The Potential of Vitamin-D-Binding Protein as a Urinary Biomarker to Distinguish Steroid-Resistant from Steroid-Sensitive Idiopathic Nephrotic Syndrome in Iraqi Children
DOI:
https://doi.org/10.33192/smj.v75i4.260831Keywords:
Nephrotic syndrome, Biomarker, Vitamin D binding protein, Steroid-sensitive nephrotic syndrome, Steroid-resistant nephrotic syndromeAbstract
Objective: To determine the ability of uVDBP to discern SRNS from steroid-sensitive nephrotic syndrome (SSNS) in Iraqi children.
Materials and Methods: This cross-sectional study enrolled children with SRNS (n=31) and SSNS (n=32) from the pediatric nephrology clinic of Babylon Hospital for Maternity and Pediatrics over three months. Patients' characteristics in terms of demographics, clinical data, and urinary investigations were collected. Quantitative analysis of uVDBP levels was undertaken via a commercially available ELISA kit.
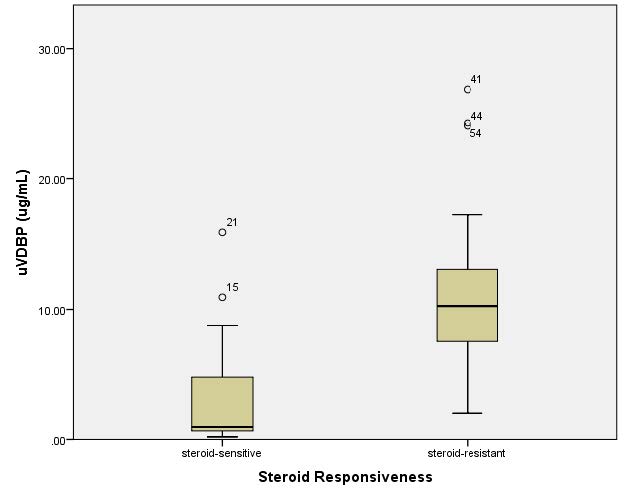
Results: The median uVDBP values were significantly higher (p-value<0.001) in the SRNS group (median=10.26, IQR=5.91 μg/mL) than in the SSNS group (median=0.953, IQR=4.12 μg/mL). A negative correlation was noted between uVDBP levels and estimated glomerular filtration rate (eGFR) (Spearman's rho coefficient= − 0.494, p=0.001). Nevertheless, the rise in uVDBP concentrations was still considerable in children with SRNS whose eGFR measurements were above 60 mL/min/1.73 m2. The study revealed a good discriminatory power for uVDBP as a predicting parameter to distinguish SRNS from SSNS (AUC= 0.909, p<0.0001. The optimal uVDBP cut-off value of 5.781 μg/mL was associated with a sensitivity of 0.839 and specificity of 0.844 to differentiate SRNS from SSNS.
Conclusion: Considering its significant discriminatory strength, uVDBP can be considered as a potential marker to noninvasively distinguish children with SRNS from those with SSNS.
References
Eddy AA, Symons JM. Nephrotic syndrome in childhood. Lancet Lond Engl. 2003 Aug 23;362(9384):629–39.
Ehren R, Benz MR, Brinkkötter PT, Dötsch J, Eberl WR, Gellermann J, et al. Pediatric idiopathic steroid-sensitive nephrotic syndrome: diagnosis and therapy -short version of the updated German best practice guideline (S2e) - AWMF register no. 166-001, 6/2020. Pediatr Nephrol Berl Ger. 2021 Oct;36(10):2971–85.
Noone DG, Iijima K, Parekh R. Idiopathic nephrotic syndrome in children. Lancet Lond Engl. 2018 Jul 7;392(10141):61–74.
Arif MK, Arif M, Amjad N. A histopathological outlook on nephrotic syndrome: A pediatric perspective. Indian J Nephrol. 2016 Jun;26(3):188–91.
Ahmed NF, Ibrahim R. Childhood nephritic syndrome Clinical manifestations and histopathlogical spectrum. J Fac Med Baghdad. 2007 Oct 1;49(3):304–6.
Azat NFA, hameed NN, Sahib OA. Pediatric Glomerular Diseases (Review of histopathological subtypes). J Fac Med Baghdad. 2010 Apr 4;52(1):1–2.
Wine R, Vasilevska-Ristovska J, Banh T, Knott J, Noone D, Gbadegesin R, et al. Trends in the epidemiology of childhood nephrotic syndrome in Africa: A systematic review. Glob Epidemiol. 2021 Nov 1;3:100061.
Gipson DS, Chin H, Presler TP, Jennette C, Ferris ME, Massengill S, et al. Differential risk of remission and ESRD in childhood FSGS. Pediatr Nephrol Berl Ger. 2006 Mar;21(3):344–9.
Roberti I, Vyas S. Long-term outcome of children with steroid-resistant nephrotic syndrome treated with tacrolimus. Pediatr Nephrol Berl Ger. 2010 Jun;25(6):1117–24.
Hari P, Bagga A, Jindal N, Srivastava RN. Treatment of focal glomerulosclerosis with pulse steroids and oral cyclophosphamide. Pediatr Nephrol Berl Ger. 2001 Nov;16(11):901–5.
FRANKUL FarM, Fahmi N, Ahmed L. HYPERTENSION IN CHILDREN WITH NEPHROTIC SYNDROME. J Fac Med Baghdad. 2005 Apr 3;47(1):5–8.
Hilmanto D, Mawardi F, Lestari AS, Widiasta A. Disease-Associated Systemic Complications in Childhood Nephrotic Syndrome: A Systematic Review. Int J Nephrol Renov Dis. 2022;15:53–62.
Bonilla-Felix M, Parra C, Dajani T, Ferris M, Swinford RD, Portman RJ, et al. Changing patterns in the histopathology of idiopathic nephrotic syndrome in children. Kidney Int. 1999 May;55(5):1885–90.
Kari JA. Changing trends of histopathology in childhood nephrotic syndrome in western Saudi Arabia. Saudi Med J. 2002 Mar;23(3):317–21.
Mohammed TF, Al-Badri AA, Abd Al-Latteef A, Abdulhussain RMH. Trends of Histopathology in Childhood Nephrotic Syndrom. Iraqi Postgrad Med J. 2009;1(1):47–55.
Asinobi AO, Ademola AD, Okolo CA, Yaria JO. Trends in the histopathology of childhood nephrotic syndrome in Ibadan Nigeria: preponderance of idiopathic focal segmental glomerulosclerosis. BMC Nephrol. 2015 Dec 15;16(1):213.
Gipson PE, Gipson DS. CHAPTER 27 - Focal segmental glomerulosclerosis. In: LERMA EV, SPARKS MA, M. TOPF J, editors. Nephrology Secrets (Fourth Edition) [Internet]. Elsevier; 2019. p. 186–91. Available from: https://www.sciencedirect.com/science/article/pii/B9780323478717000368
Ahmed NF, Hussain HH. Chronic Renal Failure in Children Admitted to Children Welfare Teaching Hospital. Iraqi Postgrad Med J. 2008 Jan 1;7(1):12–7.
Trautmann A, Vivarelli M, Samuel S, Gipson D, Sinha A, Schaefer F, et al. IPNA clinical practice recommendations for the diagnosis and management of children with steroid-resistant nephrotic syndrome. Pediatr Nephrol Berl Ger. 2020 Aug;35(8):1529–61.
Tullus K, Webb H, Bagga A. Management of steroid-resistant nephrotic syndrome in children and adolescents. Lancet Child Adolesc Health. 2018 Dec;2(12):880–90.
Schijvens AM, Teeninga N, Dorresteijn EM, Teerenstra S, Webb NJ, Schreuder MF. Steroid treatment for the first episode of childhood nephrotic syndrome: comparison of the 8 and 12 weeks regimen using an individual patient data meta-analysis. Eur J Pediatr. 2021 Sep 1;180(9):2849–59.
Rovin BH, Adler SG, Barratt J, Bridoux F, Burdge KA, Chan TM, et al. KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Kidney Int. 2021 Oct 1;100(4):S1–276.
Glassock RJ. Con: kidney biopsy: an irreplaceable tool for patient management in nephrology. Nephrol Dial Transplant. 2015 Apr;30(4):528–31.
Jassil NK, Sharma A, Bikle D, Wang X. VITAMIN D BINDING PROTEIN AND 25-HYDROXYVITAMIN D LEVELS: EMERGING CLINICAL APPLICATIONS. Endocr Pract. 2017 May;23(5):605–13.
Yousefzadeh P, Shapses SA, Wang X. Vitamin D Binding Protein Impact on 25-Hydroxyvitamin D Levels under Different Physiologic and Pathologic Conditions. Int J Endocrinol. 2014;2014:981581.
Weng FL, Shults J, Herskovitz RM, Zemel BS, Leonard MB. Vitamin D insufficiency in steroid-sensitive nephrotic syndrome in remission. Pediatr Nephrol Berl Ger. 2005 Jan;20(1):56–63.
Solarin AU, Adekunle MO, Oladimeji AB, Olutekunbi OA, Lamina MO, Oshomah-Bello OE, et al. Vitamin D status and serum vitamin D binding protein levels in Nigerian children with nephrotic syndrome. Afr J Nephrol. 2022 Aug 18;25(1):149–54.
Marzouk H, Ghobrial E, Khorshied M, Mohammed M. Vitamin D level in nephrotic syndrome, Factors of impact? GEGET. 2019;14(2):53–61.
Bennett MR, Pordal A, Haffner C, Pleasant L, Ma Q, Devarajan P. Urinary Vitamin D-Binding Protein as a Biomarker of Steroid-Resistant Nephrotic Syndrome. Biomark Insights. 2016;11:1–6.
Choudhary A, Mohanraj PS, Krishnamurthy S, Rajappa M. Association of Urinary Vitamin D Binding Protein and Neutrophil Gelatinase-Associated Lipocalin with Steroid Responsiveness in Idiopathic Nephrotic Syndrome of Childhood. Saudi J Kidney Dis Transplant. 2020 Oct;31(5):946–56.
Aoun AH. Query About Validity of uVDBP as a Biomarker of Steroid-Resistant Nephrotic Syndrome. Biomark Insights. 2022;17:11772719221078372.
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982 Apr;143(1):29–36.
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, et al. New equations to estimate GFR in children with CKD. J Am Soc Nephrol JASN. 2009 Mar;20(3):629–37.
Bouillon R, Schuit F, Antonio L, Rastinejad F. Vitamin D Binding Protein: A Historic Overview. Front Endocrinol. 2019;10:910.
Vallés P, Peralta M, Carrizo L, Martin L, Principi I, Gonzalez A, et al. Follow-up of steroid-resistant nephrotic syndrome: tubular proteinuria and enzymuria. Pediatr Nephrol Berl Ger. 2000 Dec;15(3–4):252–8.
Woroniecki RP, Shatat IF, Supe K, Du Z, Kaskel FJ. Urinary cytokines and steroid responsiveness in idiopathic nephrotic syndrome of childhood. Am J Nephrol. 2008;28(1):83–90.
Woroniecki RP, Orlova TN, Mendelev N, Shatat IF, Hailpern SM, Kaskel FJ, et al. Urinary proteome of steroid-sensitive and steroid-resistant idiopathic nephrotic syndrome of childhood. Am J Nephrol. 2006;26(3):258–67.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














