Accuracy of Breast Magnetic Resonance Imaging (MRI) and Breast Ultrasound Compared to Pathology in Assessing Residual Tumor in Breast Cancer Patients Receiving Neoadjuvant Systemic Treatment at Siriraj Hospital
DOI:
https://doi.org/10.33192/smj.v77i9.276157Keywords:
Breast cancer, neoadjuvant chemotherapy, MRI, ultrasound, pathological concordanceAbstract
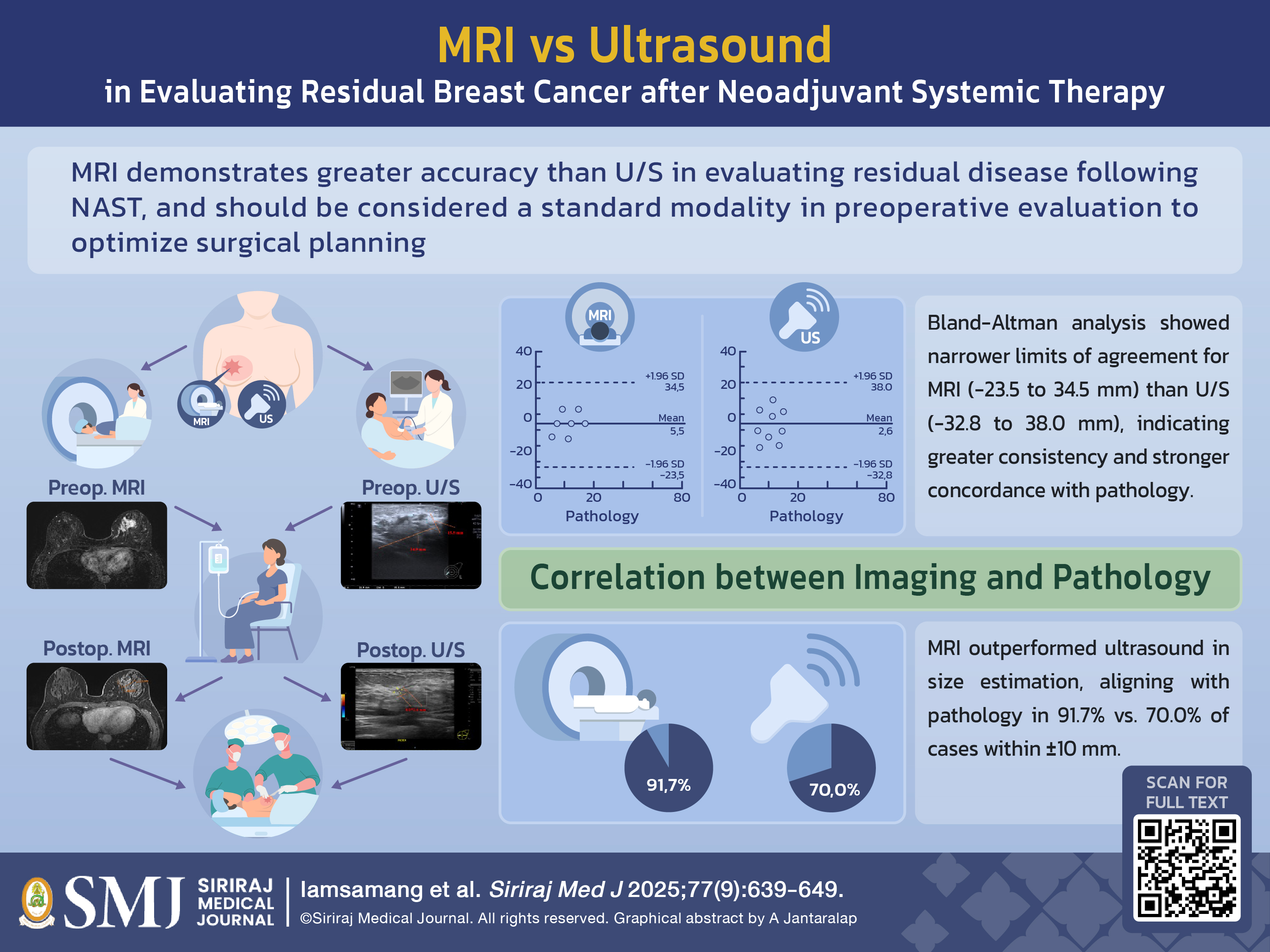
Objective: To evaluate the accuracy of magnetic resonance imaging (MRI) and ultrasound (US) in assessing residual tumor size compared to pathological findings in breast cancer patients who received neoadjuvant systemic treatment (NAST), and to examine the influence of imaging on surgical planning across different molecular subtypes.
Materials and Methods: This retrospective study included 24 breast cancer patients who underwent NAST followed by surgery at Siriraj Hospital between 2016 and 2024. Preoperative breast MRI and breast US, performed within 3–6 weeks prior to surgery, were compared with pathological tumor size. Analysis focused on mass lesions, with nonmass enhancement (NME) considered in selected cases where it presented. Imaging findings were independently reviewed by a second, blinded radiologist. Concordance between imaging and pathology was assessed.
Results: A total 24 patients were analyzed. MRI showed superior agreement with pathological tumor size, with 91.7% of cases falling within a ±10 mm margin, compared to 70.0% for US. Mean tumor sizes were 5.4 mm for MRI, 8.3 mm for US, and 10.9 mm based on pathological examination. Bland-Altman analysis revealed better agreement between MRI and pathology (limits of agreement: –23.5 – 34.5 mm) compared to US. These results highlight the superior accuracy and reliability of MRI over US for preoperative tumor size assessment.
Conclusion: MRI demonstrates greater accuracy than US in evaluating residual disease following NAST. In case of invasive lobular carcinoma (ILC) subtypes, incorporating NME into imaging assessment may improve concordance with pathological findings. MRI should be considered a standard modality in preoperative evaluation to optimize surgical planning.
References
ทะเบียนมะเร็งระดับโรงพยาบาลพ.ศ. 2564 สถาบันมะเร็งแห่งชาติกรมการแพทย์กระทรวงสาธารณสุข, www.nci.go.th/e_book/hosbased_2564/index.html
Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, et al. Pathological complete response and long term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164-72. DOI: https://doi.org/10.1016/S0140-6736(13)62422-8
Zheng C-H, Xu K, Shan W-P, Zhang Y-K, Su Z-D, Gao X-J, et al. Meta-Analysis of Shrinkage Mode After Neoadjuvant Chemotherapy for Breast Cancers: Association With Hormonal Receptor. Front Oncol. 2022;11:617167. DOI: https://doi.org/10.3389/fonc.2021.617167
Negarao EMS, Souza JA, Marques EF. Breast cancer phenotype influences MRI response evaluation after neoadjuvant chemotherapy. Eur J Radiol. 2019;120:108701. DOI: https://doi.org/10.1016/j.ejrad.2019.108701
Price ER, Wong J, Mukhtar R, Hylton N, Esserman LJ. How to use magnetic resonance imaging following neoadjuvant chemotherapy in locally advanced breast cancer. World J Clin Cases. 2015;3(7):607-13. DOI: https://doi.org/10.12998/wjcc.v3.i7.607
Boughey JC, McCall LM, Ballman KV, Mittendorf EA, Ahrendt GM, Wilke LG, et al. Tumor Biology Correlates With Rates of Breast-Conserving Surgery and Pathologic Complete Response After Neoadjuvant Chemotherapy for Breast Cancer: Findings From the ACOSOG Z1071 (Alliance) Prospective Multicenter Clinical Trial. Ann Surg. 2014; 260(4):608–16. DOI: https://doi.org/10.1097/SLA.0000000000000924
JEON-HOR CHEN. Impact of Factors Affecting the Residual Tumor Size Diagnosed by MRI Following Neoadjuvant Chemotherapy in Comparison to Pathology. J Surg Oncol. 2014;109(2):158-67. DOI: https://doi.org/10.1002/jso.23470
Kim J, Han B, Ko E, Ko E, Choi J, Park K. Prediction of pathologic complete response on MRI in patients with breast cancer receiving neoadjuvant chemotherapy according to molecular subtypes. Eur Radiol. 2022;32(6):4056-66. DOI: https://doi.org/10.1007/s00330-021-08461-0
Croshaw R, Shapiro-Wright H, Svensson E, Erb K, Julian T. Accuracy of clinical examination, digital mammogram, ultrasound, and MRI in determining postneoadjuvant pathologic tumor response in operable breast cancer patients. Ann Surg Oncol. 2011;18:3160-3. DOI: https://doi.org/10.1245/s10434-011-1919-5
Jiyoon Park, Eun Young Chae, Jo Hee Cha, Hee Jung Shin, Woo Jung Choi, Young-Wook Choi, et al. Comparison of mammography, digital breast tomosynthesis, automated T breast ultrasound, magnetic resonance imaging in evaluation of residual tumor after neoadjuvant chemotherapy. Eur J Radiol. 2018;108:261–8. DOI: https://doi.org/10.1016/j.ejrad.2018.09.032
Poplack SP, Tosteson TD, Kogel CA, Nagy HM. Digital breast tomosynthesis: initial experience in 98 women with abnormal digital screening mammography. AJR Am J Roentgenol. 2007;189(3):616–23. DOI: https://doi.org/10.2214/AJR.07.2231
Fornvik D, Zackrisson S, Ljungberg O, Svahn T, Timberg P, Tingberg A, Andersson I. Breast tomosynthesis: accuracy of tumor measurement compared with digital mammography and ultrasonography. Acta Radiol. 2010;51(3):240–7. DOI: https://doi.org/10.3109/02841850903524447
Hakim CM, Chough DM, Ganott MA, Sumkin JH, Zuley ML, Gur D. Digital breast tomosynthesis in the diagnostic environment: a subjective side-by-side review. AJR Am. J Roentgenol. 2010;195:W172–6. DOI: https://doi.org/10.2214/AJR.09.3244
Park JM, Franken Jr. EA, Garg M, Fajardo LL, Niklason LT. Breast tomosynthesis: present considerations and future applications. Radiographics. 2007;27 Suppl 1:S231–S40. DOI: https://doi.org/10.1148/rg.27si075511
Bernardi D, Vatteroni G, Acquaviva A, Valentini M, Sabatino V, Bolengo I, et al. Contrast-Enhanced Mammography Versus MRI in the Evaluation of Neoadjuvant Therapy Response in Patients With Breast Cancer: A Prospective Study. AJR Am J Roentgenol. 2022;219(6):884–94. DOI: https://doi.org/10.2214/AJR.22.27756
Lobbes MBI, Previous R, Smidt M, Tjan-Heijnen VCG, van Goethem M, Schipper R, et al. The role of magnetic resonance imaging in assessing residual disease and pathologic complete response in breast cancer patients receiving neoadjuvant chemotherapy: a systematic review. Insights Imaging. 2013;4(2):163–75. DOI: https://doi.org/10.1007/s13244-013-0219-y
Yuan Y, Chen X-S, Liu S-Y, Shen K-W. Accuracy of MRI in prediction of pathologic complete remission in breast cancer after preoperative therapy: a meta-analysis. AJR Am J Roentgenol. 2010;195(1):260– 8. DOI: https://doi.org/10.2214/AJR.09.3908
Marinovich ML, Houssami N, Macaskill P, Sardanelli F, Irwig L, Mamounas EP, et al. Meta-analysis of Magnetic Resonance Imaging in Detecting Residual Breast Cancer After Neoadjuvant Therapy. J Natl Cancer Inst. 2013;105:321–33. DOI: https://doi.org/10.1093/jnci/djs528
França LKL, Bitencourt AGV, Paiva HLS, Silva CB, Pereira NP, Paludo J, et al. Role of magnetic resonance imaging in the planning of breast cancer treatment strategies: comparison with conventional imaging techniques. Radiol Bras. 2017;50(2):76–81. DOI: https://doi.org/10.1590/0100-3984.2015.0124
França LKL, Bitencourt AGV, Osório VAB, Graziano L, Guatelli CS, Souza JA, et al. Tumor size assessment of invasive breast cancers: which pathological features affect MRI-pathology agreement. Applied Cancer Research. 2018;38:2. DOI: https://doi.org/10.1186/s41241-018-0055-y
Ko ES, Han BK, Kim RB, Ko EY, Shin JH, Hahn SY, et al. Analysis of Factors That Influence the Accuracy of Magnetic Resonance Imaging for Predicting Response after Neoadjuvant Chemotherapy in Locally Advanced Breast Cancer. Ann Surg Oncol. 2013; 20:2562–8. DOI: https://doi.org/10.1245/s10434-013-2925-6
Bahri S, Chen JH, Mehta RS, Carpenter PM, Nie K, Kwon S, et al. Residual Breast Cancer Diagnosed by MRI in Patients Receiving Neoadjuvant Chemotherapy with and Without Bevacizumab. Ann Surg Oncol. 2009;16:1619–28. DOI: https://doi.org/10.1245/s10434-009-0441-5
Kim HJ, Im YH, Han BK, Choi N, Lee J, Kim JH, et al. Accuracy of MRI for Estimating Residual Tumor Size after Neoadjuvant Chemotherapy in Locally Advanced Breast Cancer: Relation to Response Patterns on MRI. Acta Oncol Stockh Swed. 2007;46:996–1003. DOI: https://doi.org/10.1080/02841860701373587
Thiravit S. The Background Parenchymal Enhancement in Preoperative Breast MRI: The Effect on Tumor Extent Evaluation. Siriraj Med J. 2017;69(5):290-6.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2025 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














