. World Bank Country and Lending Groups Washington, DC: World Bank; 2025 [cited 2025 July 3]. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
Al'Aref SJ. 3D printing applications in cardiovascular medicine.
Crump SS, inventorApparatus and method for creating three-dimensional objects. 19921989.
McGurk M, Amis AA, Potamianos P, Goodger NM. Rapid prototyping techniques for anatomical modelling in medicine. Ann R Coll Surg Engl. 1997;79(3):169-74. doi:
Chen S, Pan Z, Wu Y, Gu Z, Li M, Liang Z, et al. The role of three-dimensional printed models of skull in anatomy education: a randomized controlled trail. Sci Rep. 2017;7(1):575. doi: 10.1038/s41598-017-00647-1
Lim KH, Loo ZY, Goldie SJ, Adams JW, McMenamin PG. Use of 3D printed models in medical education: A randomized control trial comparing 3D prints versus cadaveric materials for learning external cardiac anatomy. Anat Sci Educ. 2016;9(3):213-21. doi: 10.1002/ase.1573
Cai B, Rajendran K, Bay BH, Lee J, Yen CC. The Effects of a Functional Three-dimensional (3D) Printed Knee Joint Simulator in Improving Anatomical Spatial Knowledge. Anat Sci Educ. 2019;12(6):610-8. doi: 10.1002/ase.1847
Ye Z, Dun A, Jiang H, Nie C, Zhao S, Wang T, et al. The role of 3D printed models in the teaching of human anatomy: a systematic review and meta-analysis. BMC medical education. 2020;20:1-9. doi: 10.1186/s12909-020-02242-x
Blohm JE, Salinas PA, Avila MJ, Barber SR, Weinand ME, Dumont TM. Three-Dimensional Printing in Neurosurgery Residency Training: A Systematic Review of the Literature. World Neurosurg. 2022;161:111-22. doi: 10.1016/j.wneu.2021.10.069
VanKoevering KK, Hollister SJ, Green GE. Advances in 3-Dimensional Printing in Otolaryngology: A Review. JAMA Otolaryngol Head Neck Surg. 2017;143(2):178-83. doi: 10.1001/jamaoto.2016.3002
Raees S, Ullah F, Javed F, Akil HM, Jadoon Khan M, Safdar M, et al. Classification, processing, and applications of bioink and 3D bioprinting: A detailed review. Int J Biol Macromol. 2023;232:123476. doi: 10.1016/j.ijbiomac.2023.123476
Michael H. Behind the net: the untold history of the ARPANET and computer science 2006 [cited 2025 Jun. 23]. Available from: https://www.columbia.edu/~hauben/book-pdf/CHAPTER%207.pdf.
Brinkley JF, Bradley SW, Sundsten JW, Rosse C. The digital anatomist information system and its use in the generation and delivery of Web-based anatomy atlases. Comput Biomed Res. 1997;30(6):472-503. doi: 10.1006/cbmr.1997.1461
Goggin G. Google phone rising: The Android and the politics of open source. Continuum. 2012;26(5):741-52. doi: https://doi.org/10.1080/10304312.2012.706462
West J, Mace M. Browsing as the killer app: Explaining the rapid success of Apple's iPhone. Telecommunications Policy. 2010;34(5-6):270-86. doi: 10.1016/j.telpol.2009.12.002
George P, Dumenco L, Dollase R, Taylor JS, Wald HS, Reis SP. Introducing technology into medical education: two pilot studies. Patient education and counseling. 2013;93(3):522-4. doi: 10.1016/j.pec.2013.04.018
Choi-Lundberg DL, Low TF, Patman P, Turner P, Sinha SN. Medical student preferences for self-directed study resources in gross anatomy. Anat Sci Educ. 2016;9(2):150-60. doi: 10.1002/ase.1549
Leung BC, Williams M, Horton C, Cosker TD. Modernising Anatomy Teaching: Which Resources Do Students Rely On? J Med Educ Curric Dev. 2020;7:2382120520955156. doi: 10.1177/2382120520955156
Jaffar AA. YouTube: An emerging tool in anatomy education. Anat Sci Educ. 2012;5(3):158-64. doi: 10.1002/ase.1268
Lasker R, Vicneswararajah N. Using Twitter to teach problem-based learning. Med Educ. 2015;49(5):531. doi: 10.1111/medu.12717
Chytas D. Use of social media in anatomy education: A narrative review of the literature. Ann Anat. 2019;221:165-72. doi: 10.1016/j.aanat.2018.10.004
Joseph MA, Natarajan J, Al Zaabi O, Sirasanagandla SR. Instagram Reels improve students' knowledge, motivation, perception, and satisfaction with anatomy and physiology. Anat Sci Educ. 2025;18(6):533-43. doi: 10.1002/ase.70039
Pather N, Blyth P, Chapman JA, Dayal MR, Flack N, Fogg QA, et al. Forced Disruption of Anatomy Education in Australia and New Zealand: An Acute Response to the Covid-19 Pandemic. Anat Sci Educ. 2020;13(3):284-300. doi: 10.1002/ase.1968
Harmon DJ, Attardi SM, Barremkala M, Bentley DC, Brown KM, Dennis JF, et al. An Analysis of Anatomy Education Before and During Covid-19: May-August 2020. Anat Sci Educ. 2021;14(2):132-47. doi: 10.1002/ase.2051
Natsis K, Lazaridis N, Kostares M, Anastasopoulos N, Chytas D, Totlis T, et al. "Dissection Educational Videos" (DEVs) and their contribution in anatomy education: a students' perspective. Surg Radiol Anat. 2022;44(1):33-40. doi: 10.1007/s00276-021-02829-z
Pelchen L. Internet usage statistics in 2024 Forbes Magazine; 2024 [updated Mar 1, 2024; cited 2025 Jun. 23]. Available from: https://www.forbes.com/home-improvement/internet/internet-statistics.
Pettersson A, Karlgren K, Hjelmqvist H, Meister B, Silen C. An exploration of students' use of digital resources for self-study in anatomy: a survey study. BMC Med Educ. 2024;24(1):45. doi: 10.1186/s12909-023-04987-7
Ertel W. Introduction to artificial intelligence: Springer; 2018.
Ramesh AN, Kambhampati C, Monson JR, Drew PJ. Artificial intelligence in medicine. Ann R Coll Surg Engl. 2004;86(5):334-8. doi: 10.1308/147870804290
Nagendran M, Chen Y, Lovejoy CA, Gordon AC, Komorowski M, Harvey H, et al. Artificial intelligence versus clinicians: systematic review of design, reporting standards, and claims of deep learning studies. BMJ. 2020;368:m689. doi: 10.1136/bmj.m689
Loftus TJ, Tighe PJ, Filiberto AC, Efron PA, Brakenridge SC, Mohr AM, et al. Artificial Intelligence and Surgical Decision-making. JAMA Surg. 2020;155(2):148-58. doi: 10.1001/jamasurg.2019.4917
Madani A, Namazi B, Altieri MS, Hashimoto DA, Rivera AM, Pucher PH, et al. Artificial Intelligence for Intraoperative Guidance: Using Semantic Segmentation to Identify Surgical Anatomy During Laparoscopic Cholecystectomy. Ann Surg. 2022;276(2):363-9. doi: 10.1097/SLA.0000000000004594
Sahni NR, Carrus B. Artificial Intelligence in U.S. Health Care Delivery. N Engl J Med. 2023;389(4):348-58. doi: 10.1056/NEJMra2204673
Solaphat H, Kittipoch S, Pasit J, Chanyanart K-O, Kantapat C, Arisara A, et al. Development and evaluation of the DMIND questionnaire: Preparing for AI integration into an effective depression screening tool. Siriraj Med J. 2024;76(9):620-9. doi: 10.33192/smj.v76i9.269527
Sa-ngiamwibool P, Laohawetwanit T. Comparative Analysis of ChatGPT and Human Expertise in Diagnosing Primary Liver Carcinoma: A Focus on Gross Morphology. Siriraj Med J. 2025;77(2):119-29. doi: 10.33192/smj.v77i2.271596
OpenAI. ChatGPT San Francisco, CA: OpenAI; 2022 [cited 2025 Jun. 23]. Available from: https://openai.com/index/chatgpt/.
Khan N, Khan Z, Koubaa A, Khan MK, Salleh RB. Global insights and the impact of generative AI-ChatGPT on multidisciplinary: a systematic review and bibliometric analysis. Connection Science. 2024;36(1):2353630. doi: https://doi.org/10.1080/09540091.2024.2353630
Li YS, Lam CSN, See C. Using a Machine Learning Architecture to Create an AI-Powered Chatbot for Anatomy Education. Med Sci Educ. 2021;31(6):1729-30. doi: 10.1007/s40670-021-01405-9
Fries A, Pirotte M, Vanhee L, Bonnet P, Quatresooz P, Debruyne C, et al. Validating instructional design and predicting student performance in histology education: Using machine learning via virtual microscopy. Anat Sci Educ. 2024;17(5):984-97. doi: 10.1002/ase.2346
Bernard J, Sonnadara R, Saraco AN, Mitchell JP, Bak AB, Bayer I, et al. Automated grading of anatomical objective structured practical examinations using decision trees: An artificial intelligence approach. Anat Sci Educ. 2024;17(5):967-78. doi: 10.1002/ase.2305
Rechowicz KJ, Elzie CA. The use of artificial intelligence to detect students' sentiments and emotions in gross anatomy reflections. Anat Sci Educ. 2024;17(5):954-66. doi: 10.1002/ase.2273
Google. Gemini Deep Research: Google; 2025 [cited 2025 July 3]. Available from: https://gemini.google/overview/deep-research/?hl=en.
OpenAI. Introducing GPT-4.1 in the API: OpenAI; 2025 [updated 2025 April 14; cited 2025 July 3]. Available from: https://openai.com/index/gpt-4-1/?utm_source=chatgpt.com.
Team P. Introducing Perplexity Deep Research 2025 [cited 2025 July 3]. Available from: https://www.perplexity.ai/hub/blog/introducing-perplexity-deep-research.
Aljamaan F, Temsah MH, Altamimi I, Al-Eyadhy A, Jamal A, Alhasan K, et al. Reference Hallucination Score for Medical Artificial Intelligence Chatbots: Development and Usability Study. JMIR Med Inform. 2024;12:e54345. doi: 10.2196/54345
Colasacco CJ, Born HL. A Case of Artificial Intelligence Chatbot Hallucination. JAMA Otolaryngol Head Neck Surg. 2024;150(6):457-8. doi: 10.1001/jamaoto.2024.0428
Yu KH, Healey E, Leong TY, Kohane IS, Manrai AK. Medical Artificial Intelligence and Human Values. N Engl J Med. 2024;390(20):1895-904. doi: 10.1056/NEJMra2214183
Howell MD, Corrado GS, DeSalvo KB. Three Epochs of Artificial Intelligence in Health Care. JAMA. 2024;331(3):242-4. doi: 10.1001/jama.2023.25057
Van Booven D, Cheng-Bang C, Meenakshy M. Limitations of artificial intelligence in healthcare. Artificial Intelligence in Urologic Malignancies: Elsevier; 2025. p. 231-46.
Khalifa M, Albadawy M. Using artificial intelligence in academic writing and research: An essential productivity tool. Computer Methods and Programs in Biomedicine Update. 2024:100145. doi: 10.1016/j.cmpbup.2024.100145
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2025 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














