Factors Predicting Postoperative Quality of Life among Rectal Cancer Patients in Thailand: A Retrospective Cohort Study
DOI:
https://doi.org/10.33192/smj.v77i8.276010Keywords:
Quality of life, rectal cancer, FACT-C, Multiple regressionAbstract
Objective: The objectives of this study were to evaluate the postoperative quality of life (QoL) measures of Thai rectal cancer patients and to determine which factors impact the QoL.
Materials and Methods: We reviewed the medical records of rectal cancer patients who underwent abdominoperineal resection or low anterior resection between 2009 and 2012. We sent out Functional Assessment of Cancer Therapy – Colorectal (FACT-C) questionnaires to patients who met the criteria. The T-test, Kendall’s Tau-b, and Pearson correlation were used to select potentially significant predictors (p-value <0.1), which were then included in the multiple regression analysis to predict FACT-G (General QoL) and FACT-C (General QoL + concerns related to colorectal cancer) scores.
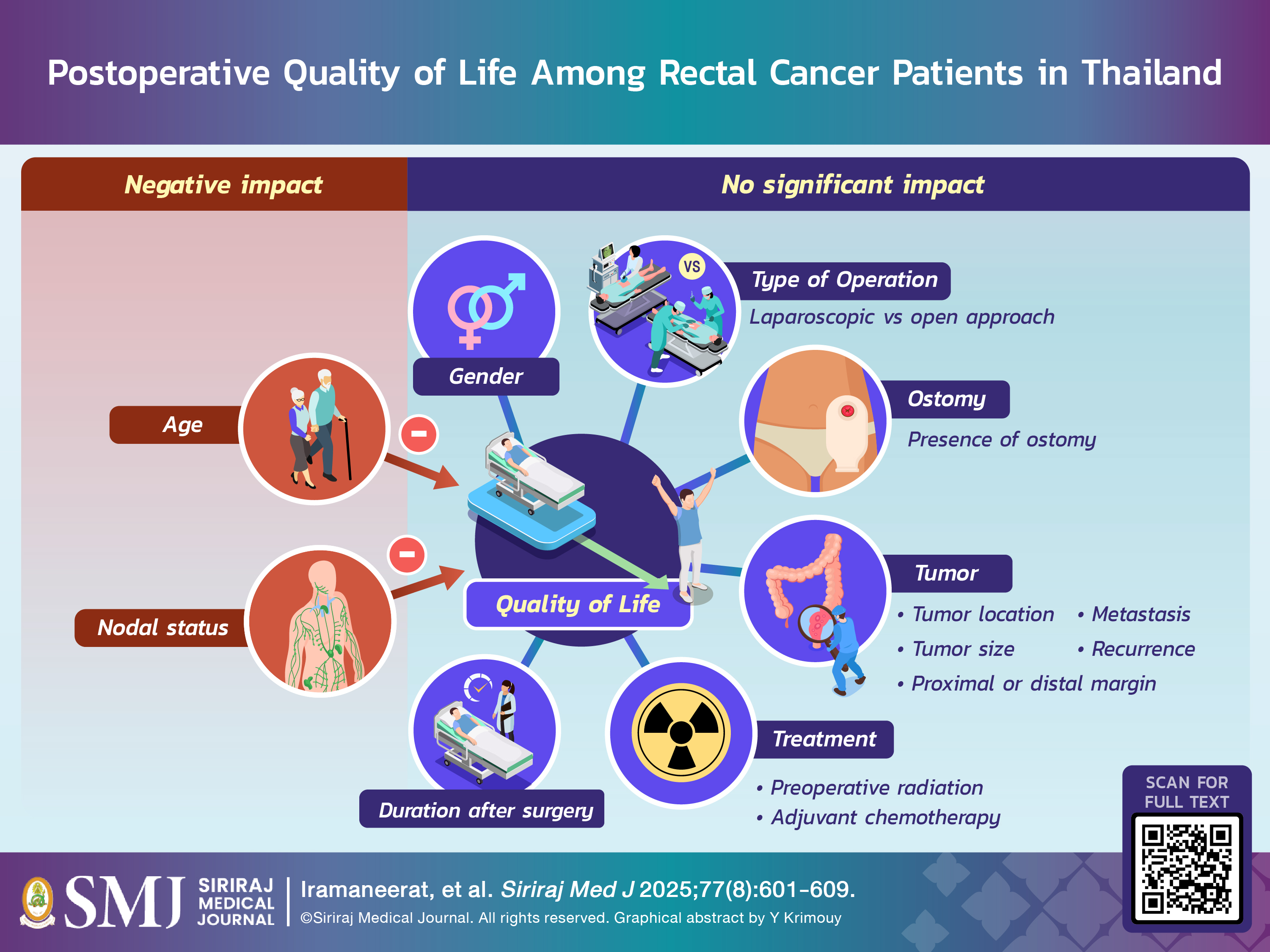
Results: We analyzed data from 144 patients (out of 480 patients who met the criteria). The average FACT-G and FACT-C scores were 87.34 and 106.79, respectively. The factor that had a significant negative impact on FACT-G was age (t = -2.67, p = 0.008). The factors that had a significant negative impact on FACT-C were nodal status (t = -1.98, p = 0.05) and age (t = -2.66, p = 0.009).
Conclusion: The postoperative QoL of Thai rectal cancer patients is similar to the QoL measures reported in a prior study. The QoL measures were found to be negatively impacted by age and lymph node status. Gender, the type of operation, presence of ostomy, location of the tumor, preoperative radiation, adjuvant chemotherapy, laparoscopic approach, duration after surgery, proximal and distal margins, tumor size, metastasis, and recurrence showed no impact on the QoL.
References
National Cancer Institute of Thailand. Hospital-based cancer registry 2019. Rachathewi, Bangkok: National Cancer Institute, Thailand, 2020.
Lohsiriwat V, Chaisomboon N, Pattana-Arun J. Current Colorectal Cancer in Thailand. Ann Coloproctol. 2020;36(2):78-82.
Camilleri-Brennan J, Steele RJ. Quality of life after treatment for rectal cancer. Br J Surg. 1998;85(8):1036-43.
Campitelli M, Dinapoli L. How to Track the Quality of Life in Rectal Cancer Patients? In: Valentini V, Schmoll H-J, van de Velde CJH, eds. Multidisciplinary Management of Rectal Cancer: Questions and Answers. Cham: Springer; 2018.p.615-22.
Cooperative clinical investigators of the Dutch Total Mesorectal Excision trial. Risk factors for faecal incontinence after rectal cancer treatment. Br J Surg. 2007;94(10):1278-84.
Li X, Song X, Chen Z, Li M, Lu L, Xu Y, et al. Quality of life in rectal cancer patients after radical surgery: a survey of Chinese patients. World J Surg Oncol. 2014;12:161.
Engel J, Kerr J, Schlesinger-Raab A, Eckel R, Sauer H, Hölzel D. Quality of life in rectal cancer patients: a four-year prospective study. Ann Surg. 2003;238(2):203-13.
Campos-Lobato LFd, Alves-Ferreira PC, Lavery IC, Kiran RP. Abdominoperineal resection does not decrease quality of life in patients with low rectal cancer. Clinics (Sao Paulo). 2011;66(6):1035-40.
Smith-Gagen J, Cress RD, Drake CM, Romano PS, Yost KJ, Ayanian JZ. Quality-of-life and surgical treatments for rectal cancer—A longitudinal analysis using the California Cancer Registry. Psycho-Oncology. 2010;19(8):870-8.
Cornish JA, Tilney HS, Heriot AG, Lavery IC, Fazio VW, Tekkis PP. A meta-analysis of quality of life for abdominoperineal excision of rectum versus anterior resection for rectal cancer. Ann Surg Oncol. 2007;14(7):2056-68.
Pachler J, Wille-Jørgensen P. Quality of life after rectal resection for cancer, with or without permanent colostomy. Cochrane Database Syst Rev. 2004;(3):CD004323.
Campelo P, Barbosa E. Functional outcome and quality of life following treatment for rectal cancer. J Coloproctology. 2016;36(4):251-61.
França Neto PR, Queiroz FLd, Staino IRFL, Lacerda Filho A. Quality of life assessment in the late postoperative period of patients with rectal cancer submitted to total mesorectal excision. J Coloproctology. 2013;33:50-7.
Chutikamo N, Navicharern R, Lohsiriwat V. Comparative study of health-related quality of life between colorectal cancer patients with temporary and permanent stoma. Siriraj Med J. 2019;71:196-200.
McNair AG, Whistance RN, Forsythe RO, Rees J, Jones JE, Pullyblank AM, et al. Synthesis and summary of patient-reported outcome measures to inform the development of a core outcome set in colorectal cancer surgery. Colorectal Dis. 2015;17(11):O217-29.
Ward WL, Hahn EA, Mo F, Hernandez L, Tulsky DS, Cella D. Reliability and validity of the Functional Assessment of Cancer Therapy-Colorectal (FACT-C) quality of life instrument. Qual Life Res. 1999;8(3):181-95.
Ganesh V, Agarwal A, Popovic M, Cella D, McDonald R, Vuong S, et al. Comparison of the FACT-C, EORTC QLQ-CR38, and QLQ-CR29 quality of life questionnaires for patients with colorectal cancer: a literature review. Supportive Care Cancer 2016;24(8):3661-8.
Thongdeebut T, Danaidutsadeekul S, Phligbua W, Lohsiriwat V. Impact of social determinants of health on postoperative health-related quality of life among patients undergoing colorectal cancer surgery. Siriraj Med J. 2025;77(5):331-41.
Yost KJ, Cella D, Chawla A, Holmgren E, Eton DT, Ayanian JZ, et al. Minimally important differences were estimated for the Functional Assessment of Cancer Therapy-Colorectal (FACT-C) instrument using a combination of distribution- and anchor-based approaches. J Clin Epidemiol. 2005;58(12):1241-51.
Lohsiriwat V, Rungteeranont C, Saigosoom N. Incidence and pattern of nodal metastasis in colon and rectal cancer: A study of 1012 cases from Thailand. Siriraj Med J. 2020;72(5):386-90.
Rodríguez-Almagro J, García-Manzanares A, Lucendo AJ, Hernández-Martínez A. Health-related quality of life in diabetes mellitus and its social, demographic and clinical determinants: A nationwide cross-sectional survey. J Clin Nurs. 2018;27(21-22):4212-23.
Best AL, Shukla R, Adamu AM, Martinez Tyson D, Stein KD, Alcaraz KI. Impact of caregivers' negative response to cancer on long-term survivors' quality of life. Support Care Cancer. 2021;29(2):679-86.
Chavasiri C, Sukprasert N, Chavasiri S. Depression and quality of life in spinal cord injury patients living in the community after hospital discharge. Siriraj Med J. 2020;72(1):59-66.
Souza JLdCAd, Nahas CSR, Nahas SC, Marques CFS, Ribeiro Junior U, Cecconello I. Health-related quality of life assessment in patients with rectal cancer treated with curative intent. Arquivos de Gastroenterologia. 2018;55:154-9.
Published
How to Cite
License
Copyright (c) 2025 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














