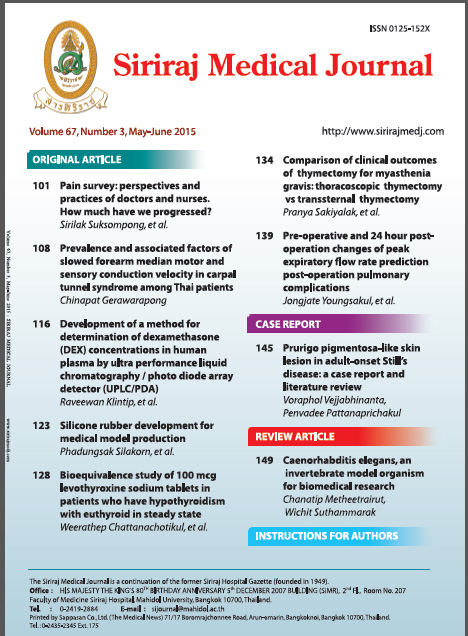
Pre-operative and 24 hourPost-operation Changes of Peak Expiratory Flow RatePrediction Post-operation Pulmonary Complications
Abstract
Background: Post-operative pulmonary complications (PPCs) are common problems after abdominal operations. The incidence varies from 10 to 69% for atelectasis and 9 to 40% for post-operation pneumonia. Many studies have investigated risk factors and risk indices for predicting PPCs. However, no definite predictors for PPCs have yet been described.
Objective: To develop a simple, reliable, and safe diagnostic tool for early detection of post-operation pulmonary complications.
Methods: A series of 151 consecutive patients scheduled for elective abdominal operations were studied between 1 September 2003 and 31 August 2004 at The Department of Surgery, Faculty of Medicine at Siriraj Hospital. The patients were measured for peak expiratory flow rate (PEFR) a night before operation, followed by every 24 hr post-operation. The data was analyzed using univariate and multivariate regression analyses with respect to post-operation pulmonary complications.
Results: A total of 15 patients (9.9%) developed post-operation pulmonary complications. Univariate analysis demonstrated that preoperative PEFR (PrePEFR) and 24 hr post-operation PEFR (PostPEFR) could predict PPCs. Using multivariate regression analyses, the PEFR Score was developed and calculated as (17.24 х Malignant)-(0.16 х PostPEFR). A cut point value was -4.68. The diagnostic sensitivity was 80% and specificity was 73.5%.
Conclusion: 24 hours post-operation PEFR is a simple and valuable bedside method for predicting PPCs.
Keywords: Peak expiratory flow rate, post-operative pulmonary complications
Downloads
Published
How to Cite
Issue
Section
License
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.