การศึกษาความสัมพันธ์ของสตรีตั้งครรภ์ติดโรคซิฟิลิสต่อผลลัพธ์การตั้งครรภ์และการเกิดทารกวินิจฉัยโรคซิฟิลิสโดยกำเนิดในโรงพยาบาลระยอง ระหว่างปี 2561-2563
คำสำคัญ:
สตรีตั้งครรภ์ติดโรคซิฟิลิส, ทารกวินิจฉัยโรคซิฟิลิสโดยกำเนิด, ผลลัพธ์การตั้งครรภ์บทคัดย่อ
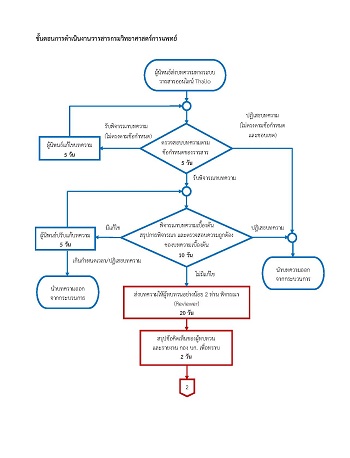
โรคซิฟิลิสเป็นโรคติดเชื้อผ่านทางเพศสัมพันธ์ เมื่อสตรีติดโรคซิฟิลิสขณะตั้งครรภ์จะทำให้เชื้อแพร่สู่ทารกผ่านทางรกและนํ้าครํ่า ส่งผลให้ทารกคลอดก่อนกำหนด ทารกวินิจฉัยโรคซิฟิลิสโดยกำเนิด และทารกเสียชีวิตในครรภ์ได้การศึกษานี้เพื่อหาผลลัพธ์ของการตั้งครรภ์และทารกในครรภ์จากสตรีตั้งครรภ์ติดโรคซิฟิลิสในโรงพยาบาลระยอง ระหว่างวันที่ 1 เมษายน พ.ศ. 2561 ถึง 31 มีนาคม พ.ศ. 2563 รวมถึงอัตราร้อยละของสตรีตั้งครรภ์ติดโรคซิฟิลิสและทารกติดโรคซิฟิลิสโดยกำเนิด และปัจจัยที่เกี่ยวข้อง สตรีตั้งครรภ์ติดโรคซิฟิลิส จำนวน 99 ราย อายุเฉลี่ย 21.5 ปี พบทารกแสดงอาการติดโรคซิฟิลิส โดยกำเนิดทั้งหมด 26 ราย (เป็นทารกเกิดมีชีพ 21 ราย และเสียชีวิต 5 ราย) อัตราการเกิดสตรีตั้งครรภ์ติดโรคซิฟิลิสเท่ากับร้อยละ 0.7 ในปี พ.ศ. 2561 และเพิ่มขึ้นเป็นร้อยละ 1.3 ในปี พ.ศ. 2562 กลุ่มทารกแรกเกิดติดโรคซิฟิลิสพบการคลอดก่อนกำหนดร้อยละ 42.3 และทารกโตช้าในครรภ์ร้อยละ 15.4 ปัจจัยในสตรีตั้งครรภ์ติดเชื้อ ได้แก่ การไม่ฝากครรภ์ การรักษาล่าช้าในไตรมาสที่สาม การรักษาไม่ครบสมบูรณ์และการไม่รับการรักษา สัมพันธ์กับการเกิดทารกติดโรคซิฟิลิสโดยกำเนิดอย่างมีนัยสำคัญทางสถิติ (p < 0.01) การศึกษานี้พบการติดโรคซิฟิลิสในสตรีตั้งครรภ์มีแนวโน้มเพิ่มขึ้นและส่งผลกระทบต่อการเกิดทารกแรกเกิดติดโรคซิฟิลิสเพิ่มขึ้น การนำข้อมูลจากการศึกษานี้ รวมทั้งการฝากครรภ์ที่เหมาะสมและการรักษาโรคครบอย่างน้อย 30 วันก่อนคลอดไปประยุกต์ใช้กับการวางแผนการรักษาสตรีตั้งครรภ์ติดโรคซิฟิลิสอาจส่งผลลัพธ์ที่ดีต่อทารกแรกเกิดในอนาคต
เอกสารอ้างอิง
สำนักโรคเอดส์ วัณโรค และโรคติดต่อทางเพศสัมพันธ์. แนวทางการดูแลรักษาโรคติดต่อทางเพศสัมพันธ์ พ.ศ. 2558. นนทบุรี: กรมควบคุมโรค กระทรวงสาธารณสุข; 2558.
World Health Organization. Report on global sexually transmitted infection surveillance 2015. Geneva, Switzerland: WHO; 2016.
Rowley J, Vander Hoorn S, Korenromp E, Low N, Unemo M, Abu-Raddad LJ, et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull World Health Organ 2019; 97(8): 548- 62.
Newman L, Rowley J, Vander Hoorn S, Wijesooriya NS, Unemo M, Low N, et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PLoS One 2015; 10(12): e0143304. (17 pages).
World Health Organization. Report on global sexually transmitted infection surveillance 2018. Geneva, Switzerland: WHO; 2018.
Tsai S, Sun MY, Kuller JA, Rhee EHJ, Dotters-Katz S. Syphilis in pregnancy. Obstet Gynecol Surv 2019; 74(9): 557-64.
Korenromp EL, Rowley J, Alonso M, Mello MB, Wijesooriya NS, Mahiane SG, et al. Global burden of maternal and congenital syphilis and associated adverse birth outcomes-Estimates for 2016 and progress since 2012. PLoS One 2019; 14(2): e0211720. (17 pages).
Zhang X, Yu Y, Yang H, Xu H, Vermund SH, Liu K. Surveillance of maternal syphilis in China: pregnancy outcomes and determinants of congenital syphilis. Med Sci Monit 2018; 24: 7727-35.
Su JR, Brooks LC, Davis DW, Torrone EA, Weinstock HS, Kamb ML. Congenital syphilis: trends in mortality and morbidity in the United States, 1999 through 2013. Am J Obstet Gynecol 2016; 214(3): 381.e1-9.
Sangtawesin V, Lertsutthiwong W, Kanjanapattanakul W, Khorana M, Horpaopan S. Outcome of maternal syphilis at Rajavithi Hospital on off springs. J Med Assoc Thai 2005; 88(11): 1519-25.
Kunpalin Y, Sirisabya A, Chaithongwongwatthana S. The surge of maternal and congenital syphilis in a tertiary care center in Bangkok, Thailand. Thai J Obstet Gynaecol 2019: 27(2): 100-8.
สำนักโรคเอดส์ วัณโรค และโรคติดต่อทางเพศสัมพันธ์. แนวทางระดับชาติเรื่องการกำจัดโรคซิฟิลิสแต่กำเนิดในประเทศไทย พ.ศ. 2558. นนทบุรี: กรมควบคุมโรค กระทรวงสาธารณสุข; 2557.
นพดล วัชระชัยสุรพล. Syphilis. ใน : สุวพร อนุกูลเรืองกิตติ์, วรรษมน จันทรเบญจกุล, ธันยวีร์ ภูธนกิจ, ชิษณุ พันธุ์เจริญ, บรรณาธิการ. New faces of pediatric infectious diseases: epidemiology, diagnosis, treatment and prevention. พิมพ์ครั้งที่ 2. กรุงเทพฯ: สาขาวิชาโรคติดเชื้อ ภาควิชากุมารเวชศาสตร์ คณะแพทยศาสตร์ จุฬาลงกรณ์มหาวิทยาลัย; 2563. หน้า 488-500.
Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015; 64(RR-03): 1-137.
Centers for Disease Control and Prevention. STD surveillance case definitions. [online]. 2013; [cited 2020 Nov 15 ]; [8 screens]. Aviable from: URL: https://www.cdc.gov/std/stats/casedefinitions-2014.pdf.
สำนักอนามัยการเจริญพันธุ์ กรมอนามัย กระทรวงสาธารณสุข. สถานการณ์อนามัยการเจริญพันธุ์ในวัยรุ่นและเยาวชน ปี 2562. [online]. 2563. [สืบค้น 15 พ.ย. 2563 ]; [30 หน้า]. เข้าถึงได้ที่: URL: https://rhold.anamai.moph.go.th/download/all_file/index/สถานการณ์RH_2562_Website.pdf.
Ganchimeg T, Ota E, Morisaki N, Laopaiboon M, Lumbiganon P, Zhang J, et al. Pregnancy and childbirth outcomes among adolescent mothers: a World Health Organization multicountry study. BJOG 2014; 121(Suppl 1): 40-8.
Dallé J, Baumgarten VZ, Ramos MC, Jimenez MF, Acosta L, Bumaguin DB, et al. Maternal syphilis and accomplishing sexual partner treatment: still a huge gap. Int J STD AIDS 2017; 28(9): 876-80.