Preemptive Analgesic Efficacy of Parecoxib for Reducing Postoperative Pain in Patients Undergoing Gynecological Surgery
DOI:
https://doi.org/10.33192/smj.v76i12.271058Keywords:
Preemptive analgesia, Parecoxib, Gynecological surgery, Postoperative painAbstract
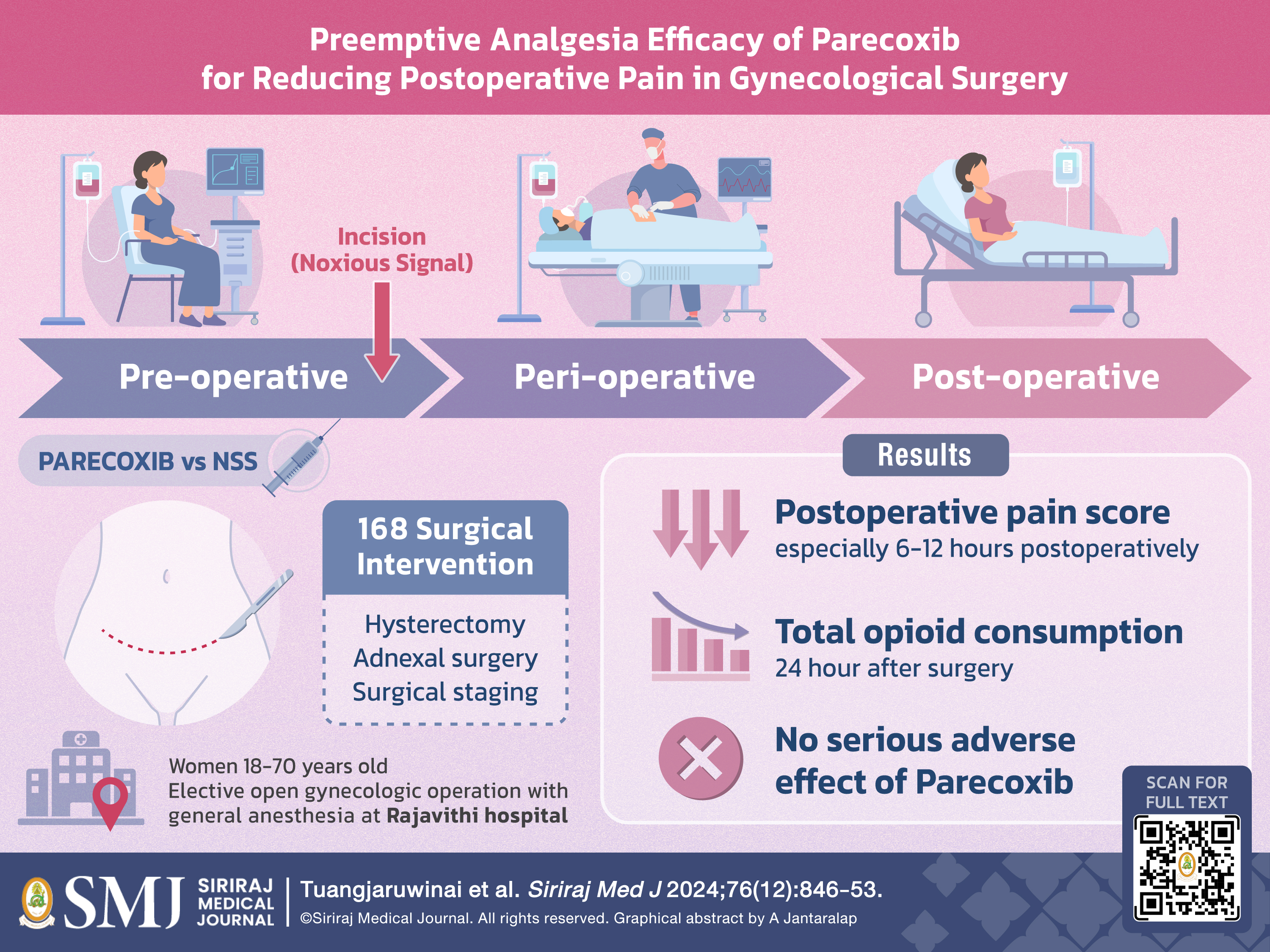
Objective: This study aimed to evaluate the effectiveness of preemptive parecoxib in reducing postoperative pain following gynecological surgery.
Materials and Methods: A double-blind, randomized study involved 168 patients undergoing laparotomy gynecological procedures, including total hysterectomy, adnexal surgery, and surgical staging, between November
2023 and July 2024. Patients were randomly assigned to receive either intravenous parecoxib (n = 82) or normal saline (n = 86) 15 minutes before surgery. Postoperative pain was measured using a visual analog scale at 2, 6, 12, and 24 hours. Morphine consumption within the first 24 hours post-surgery was recorded, along with any adverse events related to parecoxib and the length of hospital stay.
Results: Mean pain scores at 2, 6, 12, and 24 hours postoperatively were lower in the treatment group compared to the control group (5.3 vs. 5.7, p = 0.261; 3.7 vs. 5.0, p < 0.001; 3.3 vs. 5.1, p < 0.001; 3.5 vs. 4.0, p = 0.164, respectively). The mean 24-hour postoperative morphine consumption was significantly lower in the treatment group (4 ± 8 mg vs. 8 ± 5 mg, p < 0.001). No significant adverse events occurred between the groups. The total length of hospital stay was similar between the two groups (3.4 ± 1.8 vs. 3.5 ± 1.4 days, p = 0.698).
Conclusion: Preemptive parecoxib significantly reduced pain at 6 and 12 hours post-surgery and reduced morphine use within 24 hours, with no significant effect on hospital stay duration in gynecological surgery.
References
Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res. 2017;10:2287-98.
Benyamin R, Trescot AM, Datta S, Buenaventura R, Adlaka R, Sehgal N, et al. Opioid complications and side effects. Pain Physician. 2008;11(2 Suppl):S105-S20.
Schwenk ES, Mariano ER. Designing the ideal perioperative pain management plan starts with multimodal analgesia. Korean J Anesthesiol. 2018;71(5):345-52.
Smitasiri R, Chanthasenanont A, Chitkoolsamphan Y, Pongrojpaw D, Benchahong S, Suwannarurk K. Dexamethasone and Lidocaine Effects in 24 hours Post Cesarean Pain Reduction under Spinal Anesthesia: A Randomized Controlled Trial. Siriraj Med J. [Internet]. 2024 Sep. 1 [cited 2024 Oct 9];76(9):567-72. Available from: https://he02.tci-thaijo.org/index.php/sirirajmedj/article/view/268510
Boonyapalanant C, Woranisarakul V, Jitpraphai S, Chotikawanich E, Taweemonkongsap T, KC HB, et al. The Efficacy of Inside-Out Transversus Abdominis Plane Block vs Local Infiltration before Wound Closure in Pain Management after Kidney Transplantation: A Double-blind, Randomized Trial. Siriraj Med J. [Internet]. 2022 Apr. 1 [cited 2024 Oct. 9];74(4):233-8. Available from: https://he02.tci-thaijo.org/index.php/sirirajmedj/article/view/256916
Ohnesorge H, Gunther V, Grunewald M, Maass N, Alkatout I. Postoperative pain management in obstetrics and gynecology. J Turk Ger Gynecol Assoc. 2020;21(4):287-97.
Ong CK, Lirk P, Seymour RA, Jenkins BJ. The efficacy of preemptive analgesia for acute postoperative pain management: a meta-analysis. Anesth Analg. 2005;100(3):757-73.
Silverstein FE, Faich G, Goldstein JL, Simon LS, Pincus T, Whelton A, et al. Gastrointestinal toxicity with celecoxib vs nonsteroidal anti-inflammatory drugs for osteoarthritis and rheumatoid arthritis: the CLASS study: a randomized controlled trial. Celecoxib Long-term Arthritis Safety Study. JAMA. 2000;284(10):1247-55.
Pfizer. Dynastat (parecoxib sodium) - product information. https://labeling.pfizer.com/ShowLabeling.aspx?id=12244 [Accessed 12 August 2023].
Arponrat P, Pongrojpaw D, Tanprasertkul C, Suwannarurk K, Bhamarapravatana K. Postoperative pain relief in major gynaecological surgery by perioperative parecoxib administration: Thammasat University Hospital Study. J Med Assoc Thai. 2015;98(7):636-42.
Bunyavejchevin S, Prayoonwech C, Sriprajittichai P. Preemptive analgesic efficacy of parecoxib vs placebo in infertile women undergoing diagnostic laparoscopy: randomized controlled trial. J Minim Invasive Gynecol. 2012;19(5):585-8.
Nong L, Sun Y, Tian Y, Li H, Li H. Effects of parecoxib on morphine analgesia after gynecology tumor operation: a randomized trial of parecoxib used in postsurgical pain management. J Surg Res. 2013;183(2):821-6.
Ratchanon S, Phaloprakarn C, Traipak K. Pain control in laparoscopic gynecologic surgery with/without preoperative (preemptive) parecoxib sodium injection: a randomized study. J Med Assoc Thai. 2011;94(10):1164-8.
Published
How to Cite
License
Copyright (c) 2024 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














