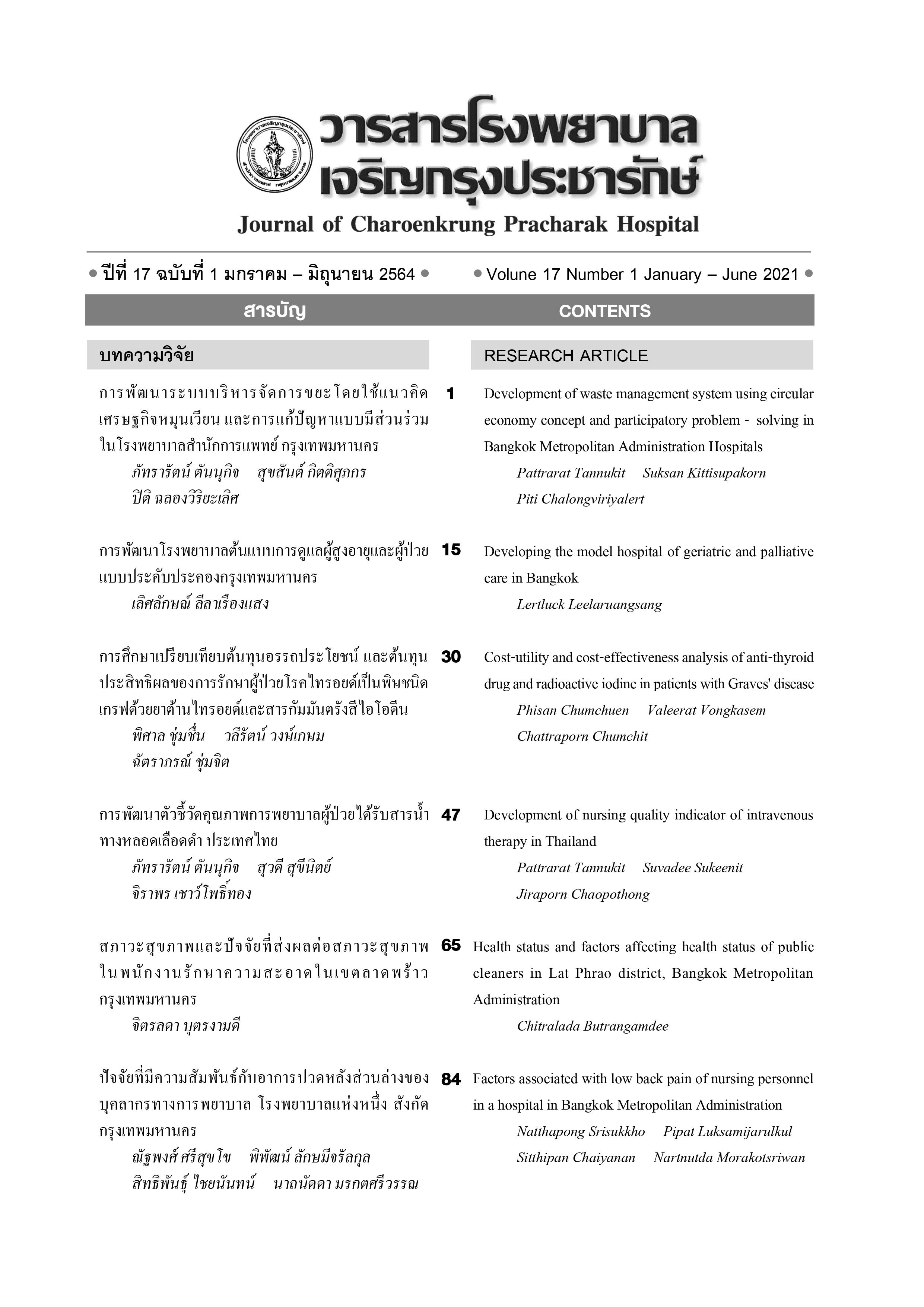
Cost-utility and cost-effectiveness analysis of anti-thyroid drug and radioactive iodine in Graves' disease patient: A prospective study
Main Article Content
Abstract
Objective: To study the therapeutic effect between the anti-thyroid hormone drugs compared (ATD) with the radioactive iodine (RAI) in the aspect of quality of life, cost, and effectiveness in Graves’ disease (GD).
Materials and Methods: The study was established in Damnoensaduak Hospital, Thailand, between July 2014 to July 2020. A total of 182 patients with GD were enrolled in the study (151 and 31 patients treated with ATD and RAI, respectively). The health utility (quality of life data) were collected before and after participating in the program measured by the EuroQol (EQ-5D) (Thai version). Cost-effectiveness evaluation from the costs invested in increasing one level of quality of life in each person was estimated. The health utility and cost were measured by using the comparison of the treatment outcomes between each treatment modality was made by an independent t-test.
Results: After two years of the following periods, the RAI treatment group show a higher significant cost than the ATD group (p< 0.01). The patients in the RAI treatment group also show a significant improvement in the quality of life than the ATD group; in terms of the utility score (p=0. 034) and remission rate (p<0.01). Cost-utility in the RAI treatment group and the ATD group provider views were 20,186.76 baht and 12,305.83 baht, respectively, and Cost-effectiveness in the RAI treatment group and the ATD group provider view were 578.93 baht and 120.07 baht, respectively.
Conclusions: RAI demonstrated a better improvement of cure rate and the health utility than the ATD, but the RAI is a higher cost for treatment strategy for GD.
Article Details
References
Bartalena L. Diagnosis and management of Graves disease: a global overview. Nat Rev Endocrinol
[Internet]. 2013 [cited 2019 Sep 15];9:724 - 34. Available from: http://www.ncbi.nlm.nih.gov/
pubmed/24126481.
พรรณทิพา ศักดิ์ทอง. คุณภาพชีวิตด้านสุขภาพ. กรุงเทพฯ: สำนักพิมพ์จุฬาลงกรณ์มหาวิทยาลัย; 2554.
วลีรัตน์ วงษ์เกษม, สุรสิทธิ์ ล้อจิตรอํานวย. อรรถประโยชน์ด้านสุขภาพของวิธีการรักษาโรคคอพอก
เป็นพิษจาก Graves' diease ในโรงพยาบาลดำเนินสะดวก. วารสารการแพทย์และวิทยาศาสตร์สุขภาพ
;19:38-45.
อุษา ฉายเกล็ดแก้ว, บรรณาธิการ. คู่มือการประเมินเทคโนโลยีด้านสุขภาพสําหรับประเทศ.
กรุงเทพฯ: บริษัท เดอะ กราฟิโก ซิสเต็มส์ จํากัด; 2552.
Tongsiri S. Valuing preferences for EQ-5D health states in the Thai general population. 2009.
Sakthong P, Charoenvisuthiwongs R, Shabunthom R. A comparison of EQ-5D index scores using the
UK, US, and Japan preference weights in a Thai sample with type 2 diabetes. Health Qual Life
Outcomes [Internet]. 2008 [cited 2020 Jan 26];6: 1-9 . Available from: https://pubmed.ncbi.nlm.nih.
gov/18811935/.
In H, Pearce EN, Wong AK, Burgess JF, McAneny DB, Rosen JE. Treatment options for Graves
disease: A cost-effectiveness analysis. J Am Coll Surg 2009; 209: 170-9.
Terwee CB, Gerding MN, Dekker FW, Prummel MF, Wiersinga WM. Development of a disease
specific quality of life questionnaire for patients with Graves’ ophthalmopathy: The GO-QOL. Br J
Ophthalmol [Internet]. 1998 [cited 2020 Oct 17];82:773-9. Available from: http://bjo.bmj.com/.
Park JJ, Sullivan TJ, Mortimer RH, Wagenaar M, Perry-Keene DA. Assessing quality of life in
Australian patients with Graves’ ophthalmopathy. Br J Ophthalmol [Internet]. 2004 [cited 2020 Oct
;88:75-8. Available from: http://bjo.bmj.com/.
Lumyongsatien M, Keeratidamkerngsakul B, Pornpanich K, Vangveeravong S, Saonanon P,
Wiwatwongwana D, et al. Development and psychometric properties of the Thai Graves’
ophthalmopathy quality of life (GO-QOL) questionnaire. J Patient-Reported Outcomes [Internet].
[cited 2020 Oct 17]; 4:1. Available from: https://jpro.springeropen.com/articles/ 10.1186/
s41687-019-0164-8.
Törring O, Watt T, Sjölin G, Byström K, Abraham-Nordling M, Calissendorff J, et al. Impaired
quality of life after radioiodine therapy compared to antithyroid drugs or surgical treatment for
Graves’ hyperthyroidism: A long-term follow-up with the thyroid-related patient-reported outcome
questionnaire and 36-item short form health status survey. Thyroid 2019;29:322-31.
Lee SY. Quality of life is worse at 6-10 years after radioactive iodine treatment of Graves’ disease as
compared with antithyroid drugs or surgery. Clin Thyroidol [Internet]. 2019 [cited 2020 Oct 17];
:144-7. Available from: www.liebertpub.com.
Conaglen HM, Tamatea JAU, Conaglen J V., Elston MS. Treatment choice, satisfaction and quality
of life in patients with Graves’ disease. Clin Endocrinol (Oxf) [Internet]. 2018 [cited 2020 Oct 17];
:977-84. Available from: http://doi.wiley.com/10.1111/cen.13611.
Hayashi K, Abe K, Sakata I, Sakaguchi C, Yamamoto K, Kosuda S. [Cost-utility analysis of
antithyroid drug therapy versus 131I therapy for Graves’ disease]. Kaku Igaku [Internet]. 2005 [cited
Feb 1];42:87-95. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16038427.
Donovan PJ, McLeod DSA, Little R, Gordon L. Cost-utility analysis comparing radioactive iodine,
anti-thyroid drugs and total thyroidectomy for primary treatment of Graves’ disease. Eur J Endocrinol
[Internet]. 2016 [cited 2020 Oct 17];175:595-603. Available from: https://pubmed.ncbi.nlm.nih.gov/
/.
Cruz AF Junior, Takahashi MH, Albino CC. Graves’ disease: cost-effectiveness of clinical and
radioiodine treatments. Thyroid[Internet]. 2005 [cited 2020 Oct 17]; 15suppl1: S-201. Available
from: http://www.13itc.org/information.html.
Starling S. Long-term treatment outcomes for Graves disease. Nature Reviews Endocrinology
[Internet]. 2019[cited 2020 Oct 17]; 5: 628. Available from: https://www.nature.com/articles/s41574-
-0268-5.