Microwave Oven vs Level-1 Rapid Fluid Warmer: A Comparative Efficacy Study of Fluid Warming in the ATLS Protocol (MOLEWA Study)
DOI:
https://doi.org/10.33192/smj.v77i9.276168Keywords:
Microwave, fluid warming, trauma, initial managementAbstract
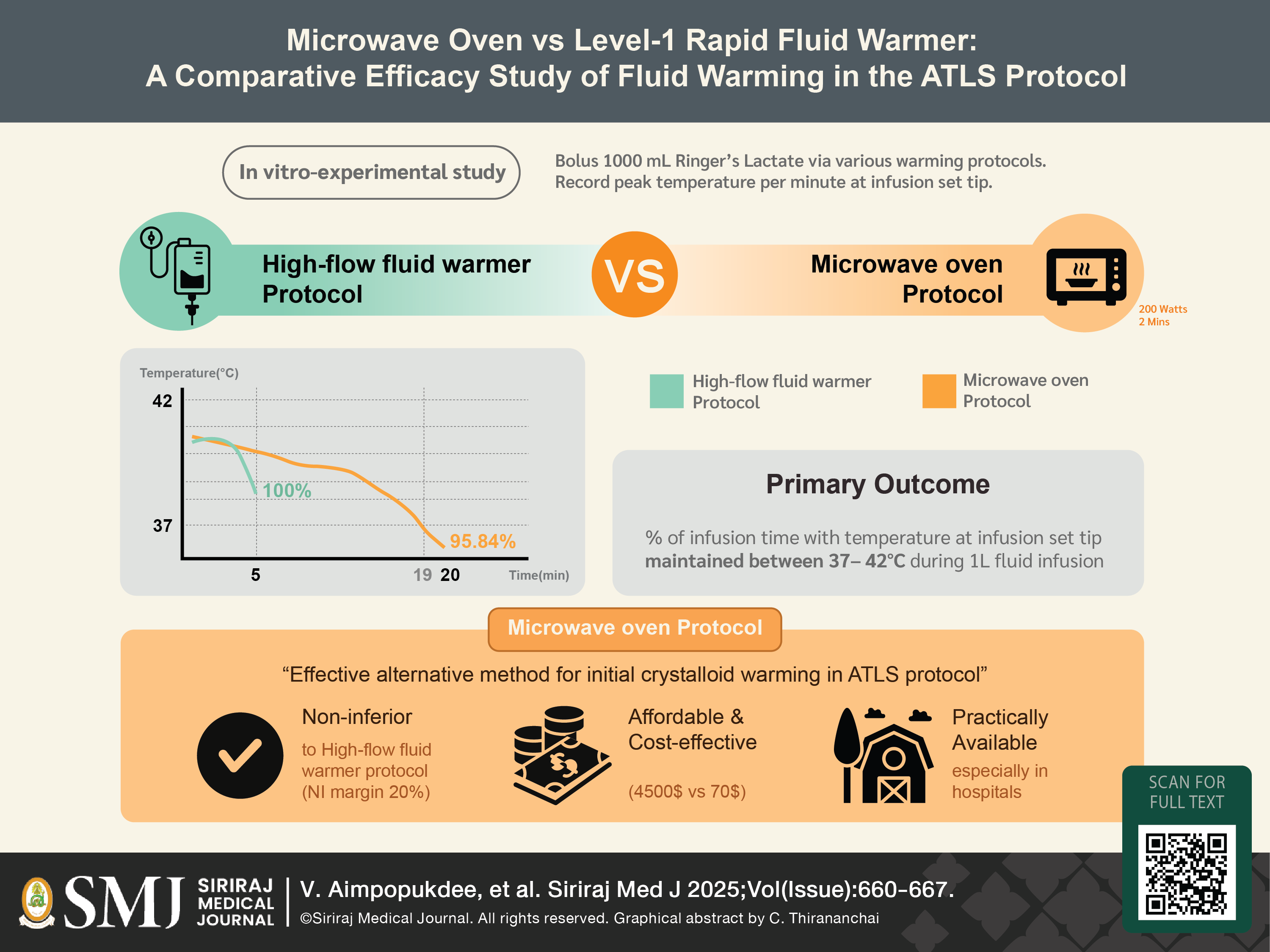
Objective: Although the use of a microwave for fluid warming has been proposed, standardized protocols for its clinical application remain limited. The purpose of this study is to evaluate the effectiveness of microwave-based fluid warming compared to conventional fluid warming equipment.
Materials and Methods: This in-vitro experimental study was conducted in two phases. In the pilot trial, we compared five groups using different combinations of container types, infusion rates, and warming techniques. In the second phase, a non-inferiority trial, two groups of 18 1-liter isotonic crystalloid bottles were compared: one using the Level-1 H-1200 fluid warmer and the other employing a microwave oven warming protocol (800W, two minutes at maximum power). The primary outcome was the percentage of infusion time during which the fluid temperature at the tip of the infusion set remained within the target range of 37°C to 42°C.
Results: The warming cabinet and microwave oven achieved mean infusion durations of 5.0 and 19.5 minutes, respectively. The Level-1 group maintained the target temperature for 100% of the infusion duration, while the microwave group achieved a rate of 95.84% [95.82%-95.86%], demonstrating non-inferiority to the Level-1 method.
Conclusion: Microwave fluid warming is a feasible, practical, and cost-effective alternative to conventional fluid warming equipment. Its comparable warming efficiency and wide availability support its potential use in rural areas with limited resources.
References
American College of Surgeons CoT. Initial Assessment and management. AdvancedTrauma Life Support (ATLS) Course Manual (10th ed.). Chicago, IL: American College of Surgeons; 2018.p.2-22.
Somnuke P, Pongraweewan O, Siriussawakul A. Optimizing Perioperative Care for Elderly Surgical Patients: A Review of Strategies and Evidence-Based Practices. Siriraj Med J. 2024;76(7):465-72. DOI: https://doi.org/10.33192/smj.v76i7.268063
Werwath DL, Schwab CW, Scholten JR, Robinett W. Microwave ovens. A safe new method of warming crystalloids. Am Surg. 1984;50(12):656-9.
Chittawatanarat K, Akanitthaphichat S. Microwave oven: how to use it as a crystalloid fluid warmer. J Med Assoc Thai. 2009;92(11):1428-33.
Seo JS, Choi SP, Choi SM, 6 authors, et al. Delivery Temperature of Warmed Saline or Blood at Variable Flow Rates. J Korean Soc Emerg Med. Year?;14(1):83-87.
Meyer T, Ribeiro M, Mendonça A. Experimental study of adequate microwave warming of crystalloids and derivation of an equation for calculating heating parameters. Rev Bras Cir Plástica. 2012;27:518-22. DOI: https://doi.org/10.1590/S1983-51752012000400007
Marín P, Rincon-Valenzuela D, Monroy-Charry A, Ruiz-Villa J, Higuera-Redondo G, Rubio J. Encuesta de actitudes sobre vigilancia de la temperatura y protección térmicaperioperatoria en Colombia. Rev Colomb Anestesiol. 2016;44. DOI: https://doi.org/10.1016/j.rca.2016.05.007
Lindhoff GA, MacG Palmer JH. An assessment of the thermal safety of microwave warming of crystalloid fluids. Anaesthesia. 2000;55(3):251-4. DOI: https://doi.org/10.1046/j.1365-2044.2000.01319.x
Maddah H. Polypropylene as a Promising Plastic: A Review. 2163-1352. 2016;2016:1-11.
Nutrition C for FS and A. Guidance for Industry: Preparation of PremarketSubmissions for Food Contact Substances (Chemistry Recommendations). Published September 28, 2022. Accessed December 18, 2023. https://www.fda.gov/regulatory-information/search-fda- guidance-documents/guidance-industry-preparation-premarket-submissions-food-contact- substances-chemistry
Bettaieb A, Averill-Bates DA. Thermotolerance induced at a fever temperature of 40 degrees C protects cells against hyperthermia-induced apoptosis mediated by death receptor signalling. Biochem Cell Biol Biochim Biol Cell. 2008;86(6):521-38. DOI: https://doi.org/10.1139/O08-136
Cheney FW, Posner KL, Caplan RA, Gild WM. Burns from Warming Devices inAnesthesia: A Closed Claims Analysis. Anesthesiology. 1994;80(4):806-10. DOI: https://doi.org/10.1097/00000542-199404000-00012
Sieunarine K, White GH. Full-thickness burn and venous thrombosis following intravenous infusion of microwave-heated crystalloid fluids. Burns. 1996;22(7):568-9. DOI: https://doi.org/10.1016/0305-4179(96)00020-4
Kimberger O, Held C, Stadelmann K, Mayer N, Hunkeler C, Sessler DI, Kurz A. Resistive polymer versus forced-air warming: comparable heat transfer and core rewarming rates in volunteers. Anesth Analg. 2008;107(5):1621-6. DOI: https://doi.org/10.1213/ane.0b013e3181845502
John M, Crook D, Dasari K, Eljelani F, El-Haboby A, Harper CM. Comparison of resistive heating and forced-air warming to prevent inadvertent perioperative hypothermia. Br J Anaesth. 2016;116(2):249-54. DOI: https://doi.org/10.1093/bja/aev412
National Institute for Health and Care Excellence (NICE). Hypothermia: prevention and management in adults having surgery. NICE guideline [NG65]. London: NICE; 2016.
Hussain KA, Romanova S, Okur I, Zhang D, Kuebler J, Huang X, et al. Assessing the Release of Microplastics and Nanoplastics from Plastic Containers and Reusable Food Pouches: Implications for Human Health. Environ Sci Technol. 2023;57(26):9782-92. DOI: https://doi.org/10.1021/acs.est.3c01942
Abhrajyoti Tarafdar, Junhao Xie, Aoif Gowen, Amy Claire O'Higgins, Junli Xu. Microplastic Transfer into the Bloodstream from Intravenous Fluid Infusion Systems. Available at http://dx.doi.org/10.2139/ssrn.4709116 DOI: https://doi.org/10.2139/ssrn.4709116
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2025 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














