Endovascular Versus Open Repair for Symptomatic, Non-Ruptured Abdominal Aortic Aneurysms: A Retrospective Cohort Study
DOI:
https://doi.org/10.33192/smj.v77i11.277132Keywords:
Abdominal aortic aneurysm, symptomatic, non-ruptured, endovascular repair, open repair, perioperative outcomes, survival analysisAbstract
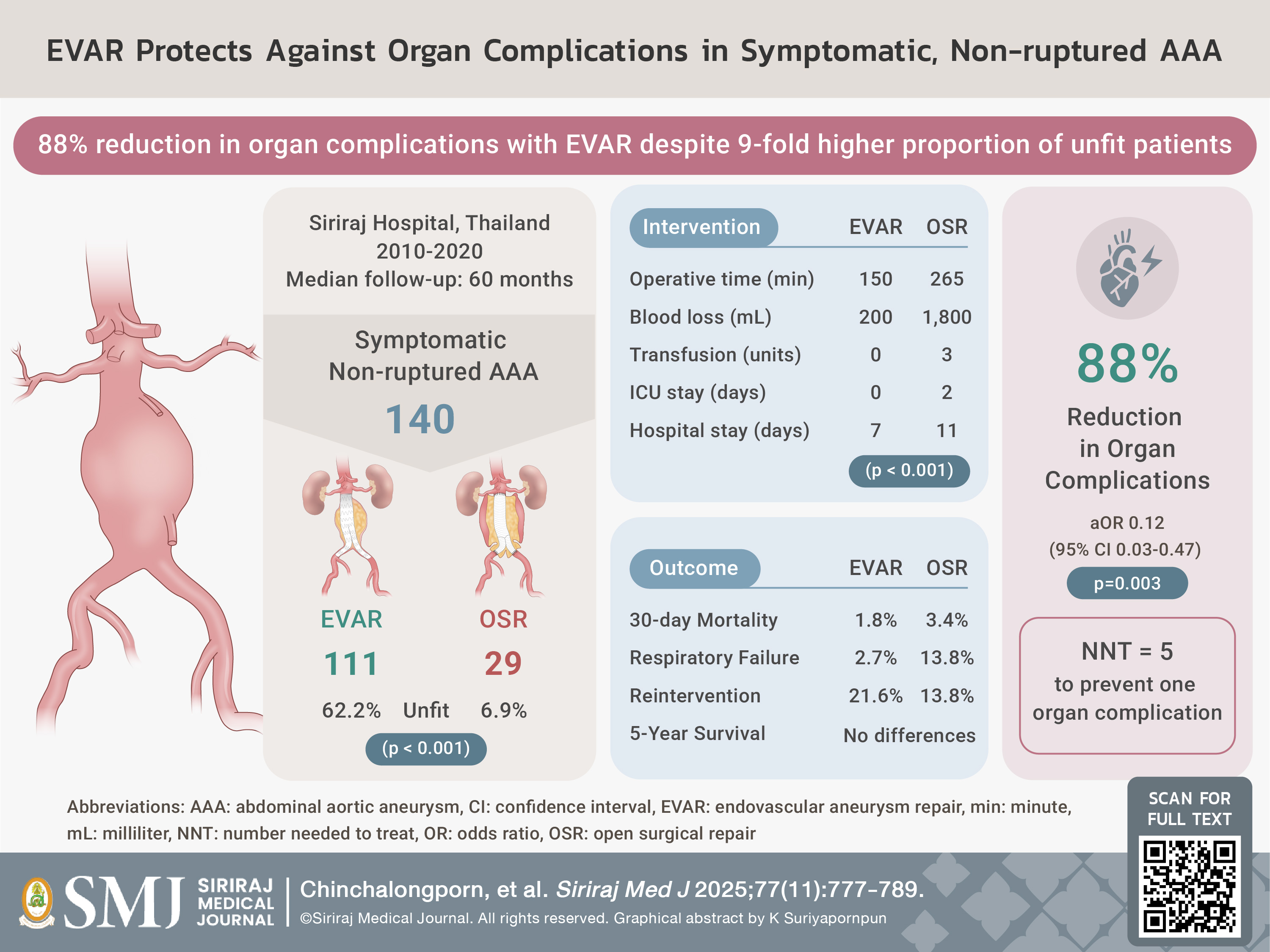
Objective: To compare perioperative organ morbidity, 30-day mortality, and 5-year overall survival following endovascular aneurysm repair (EVAR) versus open surgical repair (OSR) for symptomatic, non-ruptured abdominal aortic aneurysm (SnAAA).
Materials and Methods: We retrospectively reviewed 140 consecutive patients treated for SnAAA between 2010 and 2020 (EVAR n=111, OSR n=29). The primary endpoint was 30-day all-cause mortality; secondary endpoints included perioperative complications and 5-year survival. Due to extreme baseline imbalances (62.2% unfit in EVAR vs 6.9% in OSR) and limited sample size, multivariable adjustment was used instead of propensity score methods.
Results: Thirty-day mortality was 1.8% in the EVAR group and 3.4% in the OSR group (p=0.504, Fisher’s exact test). EVAR was associated with an 88% reduction in perioperative organ complications (adjusted OR 0.12, 95% CI 0.03-0.47, p=0.003), including a significant reduction in respiratory failure (2.7% vs 13.8%, OR 0.17, 95% CI 0.04-0.83, p=0.034). EVAR also resulted in shorter operative time (median 150 vs 265 minutes, p<0.001), reduced blood loss (200 vs 1,800 mL, p<0.001), and shorter hospital stay (7 vs 11 days, p<0.001). Five-year survival analysis revealed no significant difference between groups (log-rank p=0.193; adjusted HR 1.09, 95% CI 0.42-2.85, p=0.857).
Conclusions: Despite being performed in a higher-risk cohort, EVAR provided significant protection against organ complications without compromising long-term survival compared to OSR. These findings support EVAR as the preferred approach for unfit patients with SnAAA, while both strategies remain appropriate options for fit patients.
References
Sampson UK, Norman PE, Fowkes FG, Aboyans V, Song Y, Harrell FE, et al. Global and regional burden of aortic dissection and aneurysms: mortality trends in 21 world regions, 1990 to 2010. Glob Heart. 2014;9(1):171-80.e10.
Kontopodis N, Galanakis N, Antoniou SA, Tsetis D, Ioannou CV, Veith FJ, et al. Meta-Analysis and Meta-Regression Analysis of Outcomes of Endovascular and Open Repair for Ruptured Abdominal Aortic Aneurysm. Eur J Vasc Endovasc Surg. 2020;59(3):399-410.
Prinssen M, Verhoeven EL, Buth J, Cuypers PWM, van Sambeek MRHM, Balm R, et al. A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. N Engl J Med. 2004;351(16):1607-18.
EVAR trial participants. Endovascular aneurysm repair versus open repair in patients with abdominal aortic aneurysm (EVAR trial 1): randomised controlled trial. Lancet. 2005;365(9478):2179-86.
Lederle FA, Freischlag JA, Kyriakides TC, Padberg FT, Matsumura JS, Kohler TR, et al. Outcomes following endovascular vs open repair of abdominal aortic aneurysm: a randomized trial. JAMA. 2009;302(14):1535-42.
Powell JT, Sweeting MJ, Ulug P, Blankensteijn JD, Lederle FA, Becquemin JP, et al. Meta-analysis of individual-patient data from EVAR-1, DREAM, OVER and ACE trials comparing outcomes of endovascular or open repair for abdominal aortic aneurysm over 5 years. Br J Surg. 2017;104(3):166-78.
Antoniou GA, Antoniou SA, Torella F. Editor's Choice - Endovascular vs. Open Repair for Abdominal Aortic Aneurysm: Systematic Review and Meta-analysis of Updated Peri-operative and Long Term Data of Randomised Controlled Trials. Eur J Vasc Endovasc Surg. 2020;59(3):385-97.
Wanhainen A, Van Herzeele I, Goncalves FB, Montoya SB, Berard X, Boyle JR, et al. Editor's Choice -- European Society for Vascular Surgery (ESVS) 2024 Clinical Practice Guidelines on the Management of Abdominal Aorto-Iliac Artery Aneurysms. Eur J Vasc Endovasc Surg. 2024;67(2):192-331.
De Martino RR, Nolan BW, Goodney PP, Chang CK, Schanzer A, Cambria R, et al. Outcomes of symptomatic abdominal aortic aneurysm repair. J Vasc Surg. 2010;52(1):5-12.e1.
Prapassaro T, Chinsakchai K, Techarattanaprasert S, Wongwanit C, Ruansetakit C, Hongku K, et al. Determining Perioperative Mortality in Patients with Ruptured Abdominal Aortic Aneurysm: Insights from a Retrospective Cohort Study. Siriraj Med J. 2024;76(8):480-7.
Darling RC, Messina CR, Brewster DC, Ottinger LW. Autopsy study of unoperated abdominal aortic aneurysms. The case for early resection. Circulation. 1977;56(3 Suppl):II161-4.
Patel R, Sweeting MJ, Powell JT, Greenhalgh RM. Endovascular versus open repair of abdominal aortic aneurysm in 15-years' follow-up of the UK endovascular aneurysm repair trial 1 (EVAR trial 1): a randomised controlled trial. Lancet. 2016;388(10058):2366-74.
Wongwanit C, Mutirangura P, Chierakul N, Chaiyasoot W, Phongraweewan O. Rapidly Enlarging and Asymptomatic Abdominal Aortic Aneurysm in a Male Patient with Chronic Obstructive Pulmonary Disease: A Case Report of Endovascular Aortic Aneurysm Repair (EVAR). Siriraj Med J. 2006;58(5):812-8.
Brown LC, Epstein D, Manca A, Beard JD, Powell JT, Greenhalgh RM. The UK Endovascular Aneurysm Repair (EVAR) trials: design, methodology and progress. Eur J Vasc Endovasc Surg. 2004;27(4):372-81.
Chinsakchai K, Thorthititum D, Hongku K, Wongwanit C, Tongsai S, Sermsathanasawadi N, et al. Endovascular Versus Open Repair for Asymptomatic Abdominal Aortic Aneurysms: A 12-Year Retrospective Cohort Analysis. Ann Vasc Surg. 2025;112:363-72.
Uthoff H, Peña C, Katzen BT, Gandhi R, West J, Benenati JF, et al. Current clinical practice in postoperative endovascular aneurysm repair imaging surveillance. J Vasc Interv Radiol. 2012;23(9):1152-9.e6
Soden PA, Zettervall SL, Ultee KH, Karling JD, Buck DB, Hile CN, et al. Outcomes for symptomatic abdominal aortic aneurysms in the American College of Surgeons National Surgical Quality Improvement Program. J Vasc Surg. 2016;64(2):297-305.
Additional Files
Published
How to Cite
License
Copyright (c) 2025 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














